Healthcare providers in the USA use a technique called Review of Systems (ROS) for obtaining the medical history of patients. This technique involves the use of a review of systems template and it’s often formatted as an element of an admission note that covers specific organ systems. It focuses on the subjective symptoms based on patients’ perceptions.
Table of Contents
- 1 Review of Systems Templates
- 2 What is a complete review of systems?
- 3 Review Of Systems Examples
- 4 The importance of a review of systems template
- 5 Review Of Systems Questions
- 6 What is included in the review of systems?
- 7 Review Of Systems Checklist
- 8 Applying a review of systems template
- 9 Review Of Systems Cheat Sheets
- 10 The difference between a review of systems and a history of present illness
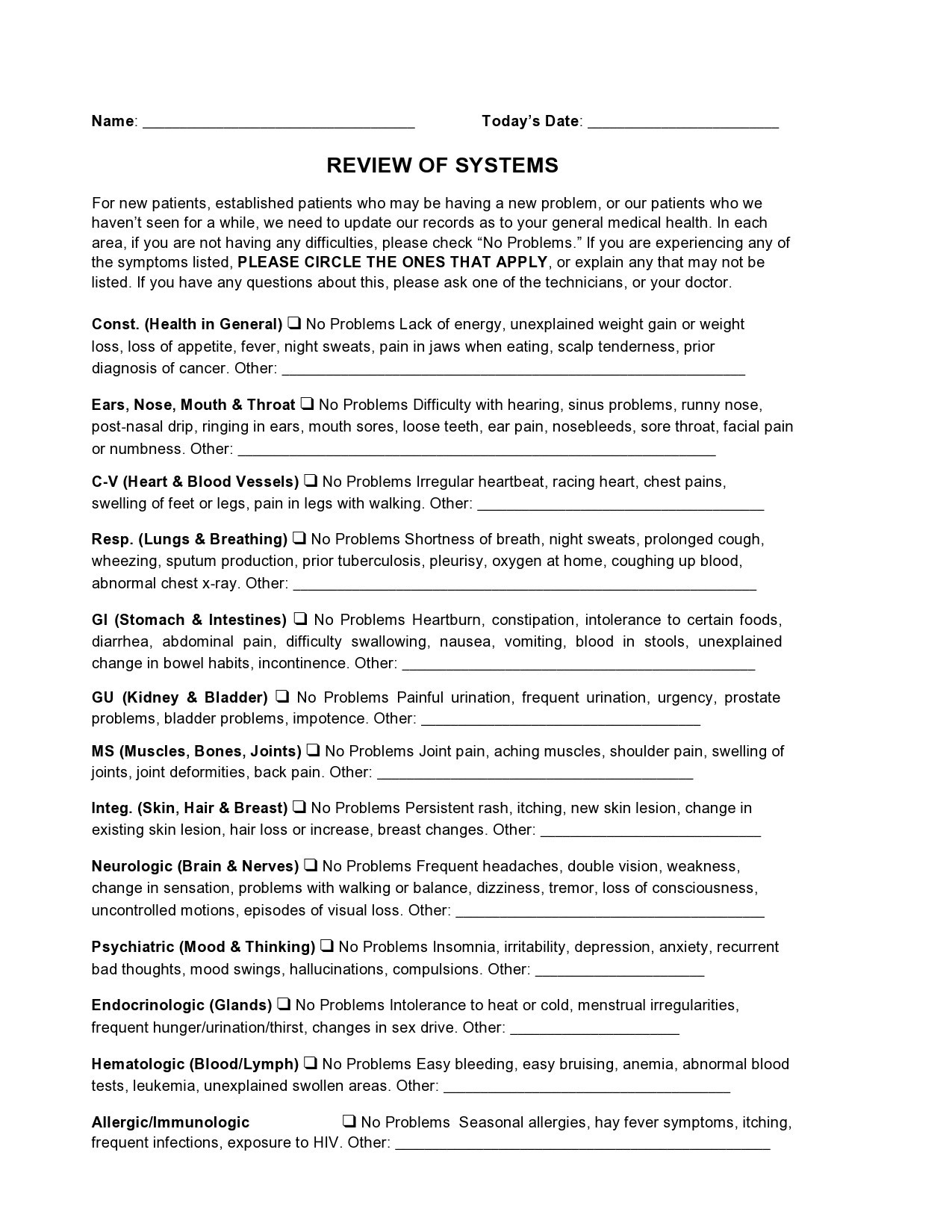
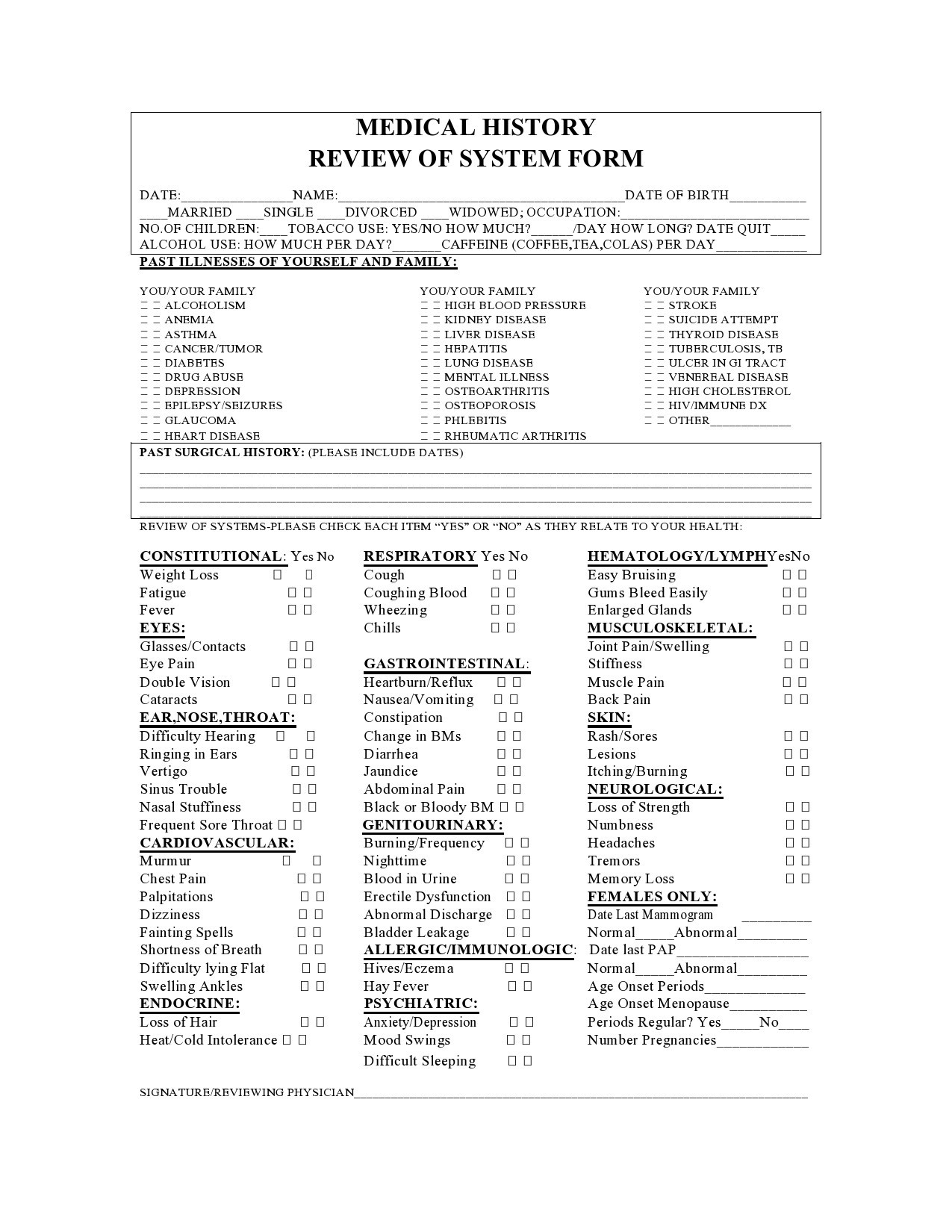
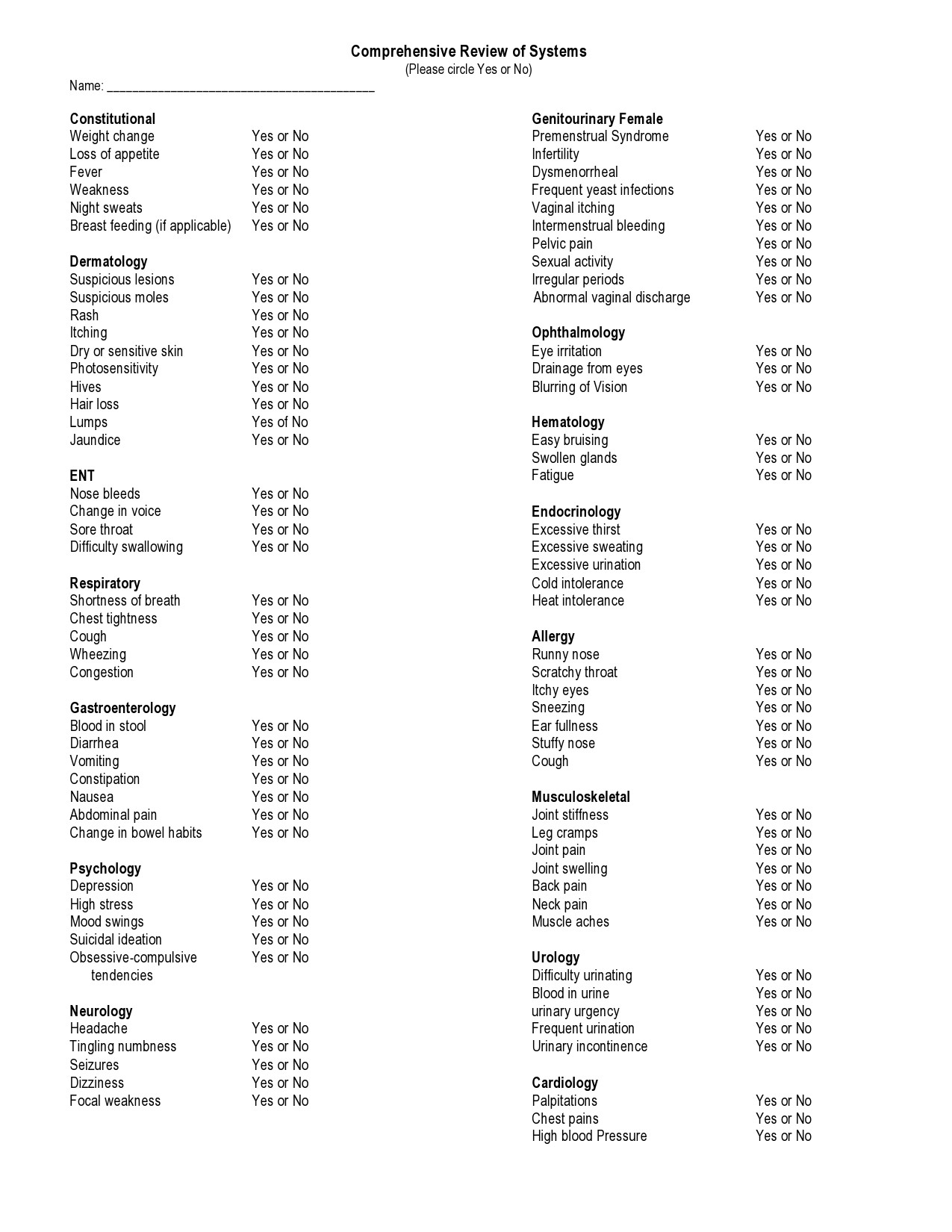
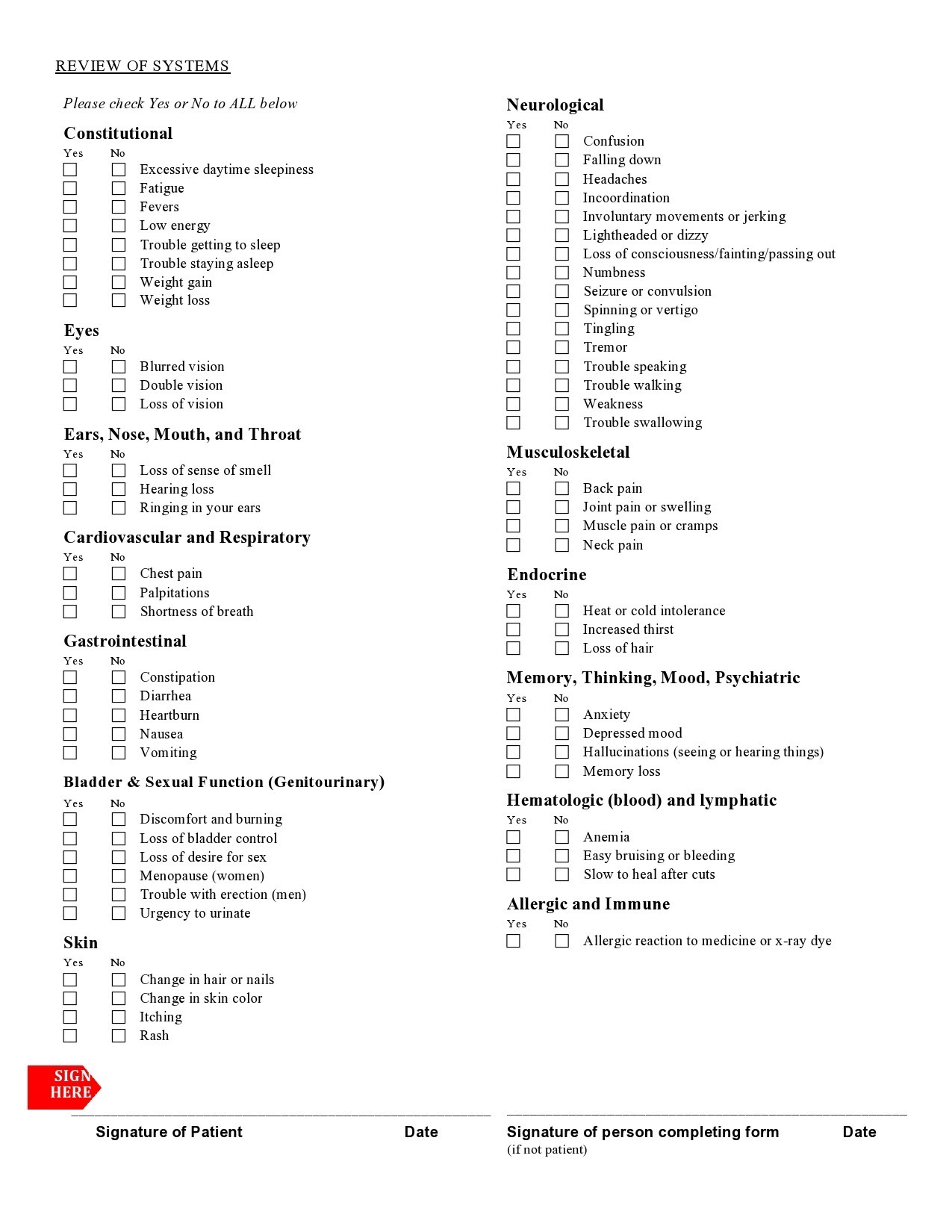
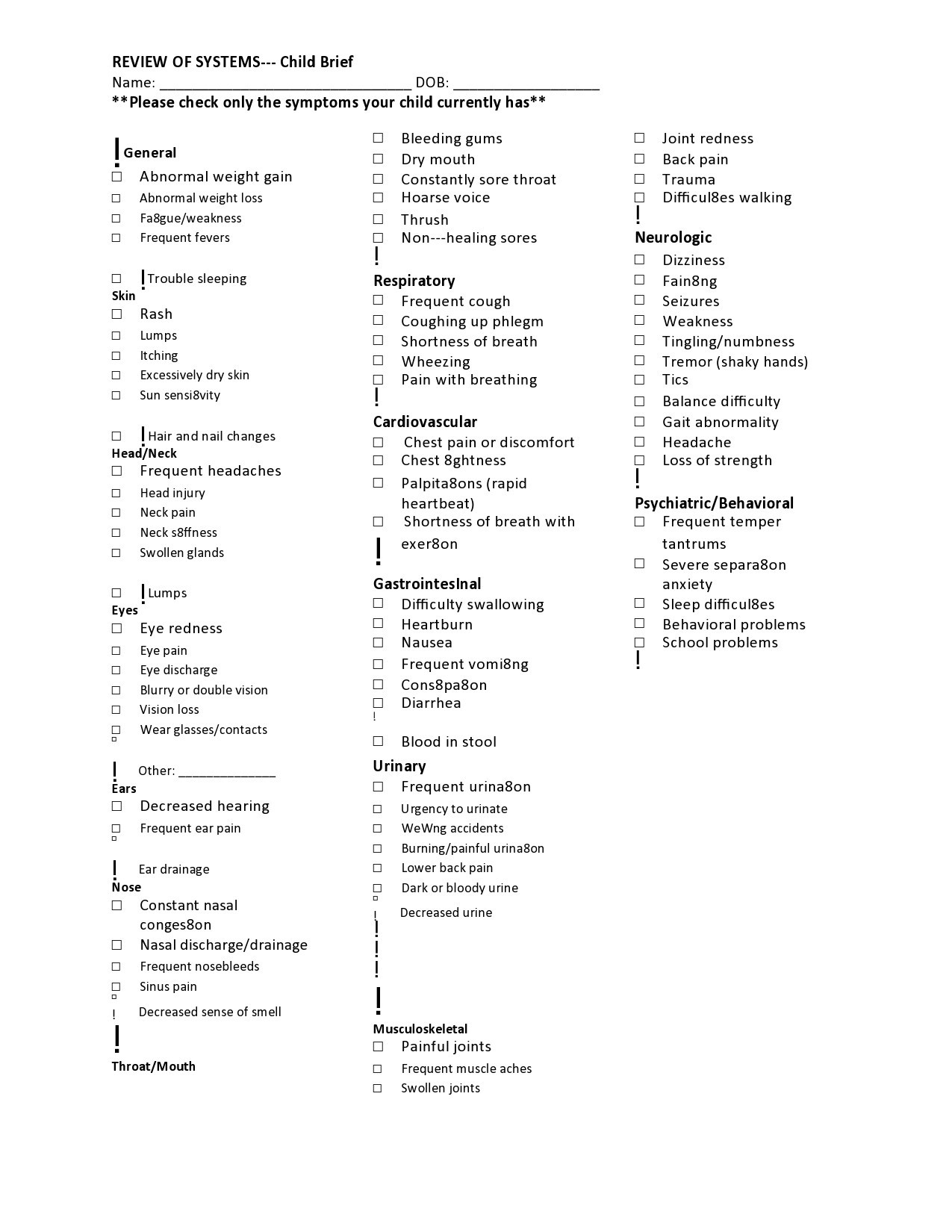
