SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
Table of Contents
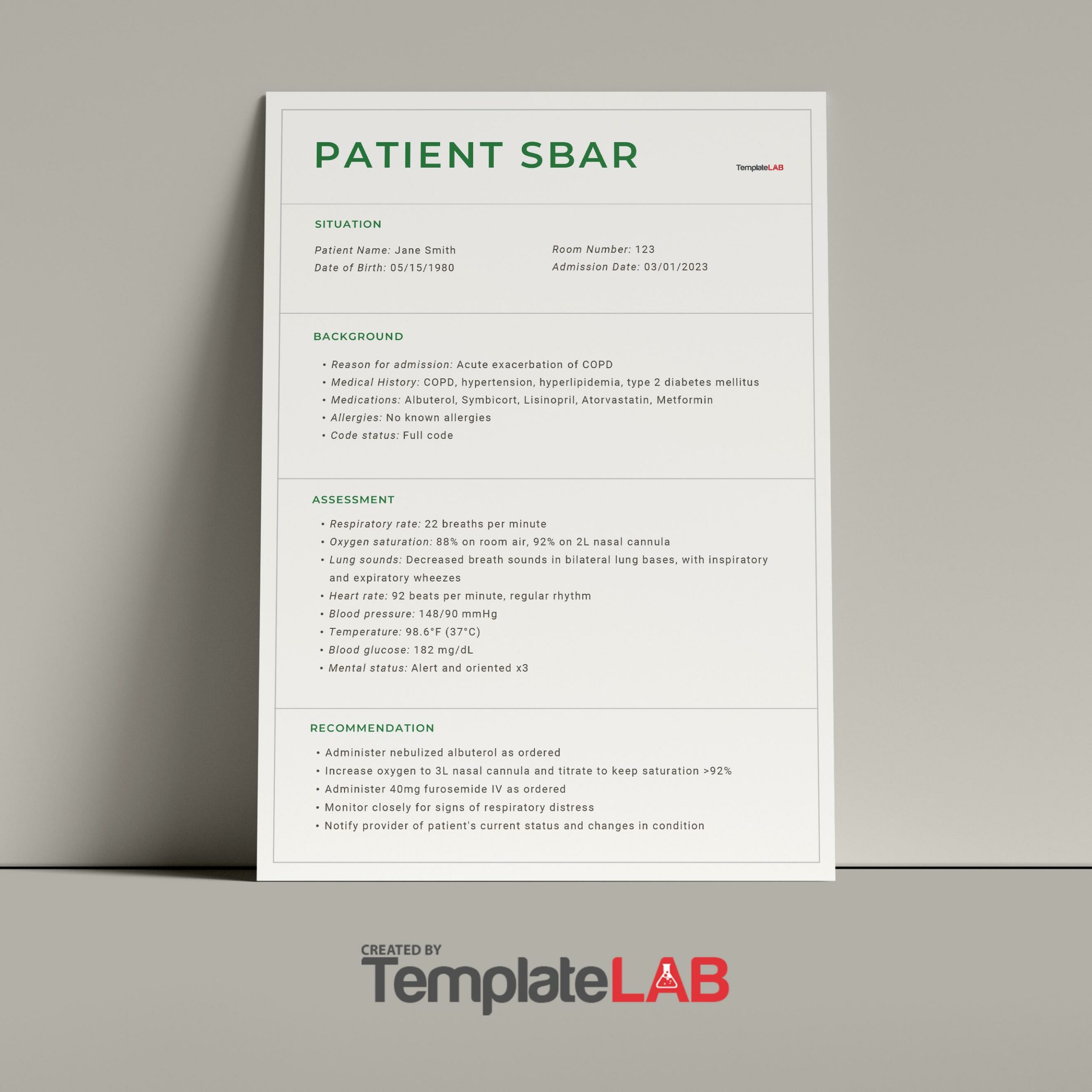
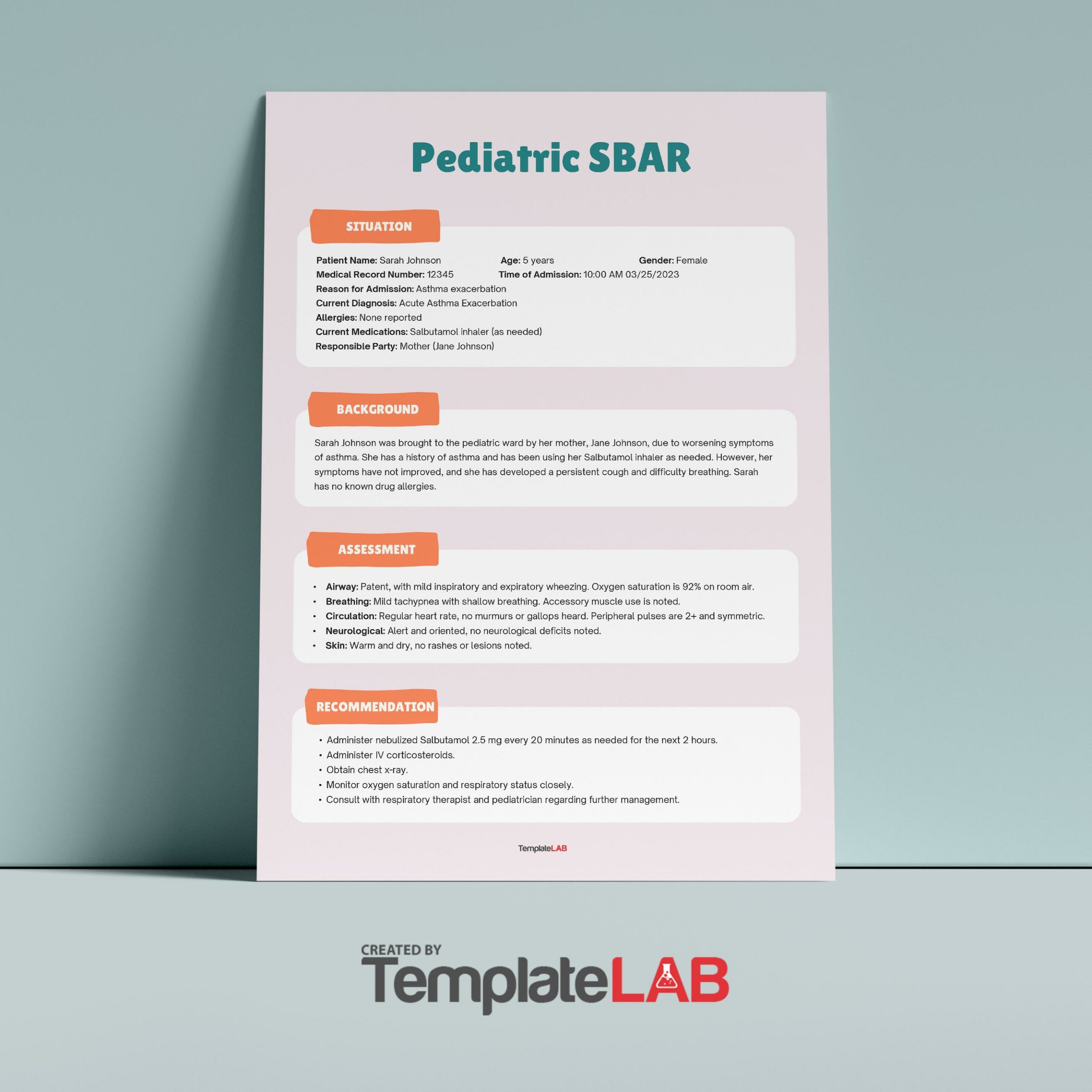