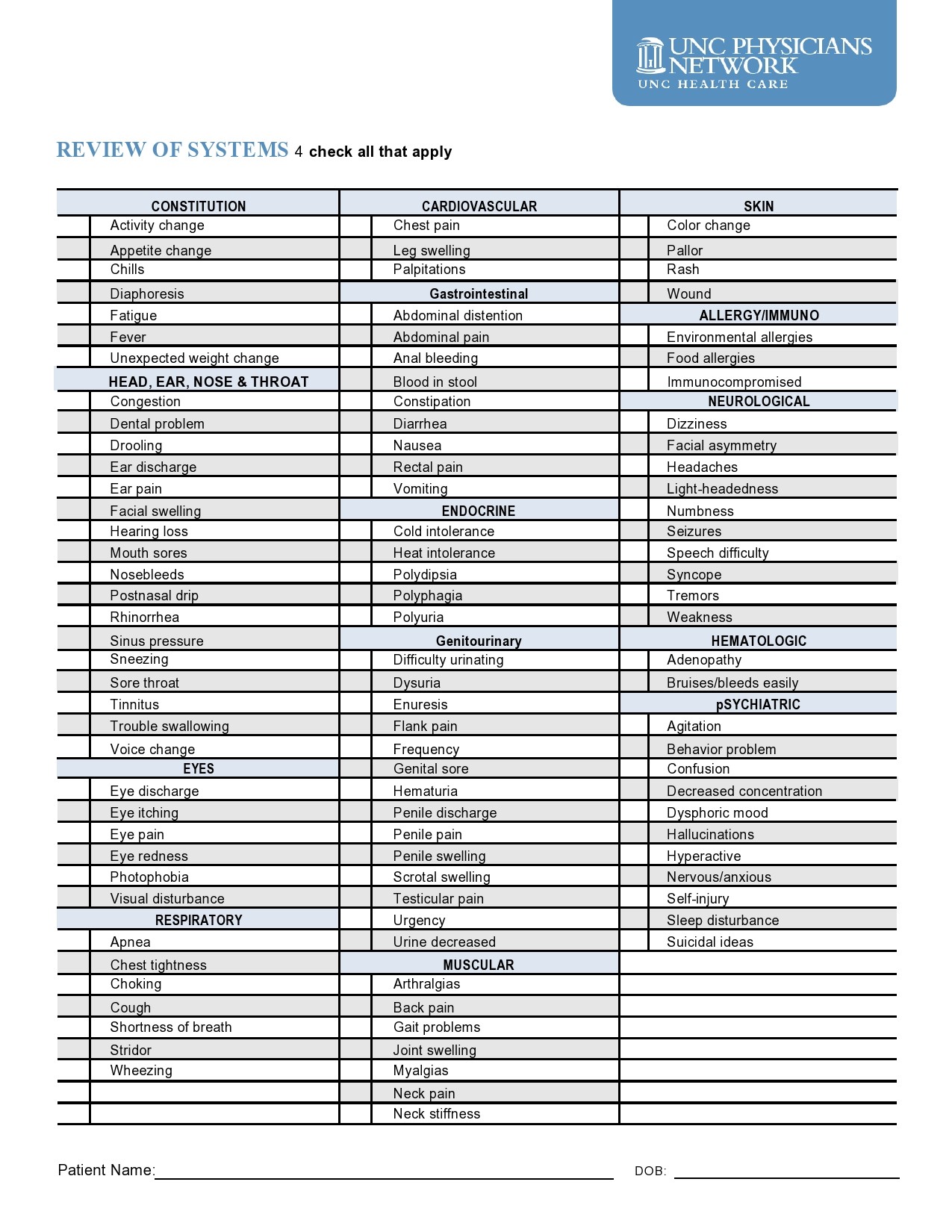
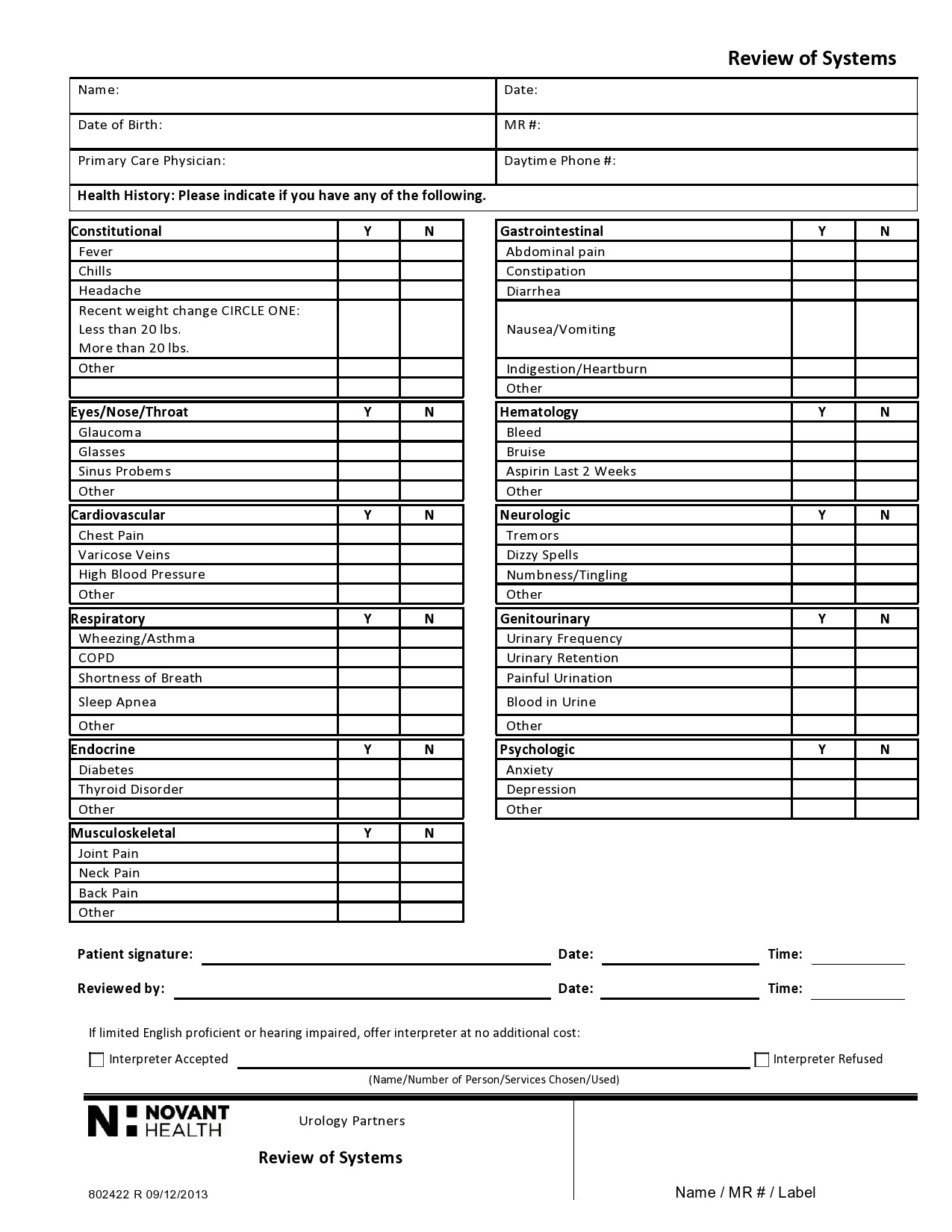
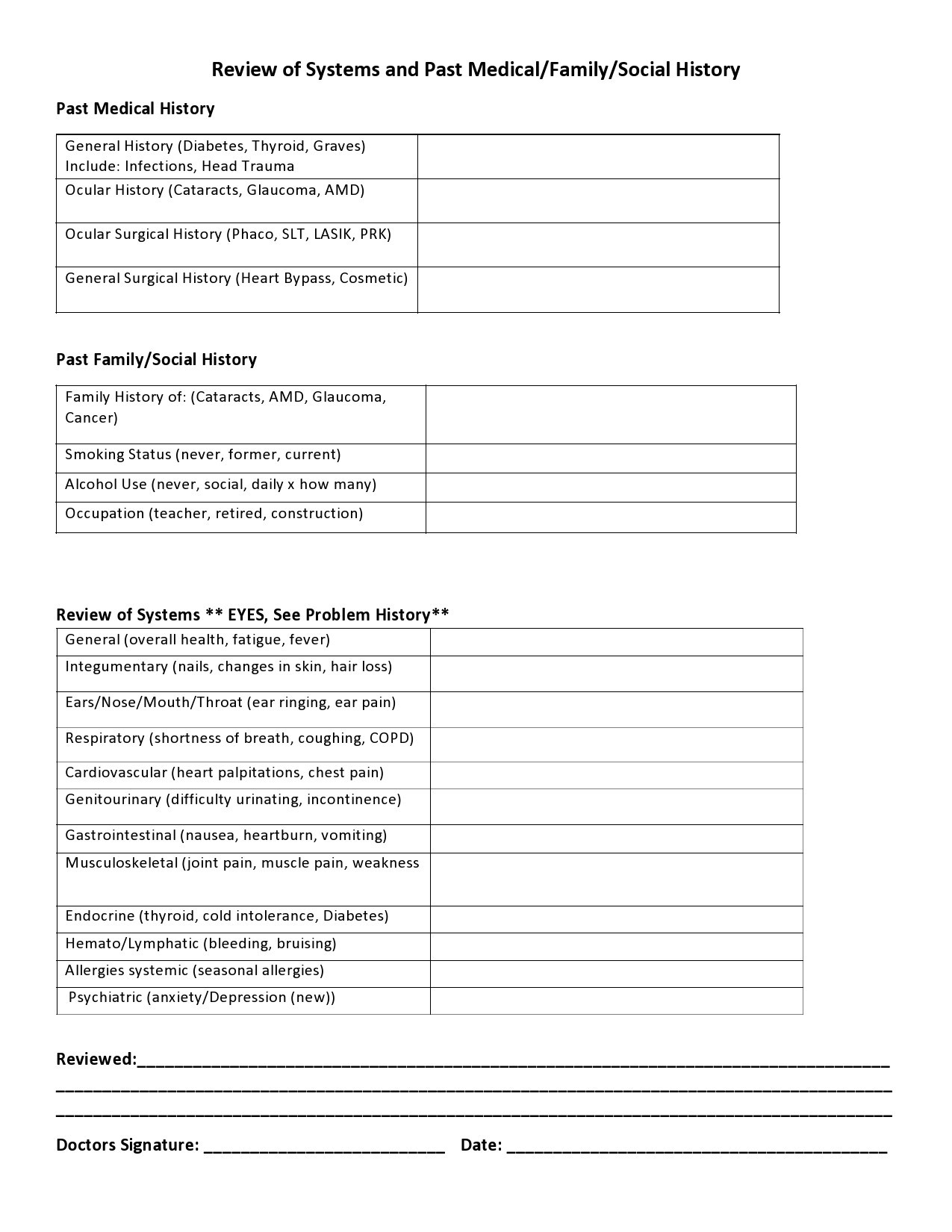
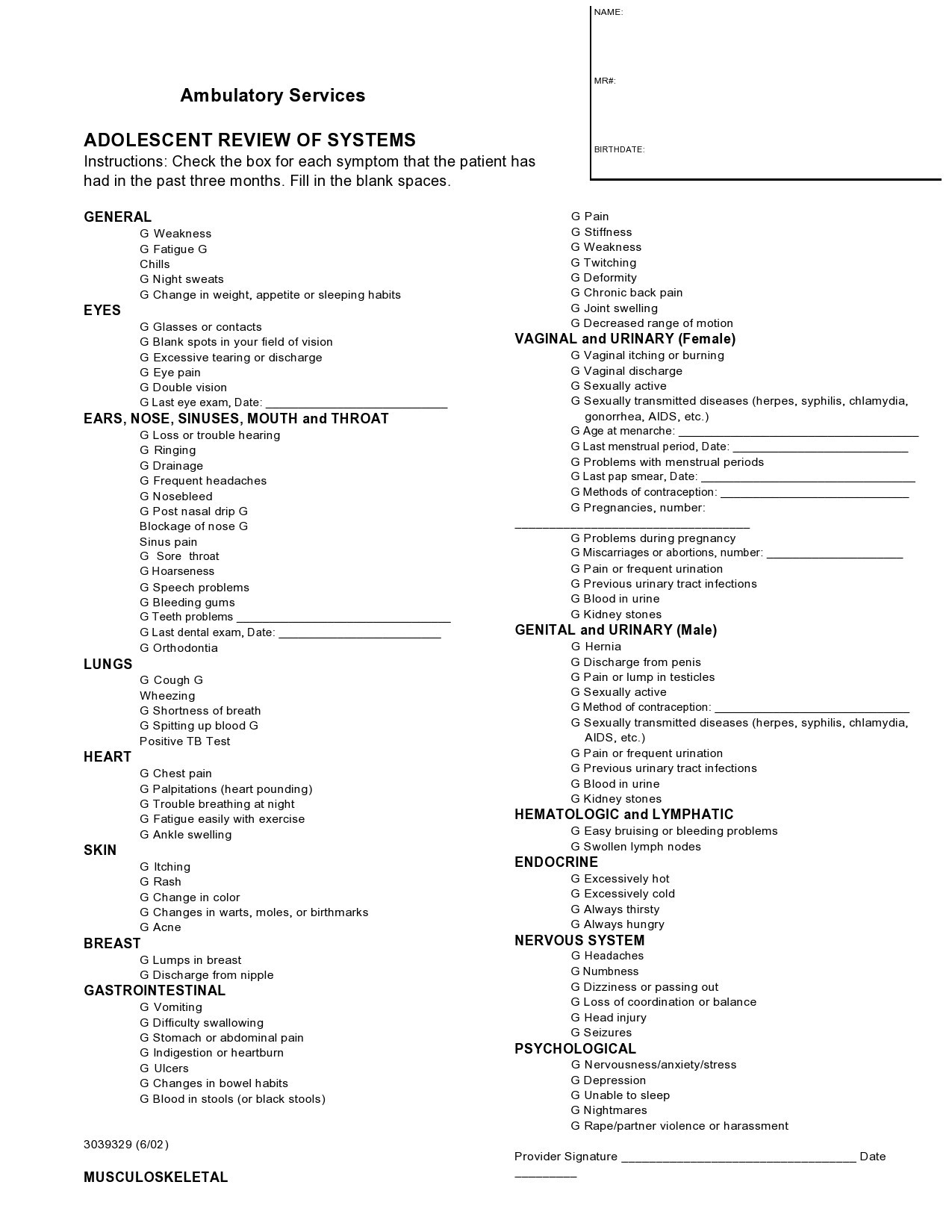