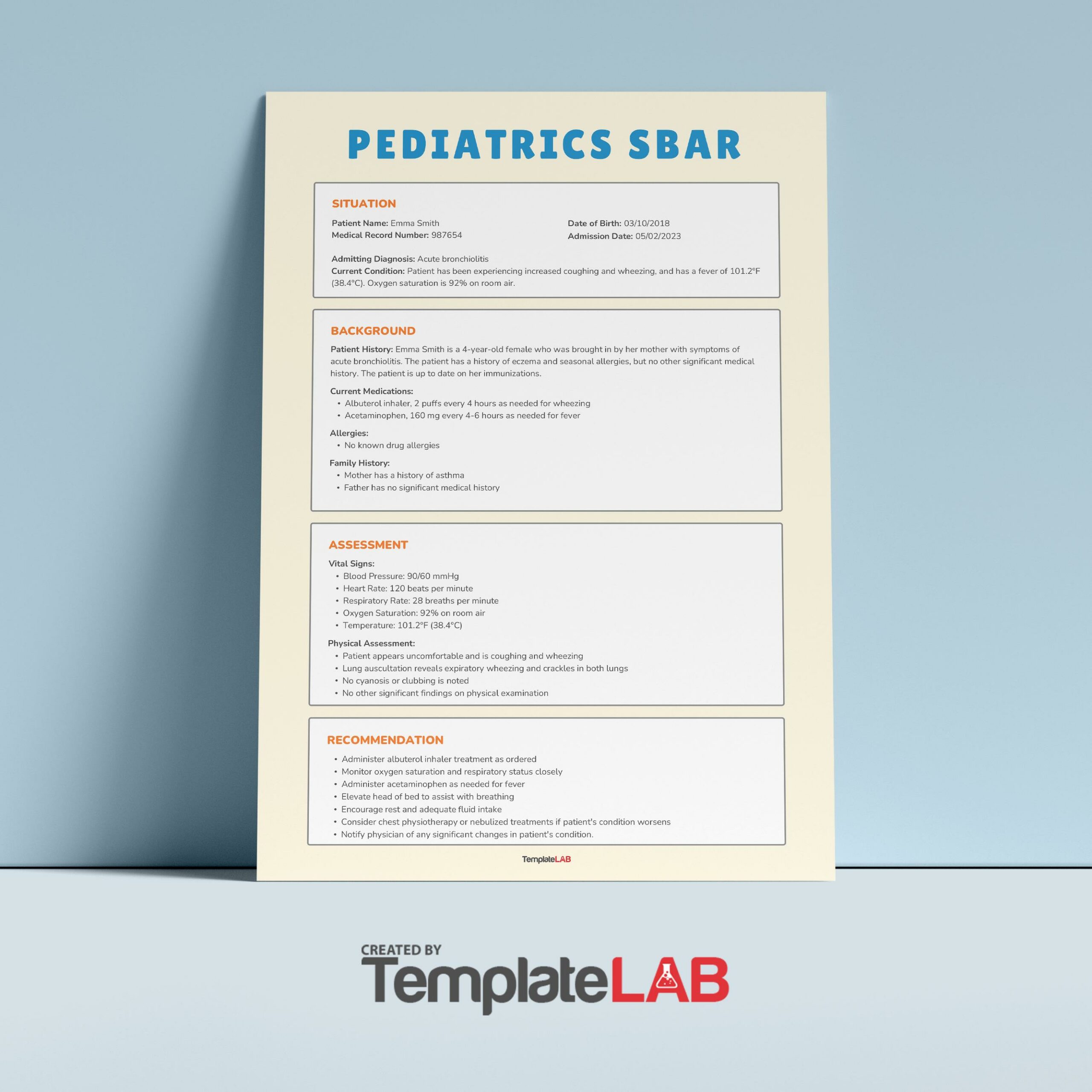
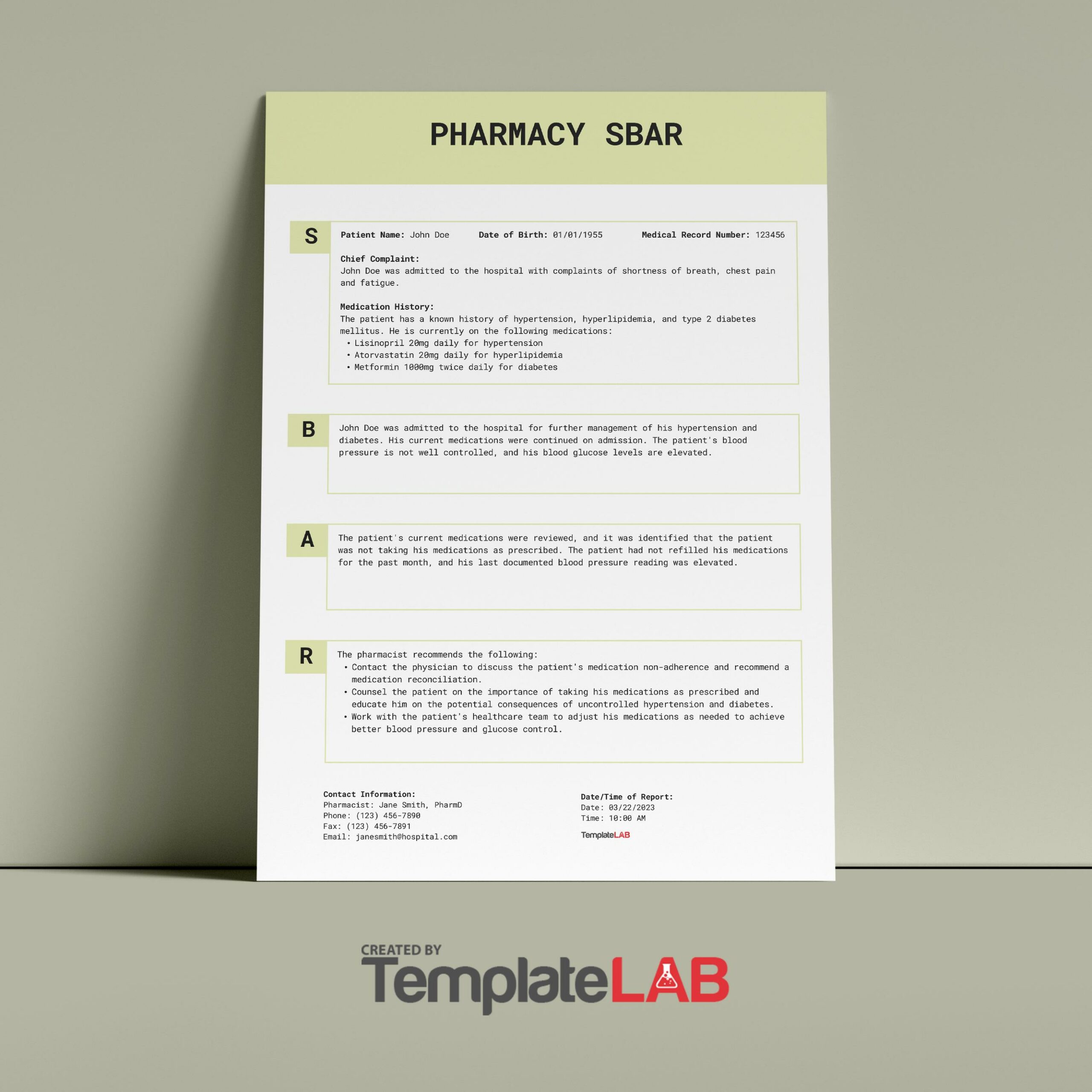
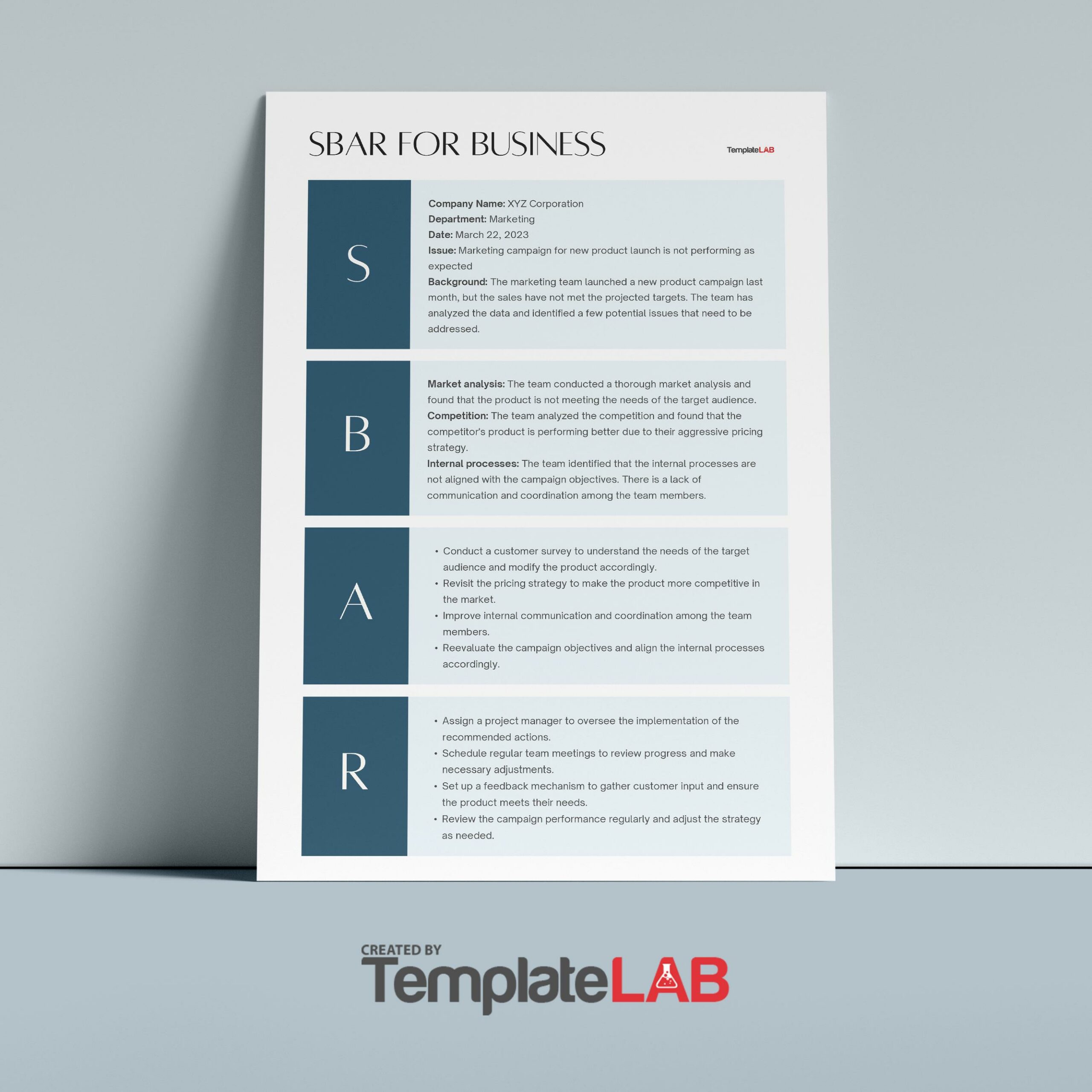
SBAR Templates
What is the SBAR?
The SBAR concept was first developed by the USA Navy as a means of communicating information to nuclear submarines. Because of its success, the SBAR template got introduced to the health care system in the 1990s.
The SBAR technique offers a framework of communication between the members of a healthcare team regarding the condition of a patient. With an acronym that’s easy to remember, SBAR nursing is a concrete tool that can be very useful in framing conversations that require immediate attention or action, especially if they are about patients with critical status.
It allows for a more focused and easier way to set expectations for what kind of data to communicate and how between the members of the health team. This is essential for the development of teamwork and encouraging a culture of patient safety.
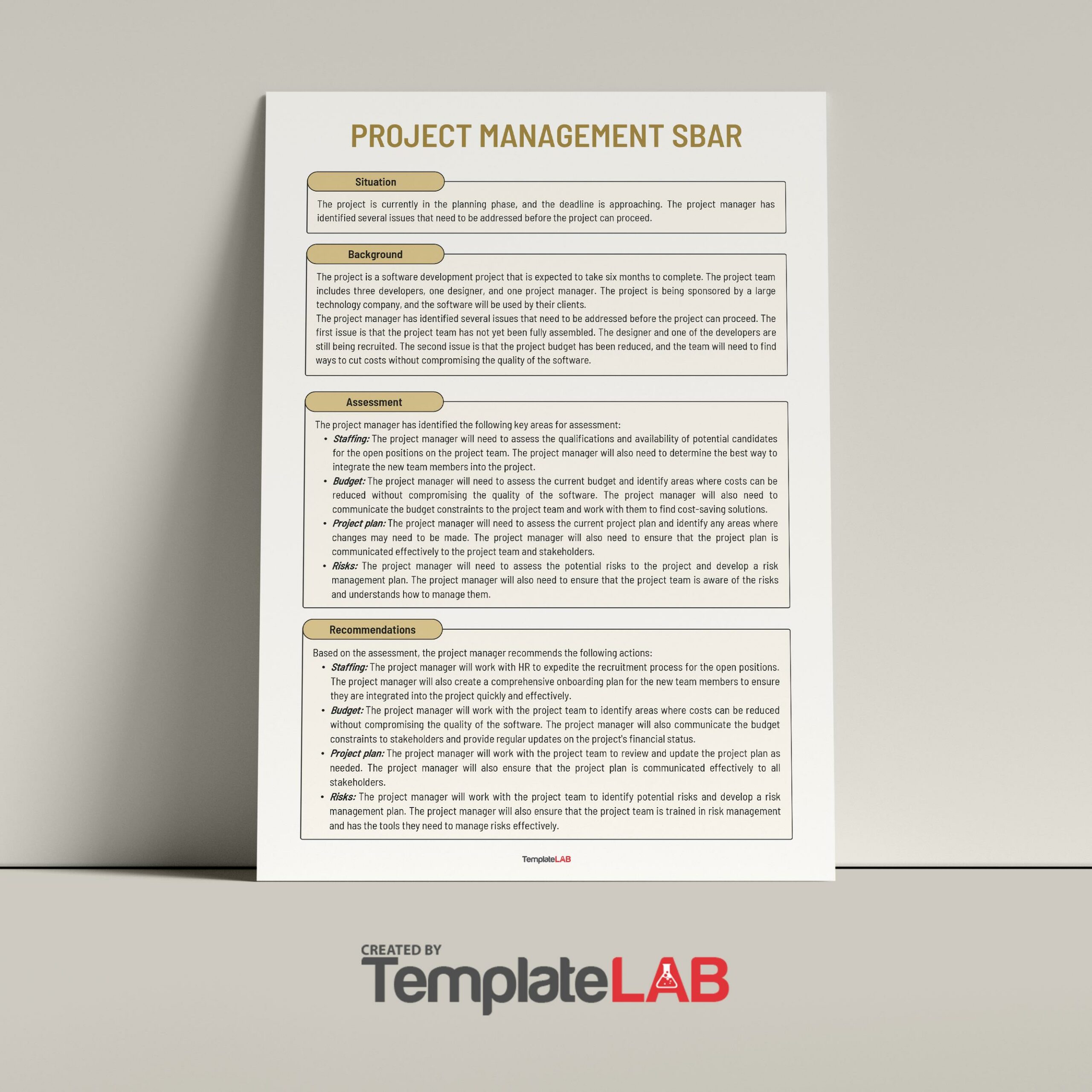
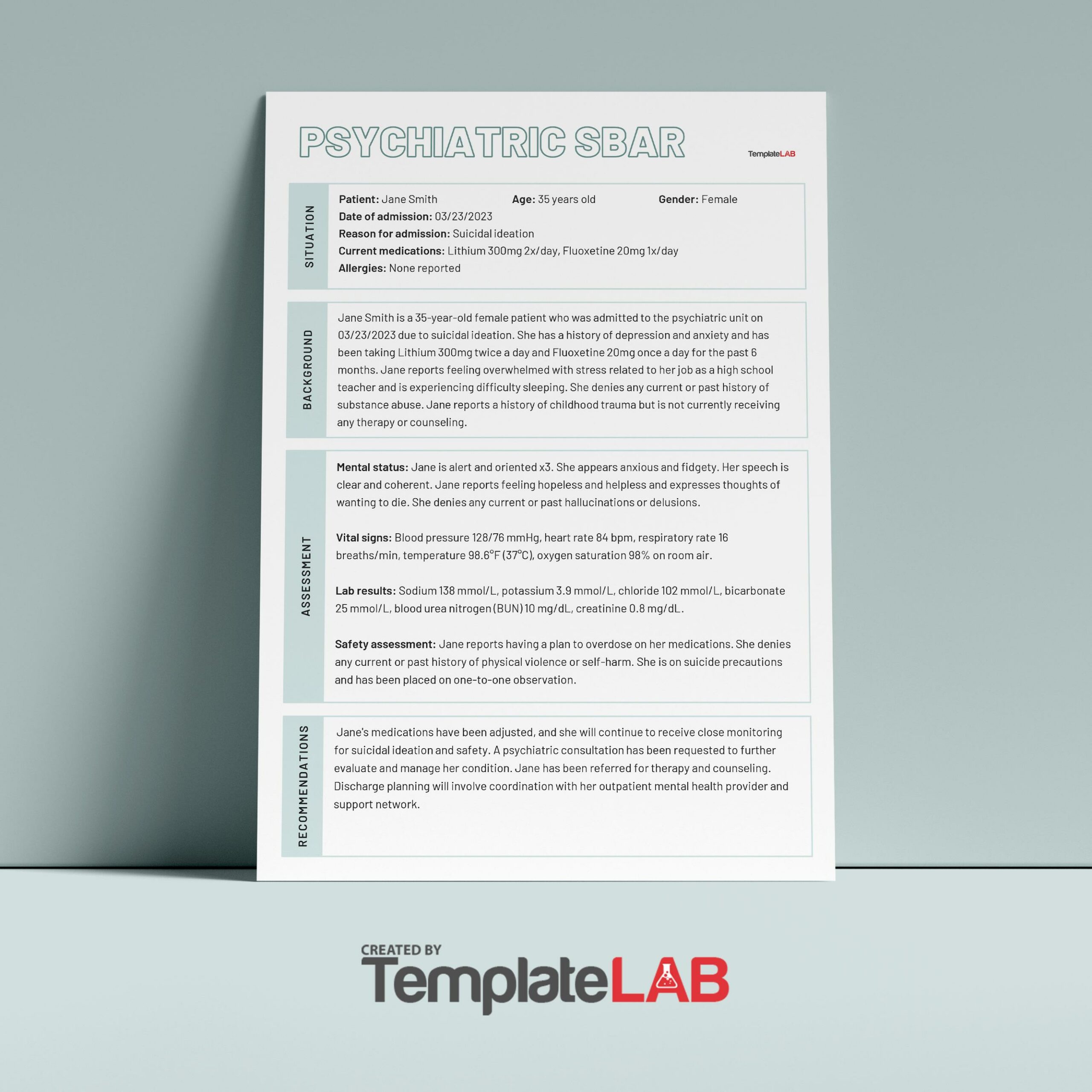
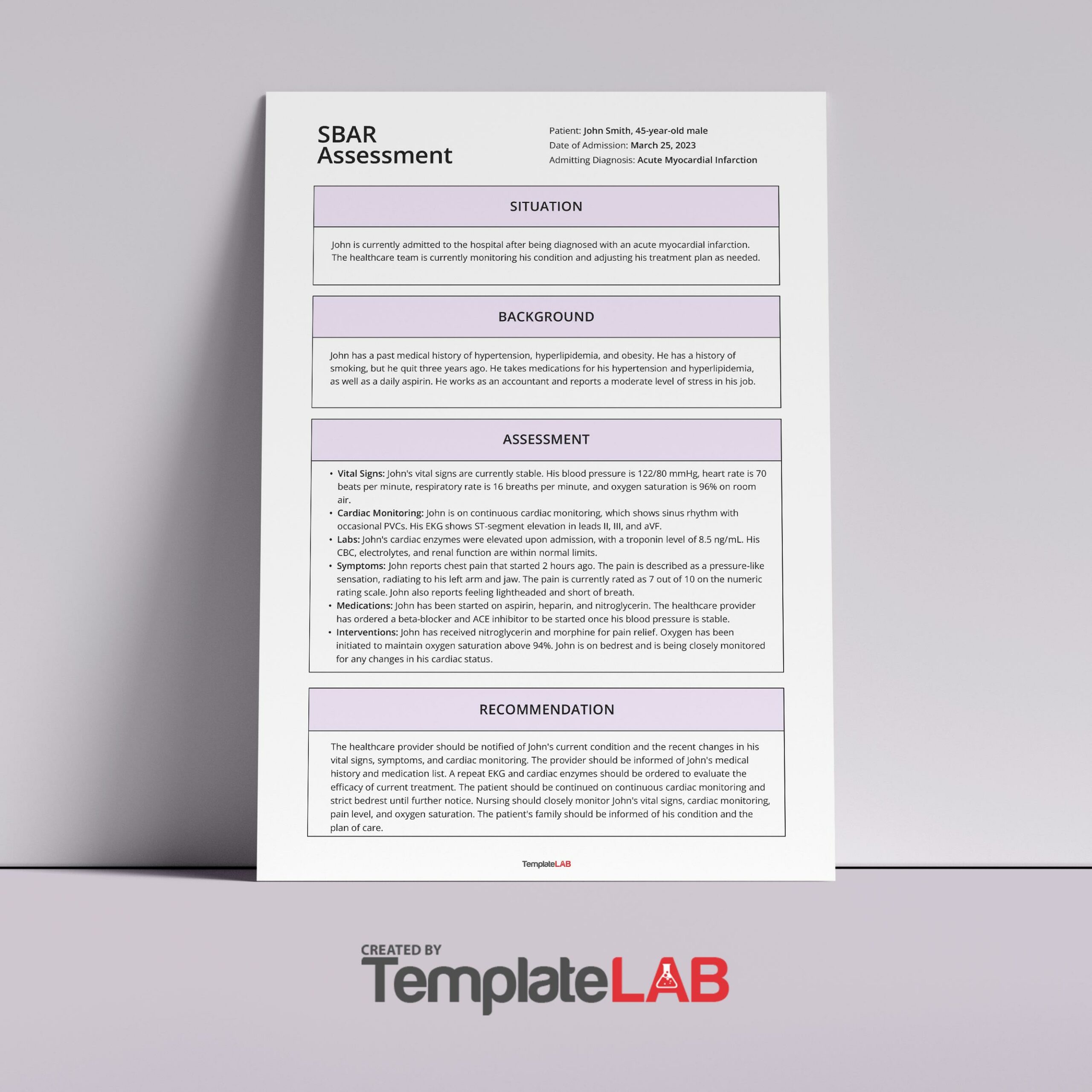
SBAR Examples
Is SBAR evidence-based?
In medical practice, there can be different approaches to communicate and this includes shift-reporting in a room, by phone, at the nurse’s station, or at a patient’s bedside. Most of the literature involved in these approaches indicates that there is a need for a standardized communication method.
One such technique is the use of an SBAR tool template as this provides a framework for effective communication. As a result, it can help you create an environment that allows people to express their concerns by speaking up. Such actions can reduce the risks of adverse events and foster a safer culture in the hospital.
An excellent way to prevent negative outcomes for patients while strengthening teamwork in healthcare is by improving the communication between caregivers. In this aspect, SBAR examples can provide common expectations like what needs communication, how to structure communication, and what the required elements are.
Moreover, an SBAR template also provides ways to hand-off important information in the presence of the patient, thus, allowing the patient’s active participation in your care. As it should be, the patient is always central to all of the information surrounding care activities.
They can add information or ask questions during the discussion. With this method, the patient can see how you and the other staff members work as a team. This gives them the assurance that everyone involved knows and agrees on the plan of care.