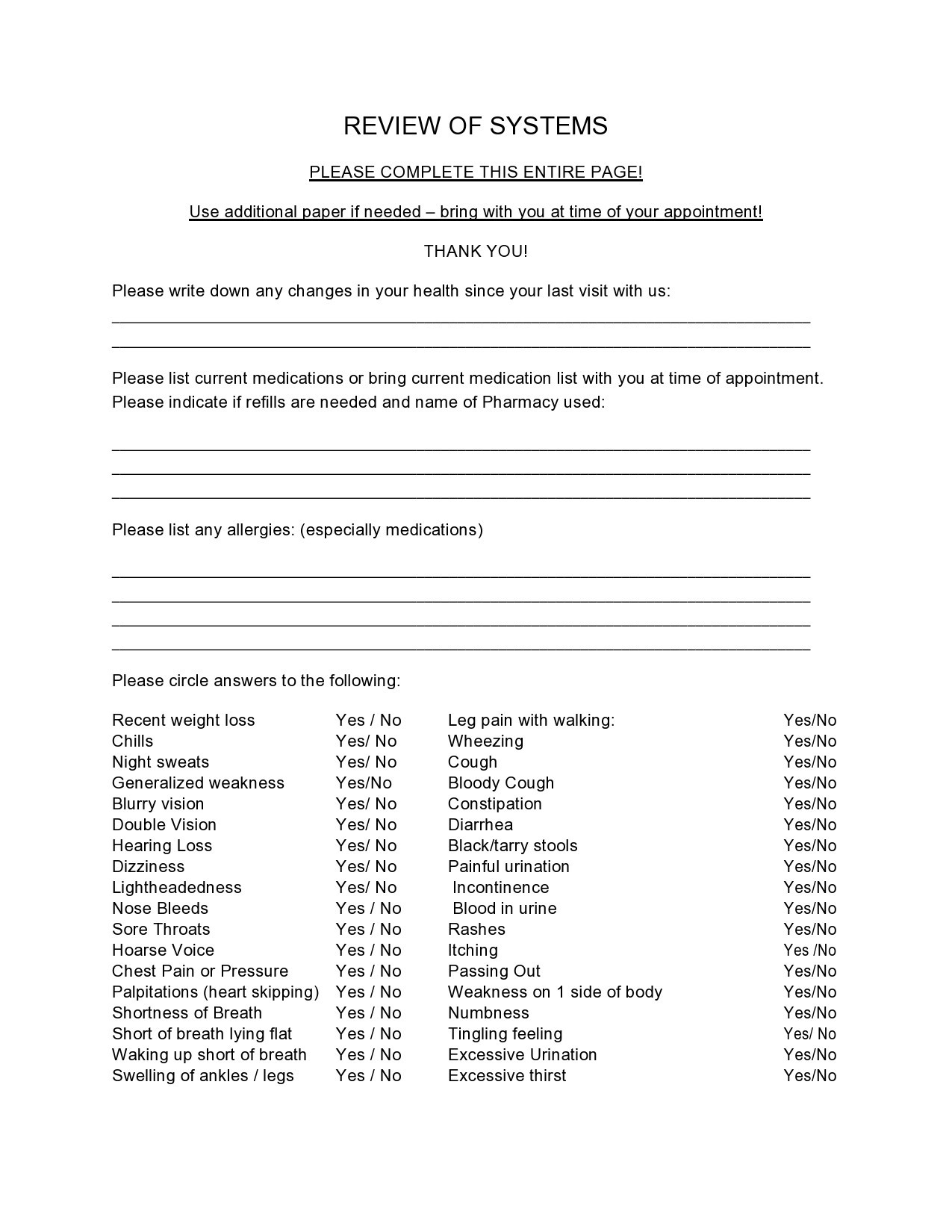
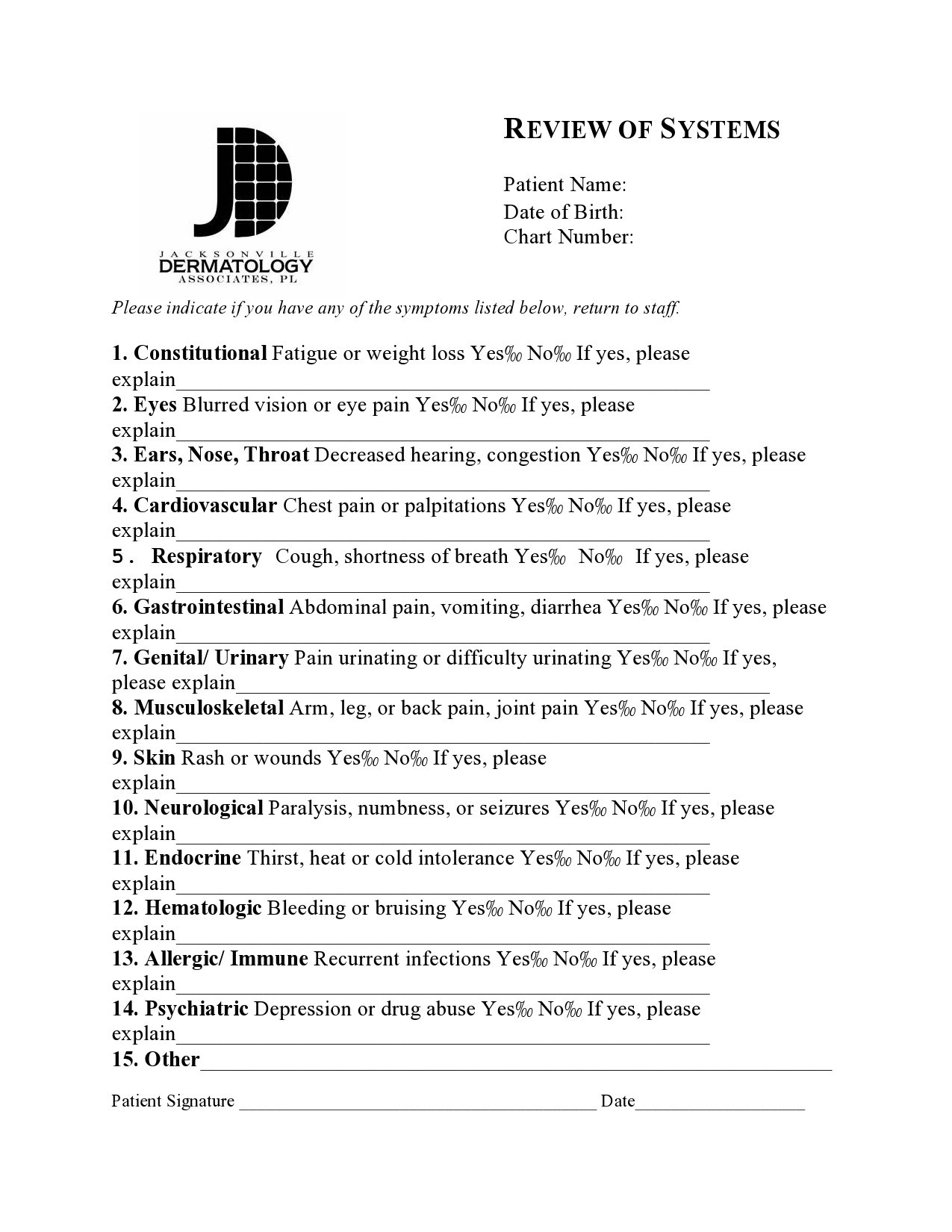
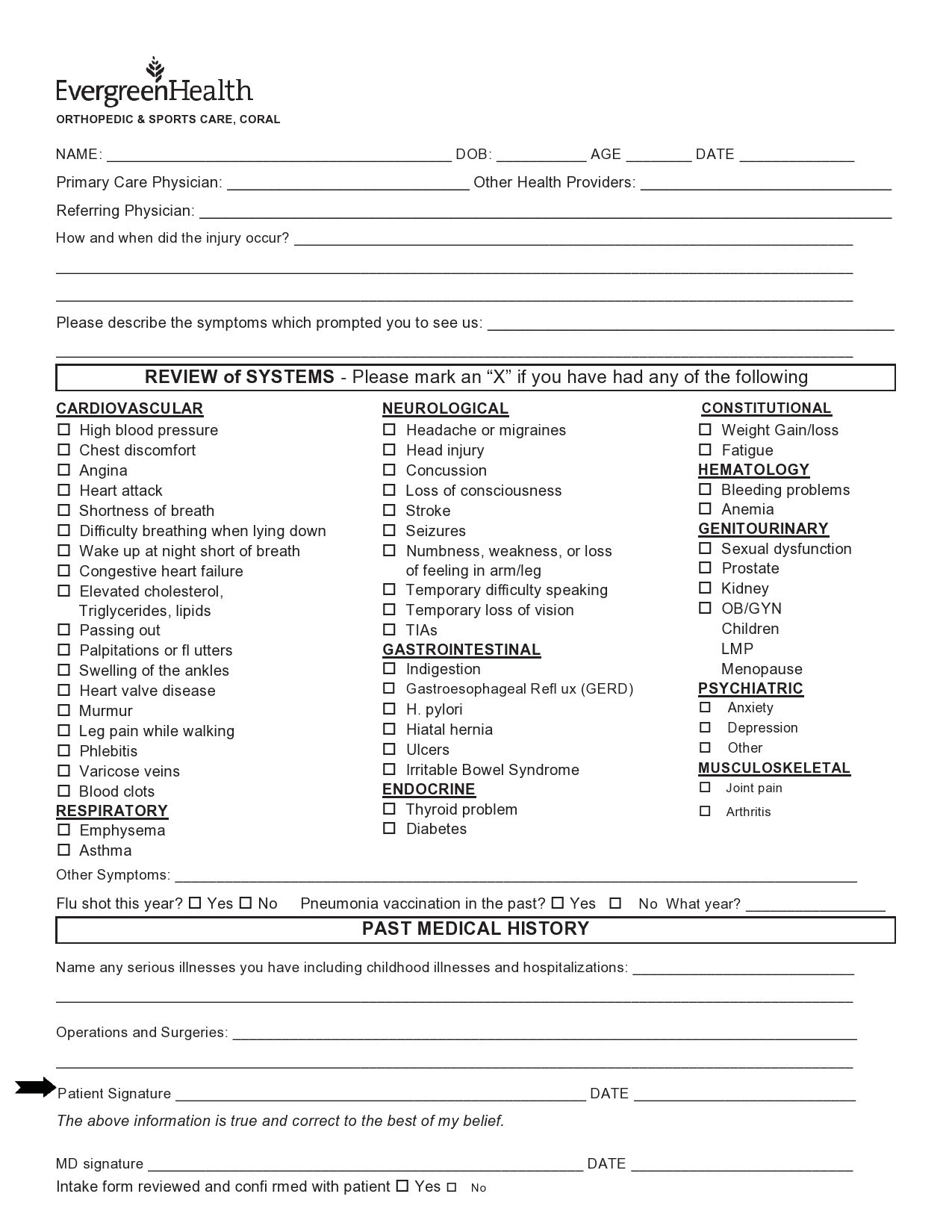
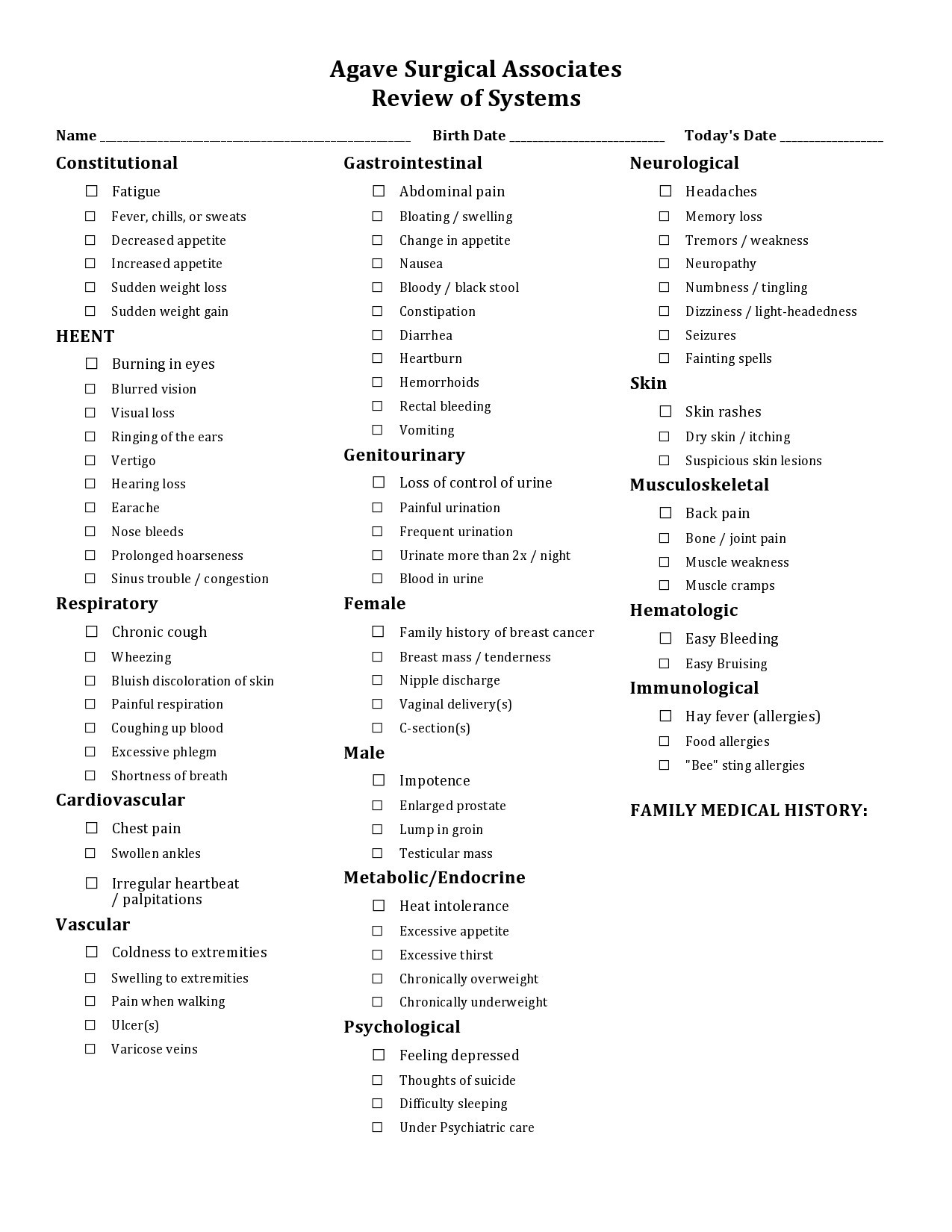
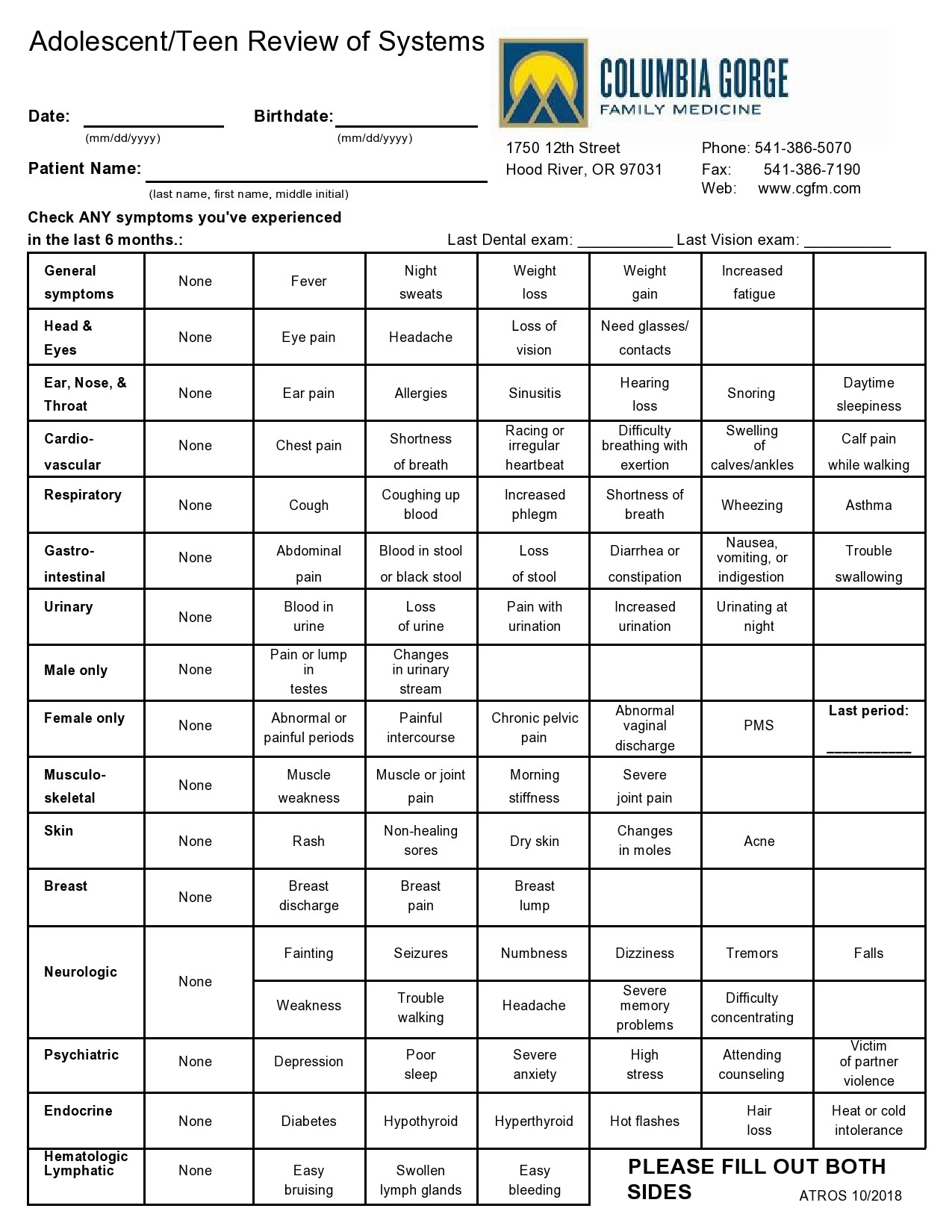