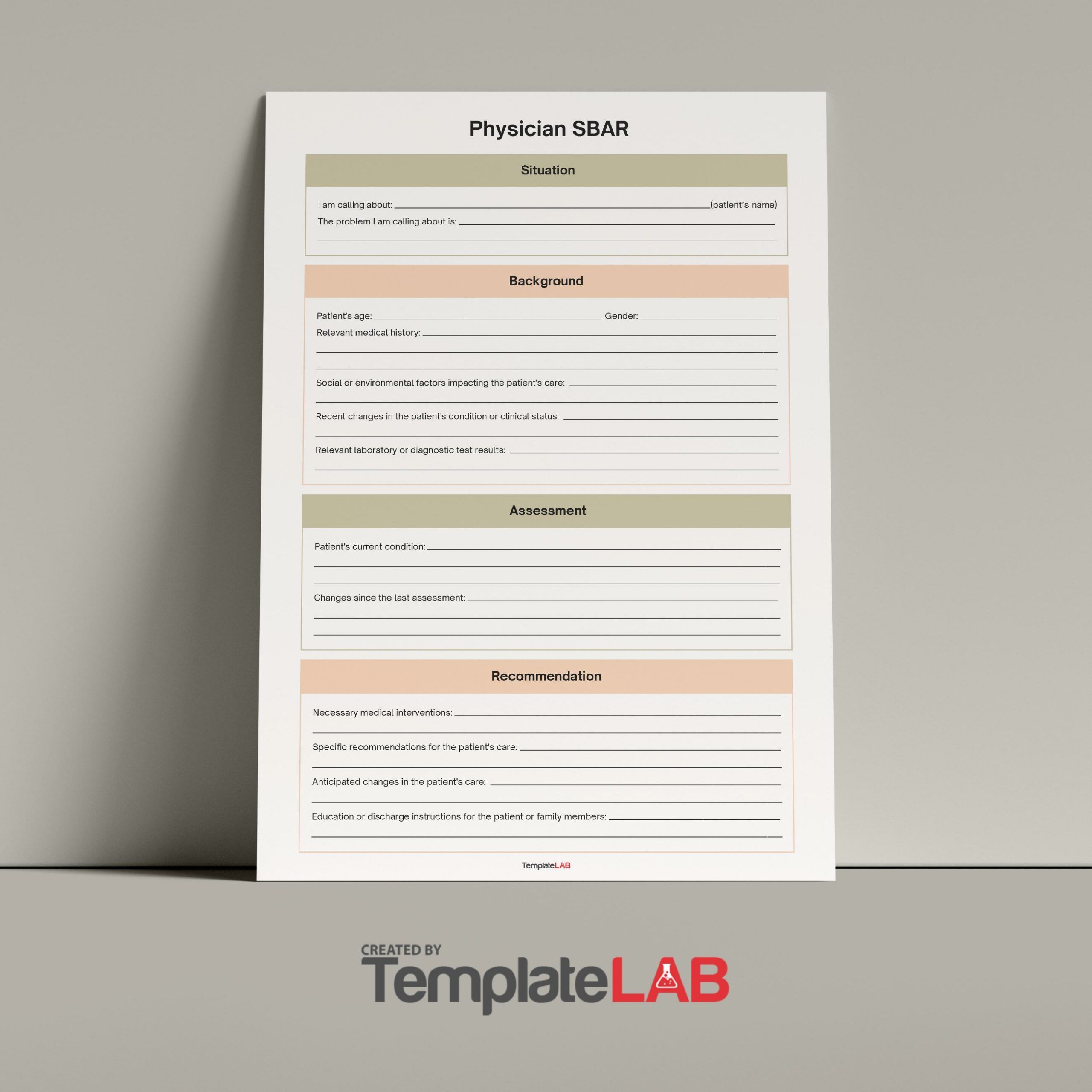
SBAR Communication Templates
What to include?
You can use the SBAR nursing document to communicate any non-urgent and urgent patient information to other healthcare professionals like therapists and doctors. SBAR examples are typically used for:
- Conversations with physical therapists, physicians, and other medical professionals.
- In-person discussions and those done over the phone.
- Handoff communications or shift changes.
- When trying to resolve an issue with a patient.
- Daily safety briefings.
- When bringing up a concern.
- When calling an emergency response team.
The SBAR template is a useful tool in communicating and organizing information. Although the SBAR could get subjected to existing communication barriers and time constraints as obstacles to it, this document still improves the quality of communications. If you plan to make your own template, include the following:
- Pre-SBAR
Before you can initiate an SBAR, there are a few things you should do first:
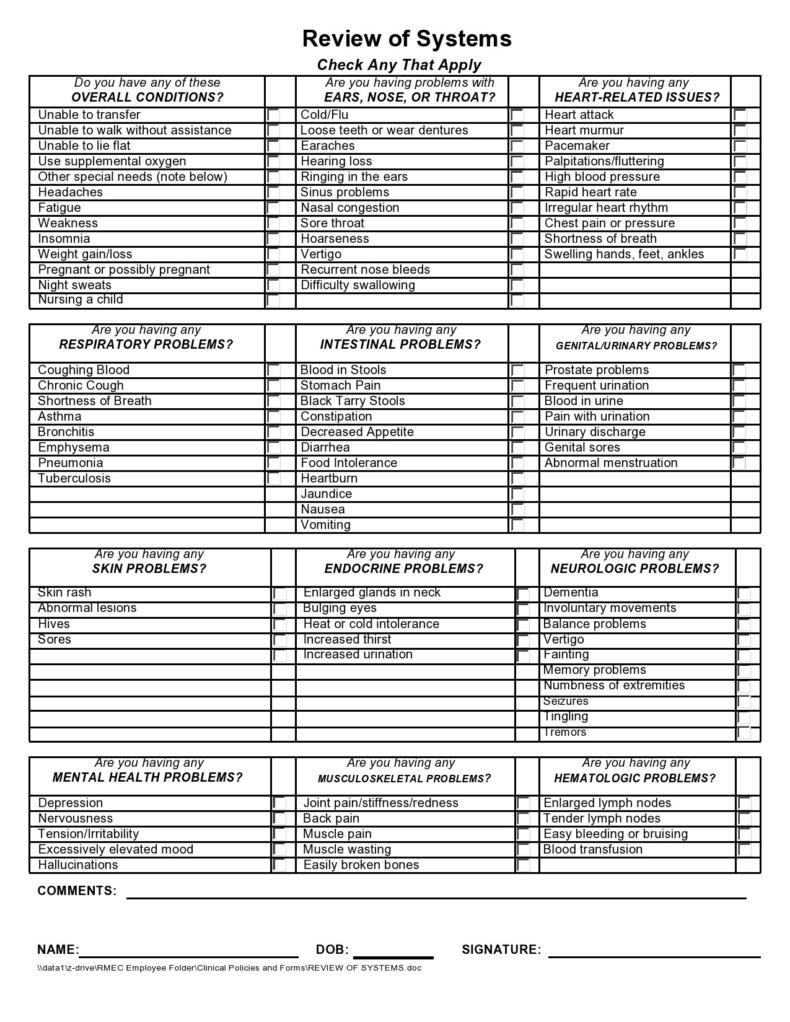
You should perform a comprehensive assessment of the patient.
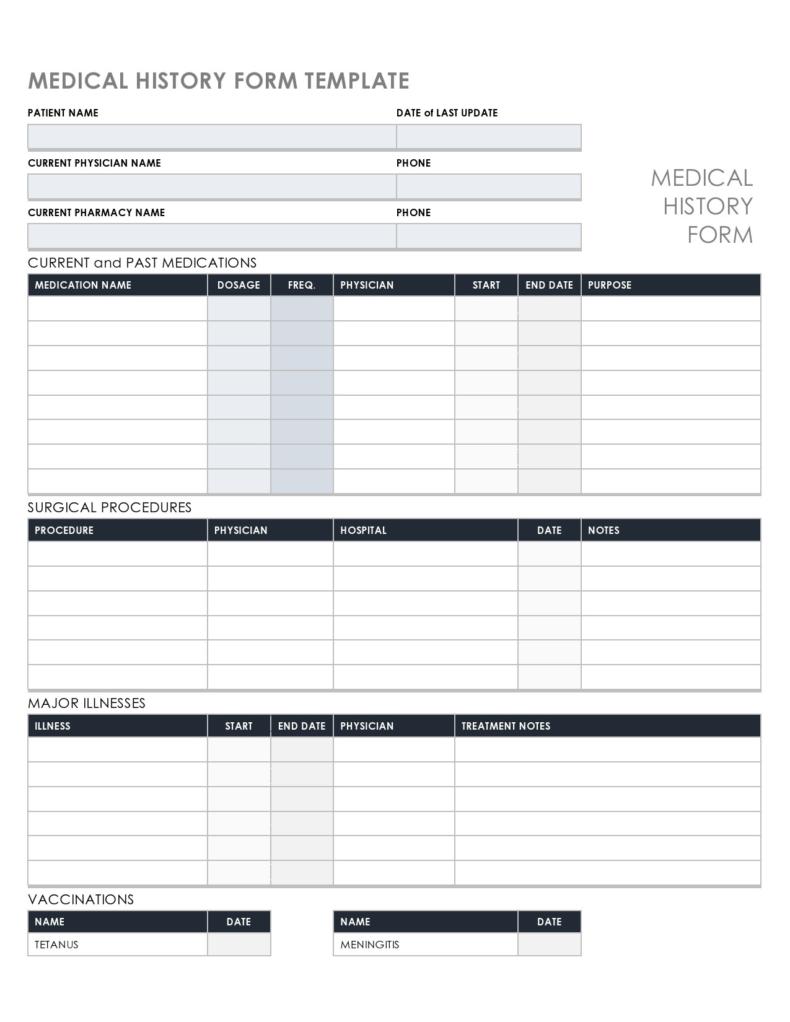
You should have the patient’s on-hand along with a list of their existing allergies, IV fluids, labs, and medications.
Complete all of the patient’s vital signs.
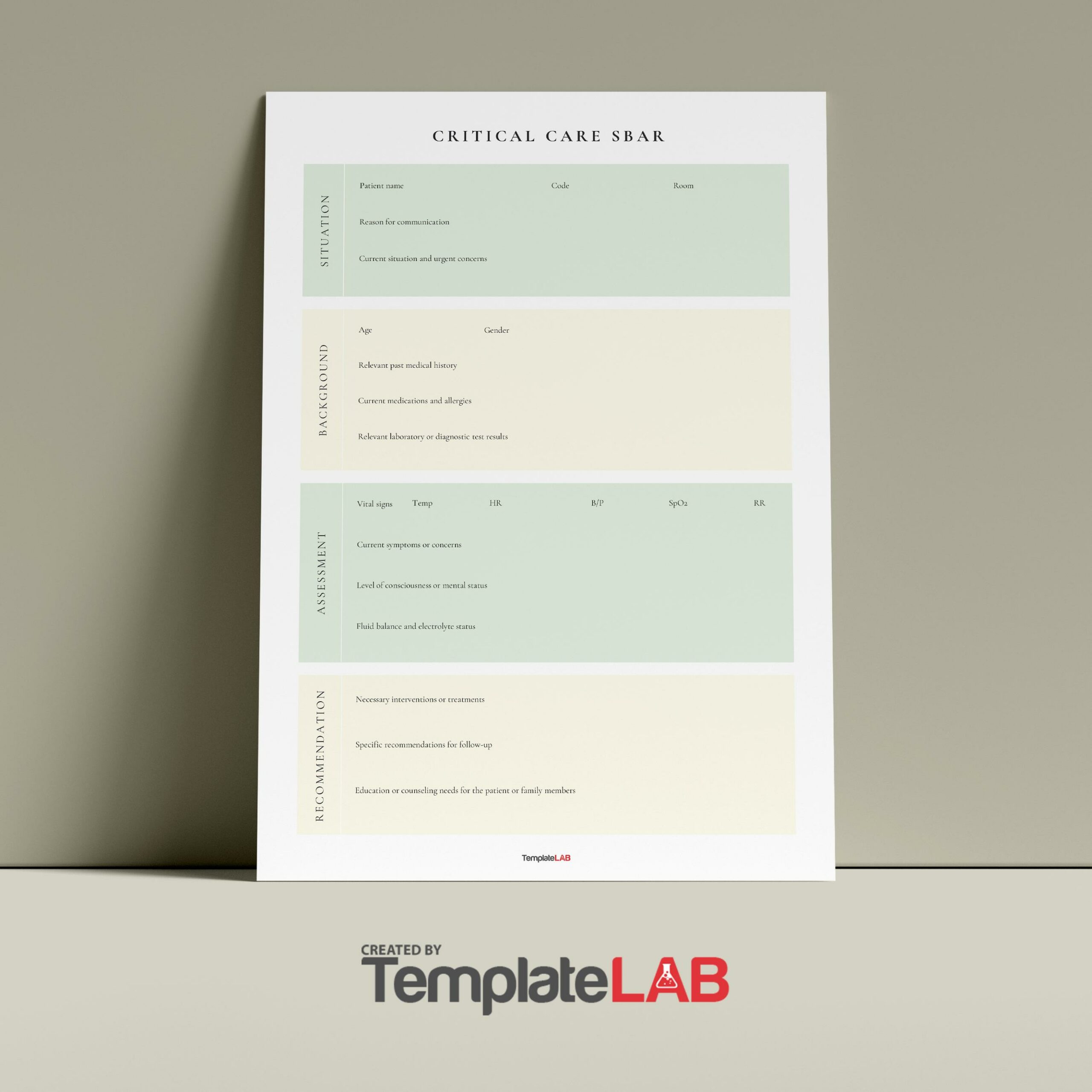
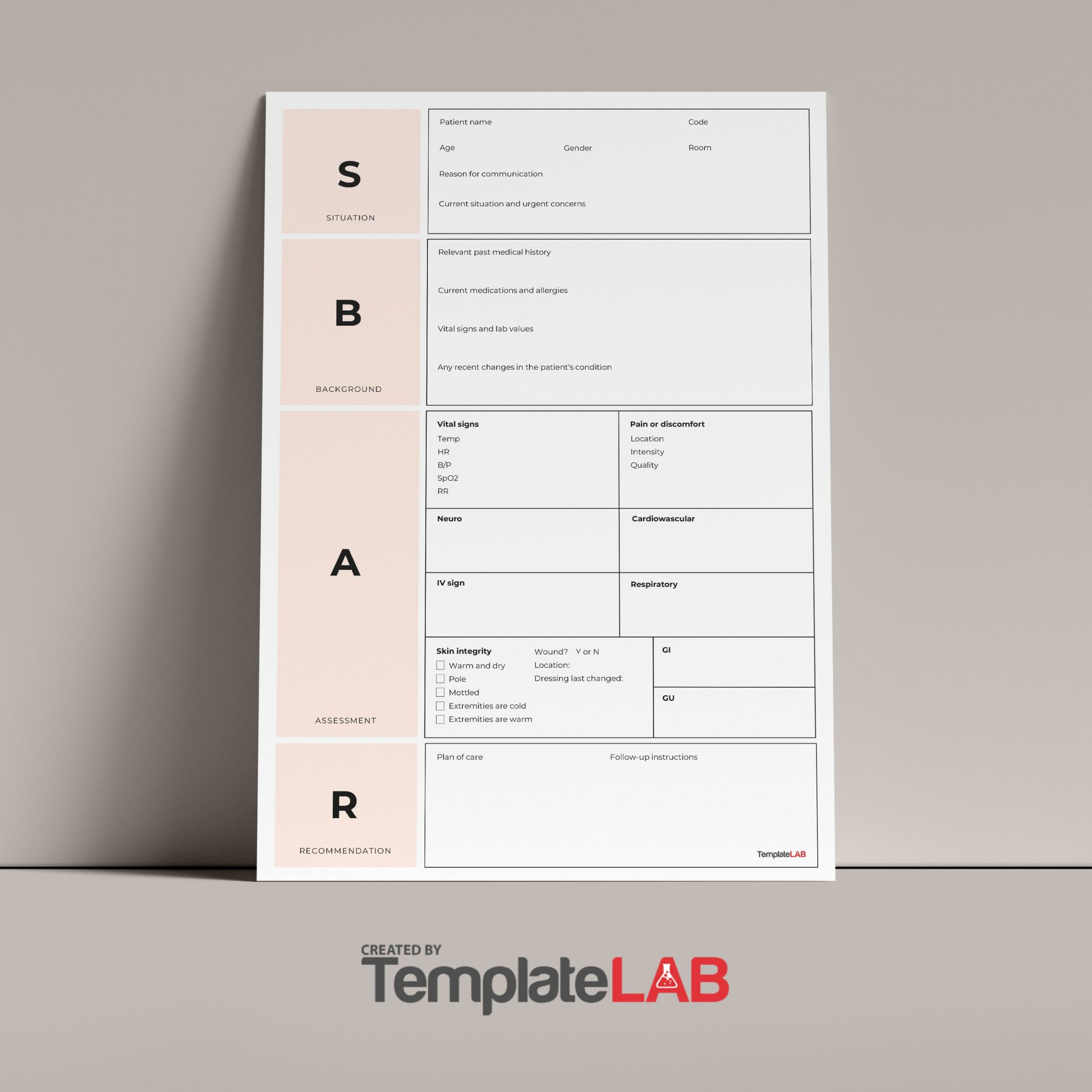
Identify the patient’s code status and report it. - Situation
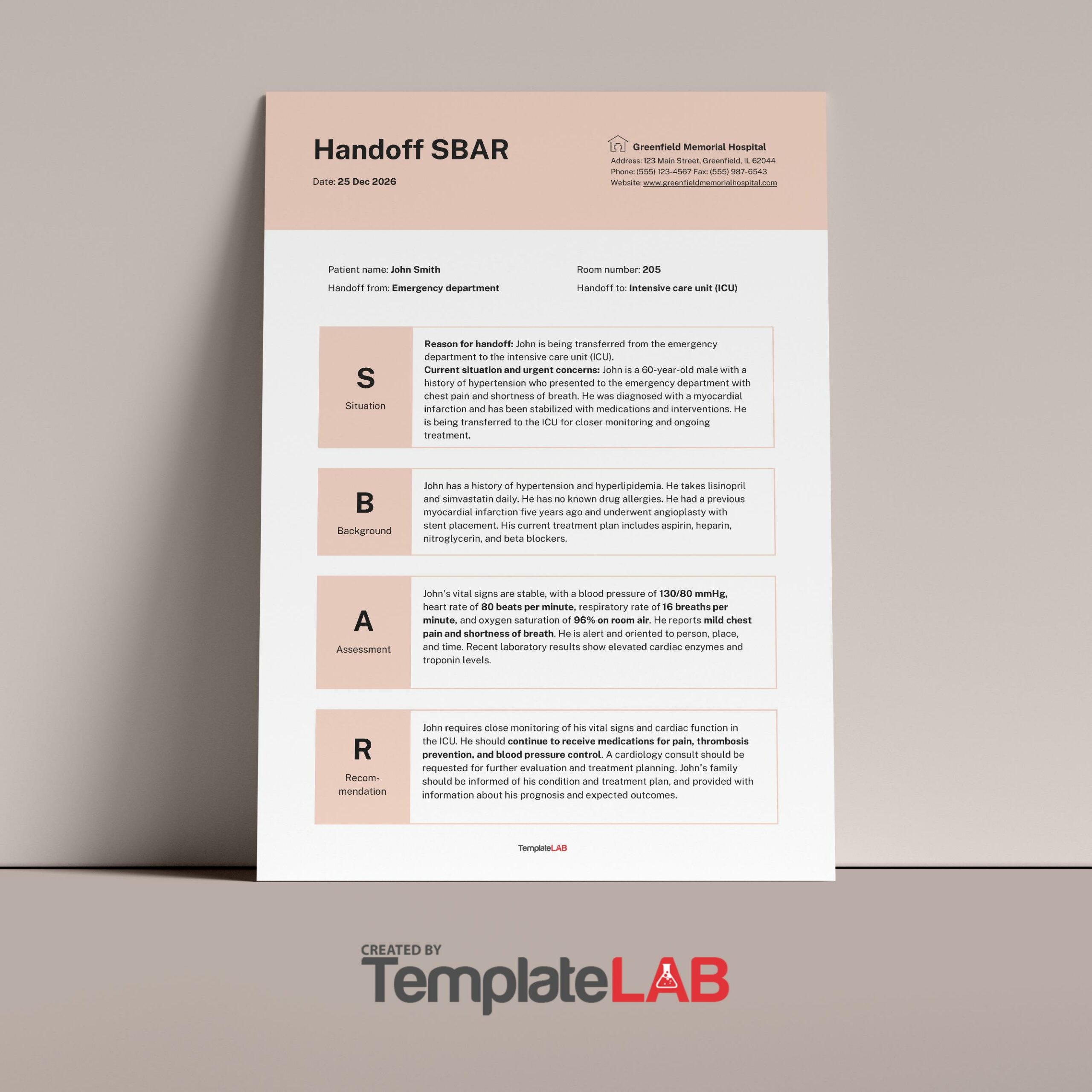
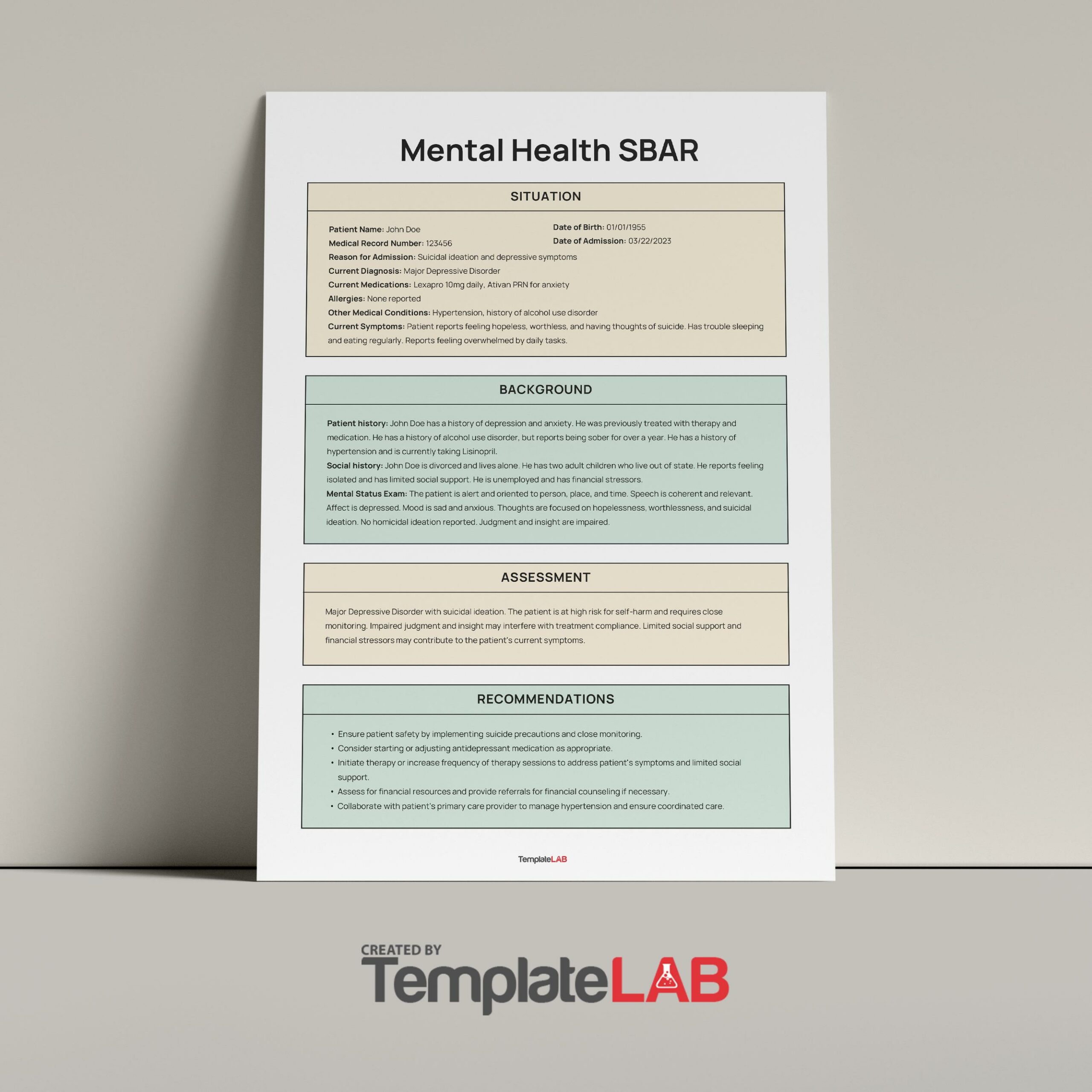
This is a short and clear description of the current situation of the patient. You should mention what’s happening with the patient at the present moment. If you’re giving a shift report to the next nurse, indicate the name of the patient, the reason why the patient is on the unit, and introduce the next nurse to the patient. - Background
You must provide relevant and clear background information about the patient. Give the next caregiver background information that’s specific to the relevant history of the patient. This part sets the context for what you will discuss and this may include the diagnosis of the patient, history of any treatment or procedures done, and family history. - Assessment
This section states your professional conclusion that you based on the patient’s background and current situation. In other words, you will report the patient’s current condition. - Recommendation
Inform the individual you’re communicating with what you need from them. State what you think would be the best response to the patient’s care for the day. You may suggest things like:
Initiating discharge planning by discussing the patient’s need.
Contacting the physician about the discharge plans.
Conveying to the rest of the healthcare team what they need to do before discharge.
You will appreciate the benefits of effective communication with your coworkers as you continue to use this method. These benefits include:
- The next nurse’s ability to visualize patients right away and prioritize their care.
- Demonstrating equipment use and sharing information related to the needs of individual patients.
- Promoting accountability between shifts by immediate visualization of patient needs.
- Improvement of staff relationships because communication between shifts happens face-to-face. This decreases blame and builds teamwork.
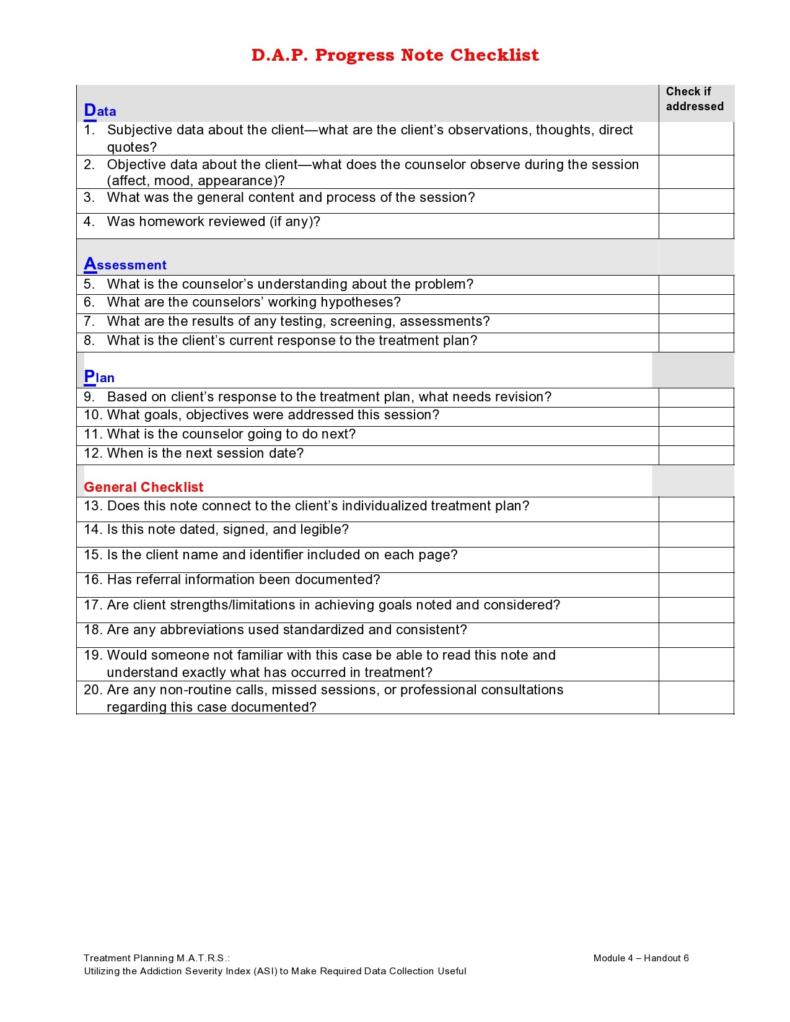
How do you write a good SBAR?
The use of an SBAR communication template provides you with an easy-to-remember concrete mechanism that proves useful for the framing of any conversation, especially the critical ones that require the immediate attention or action of a clinician.
Without an SBAR template, poor communications might cause a number of issues. When writing an SBAR, consider its elements:
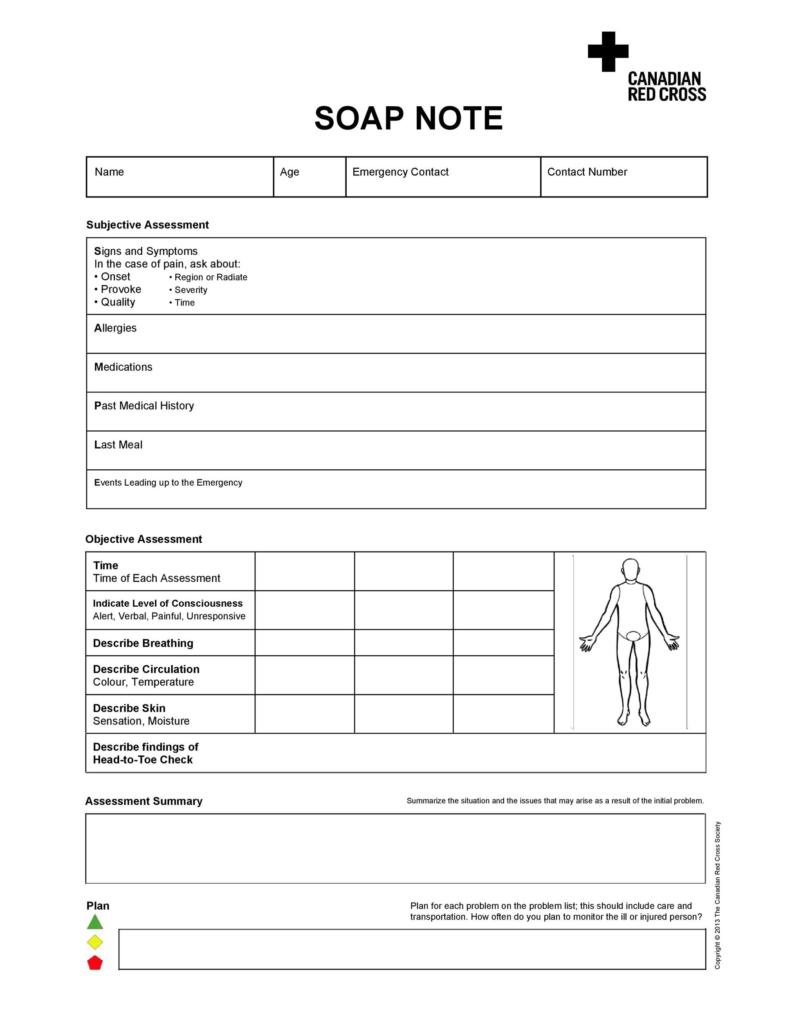
- Situation
This poses the question, “What’s going on with the patient?” or “What’s the situation you’re calling about?” The situation includes information about the patient, vitals, code status, and your concerns as the nurse. - Background
This poses the question, “What is the key clinical context or background?” Relevant background information related to the situation may include:
The admitting diagnosis
The date of admission
The list of current allergies, IV fluids, labs, and medications
The most recent vital signs
The lab results with the time and date of the tests and the results of previous tests (for comparison)
Code status
Other relevant clinical information - Assessment
This poses the question, “What do you think the problem is?” or “What is your assessment of the patient’s situation?” In this section, you indicate what you believe is the problem, based on the history and current assessment of the patient. - Recommendation
This poses the question, “What do you recommend” or “What do you want you to do?” You may suggest a physician’s actions which might include tests. Here are some examples of recommendations:
Patient needs to be seen now
Notification of the patient’s admission
Order change
Effective s it is, the SBAR tool template doesn’t work on its own. Therefore, you must:
- You need to carefully think through the issue and your approach before speaking to, writing, or calling a physician.
- Think about the information the physician will need then have it ready before they arrive.
- Organize your facts by following the SBAR checklist. Include all relevant data without making the document too long.
- If you’re reluctant to make any recommendations, state that you’re concerned about the situation. An alternative, you can make a simple suggestion to start off a discussion.
Does it have any limitations?
You may encounter SBAR examples in different situations. But it isn’t always effective. Here are some situations where using an SBAR isn’t the best idea:
- When the other person isn’t familiar with the SBAR concept.
- The SBAR is a challenging concept to learn and practice. It requires a thorough understanding of the subject matter along with necessary follow-ups. Aside from this, it also requires a supportive environment. If the rest of the healthcare team isn’t amenable to this process, it won’t work.
- Usually, the “R” in SBAR is the weakest point of nurses. This is because some nurses feel too intimidated to give recommendations to physicians.
- One disadvantage of using the SBAR technique for bedside reporting is when you have to wake the patients up or their families when you start the discussion. Healthcare units and professionals must find a more effective way of doing this should your patient choose not to get awakened or involved in this process.
- One other disadvantage related to bedside charting using this technique is the issue concerning the disclosure of new information or sensitive topics that the patient or their family doesn’t know yet. A possible solution to this involves making plans with other nurses to share sensitive or new information before and after the bedside report.
Although the effective communication that the SBAR technique promotes leaves room for confidential information to get disclosed when doctors and nurses have discussions with patients, this might cause patients to have negative opinions about their participation in the process. Ultimately this might interfere with the use of the communication tool.