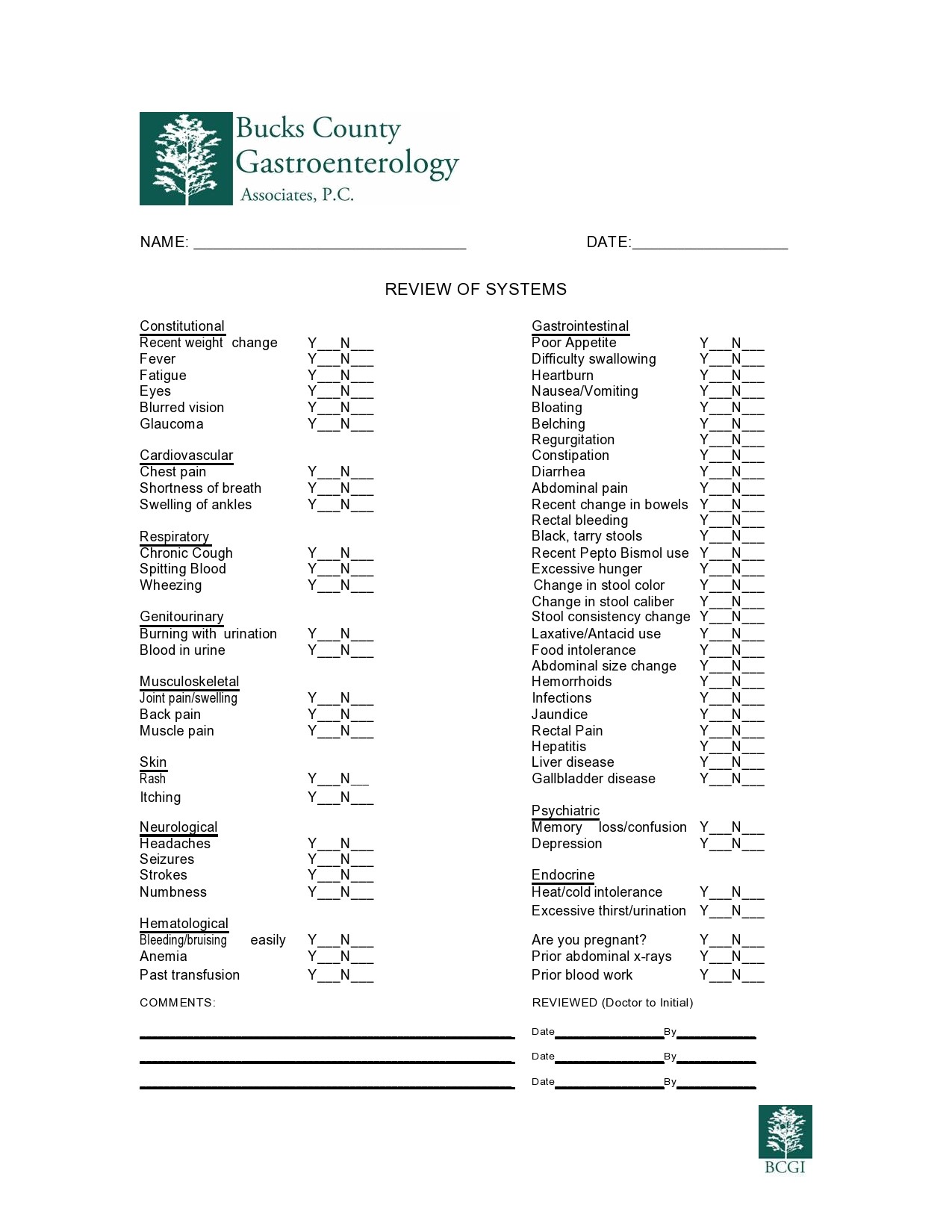
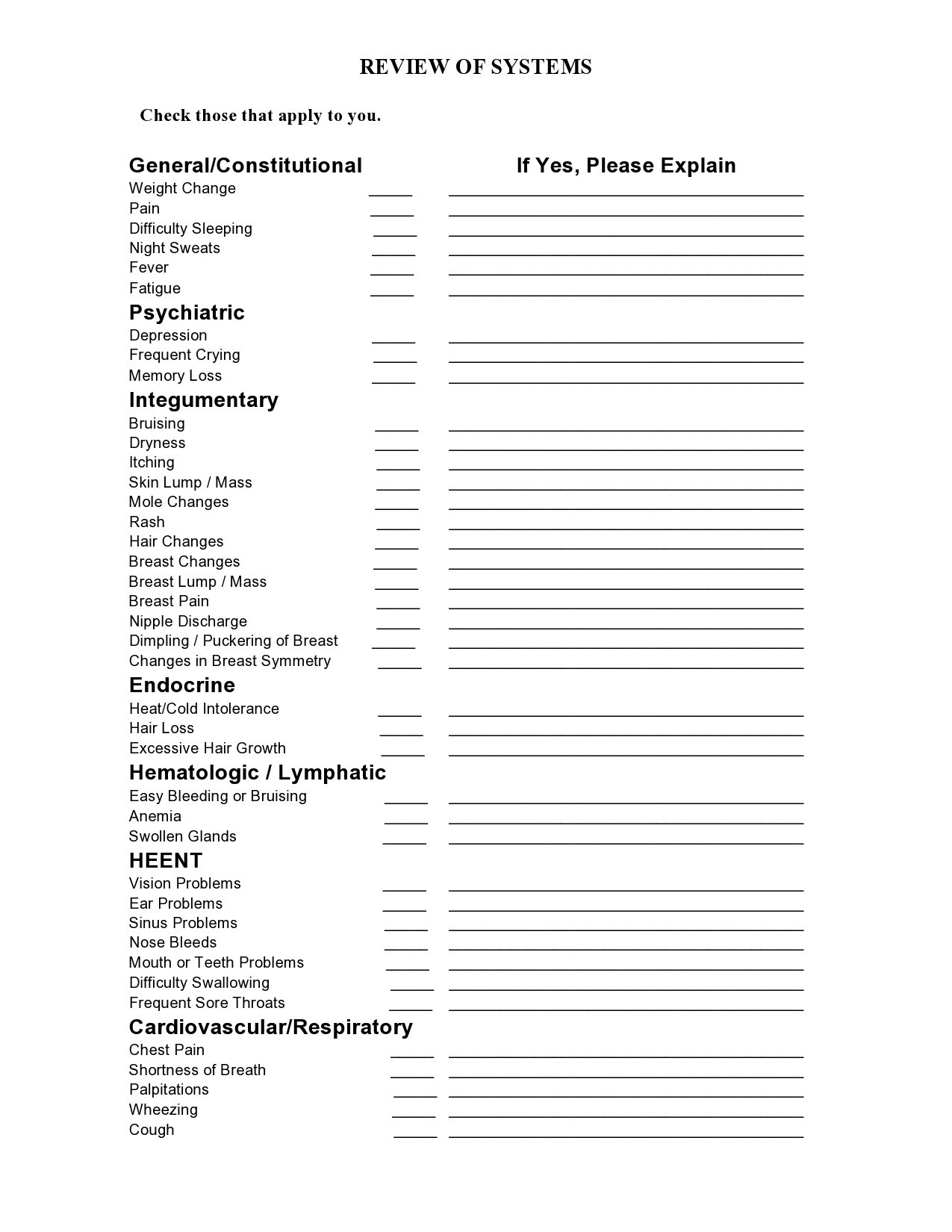
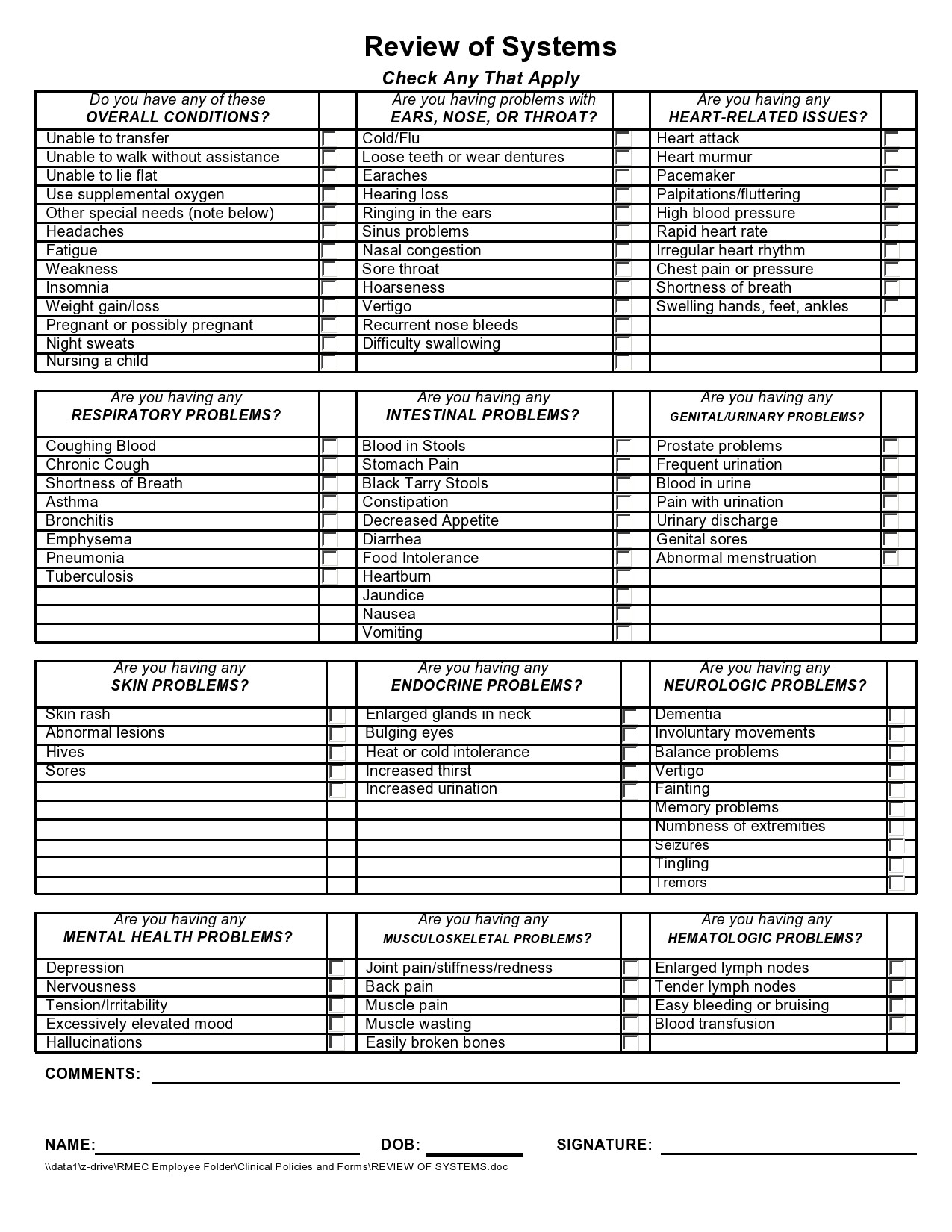
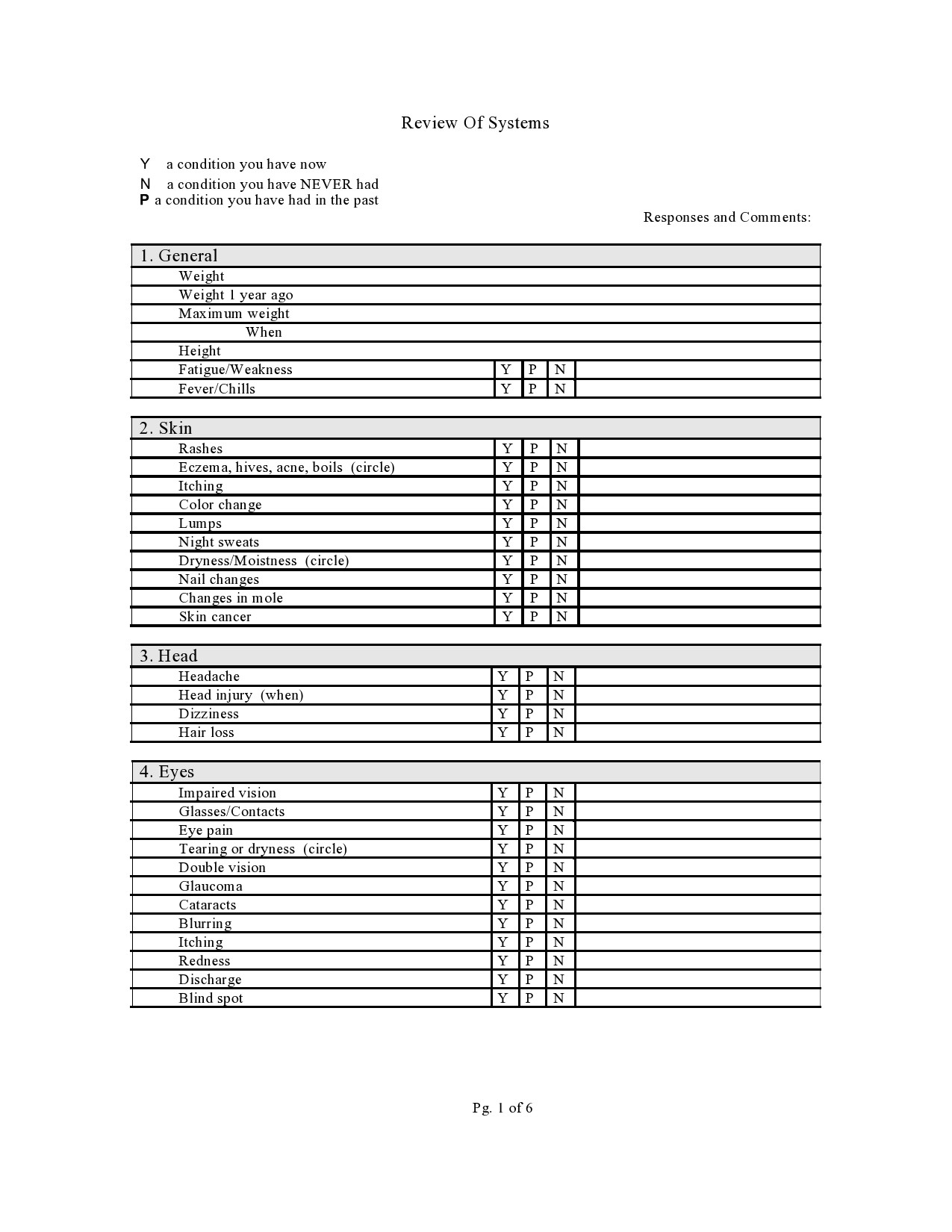
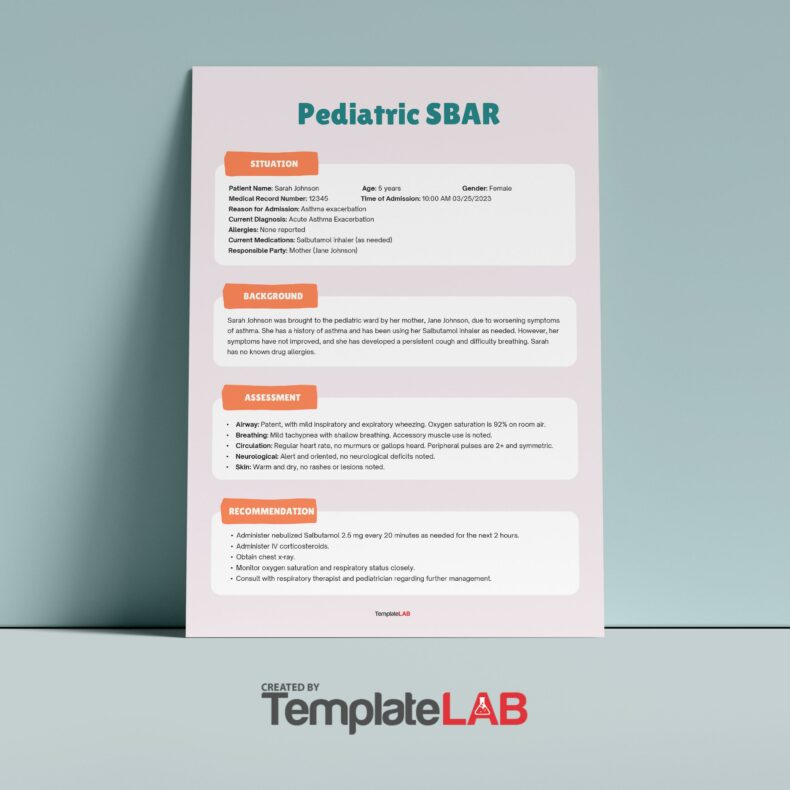
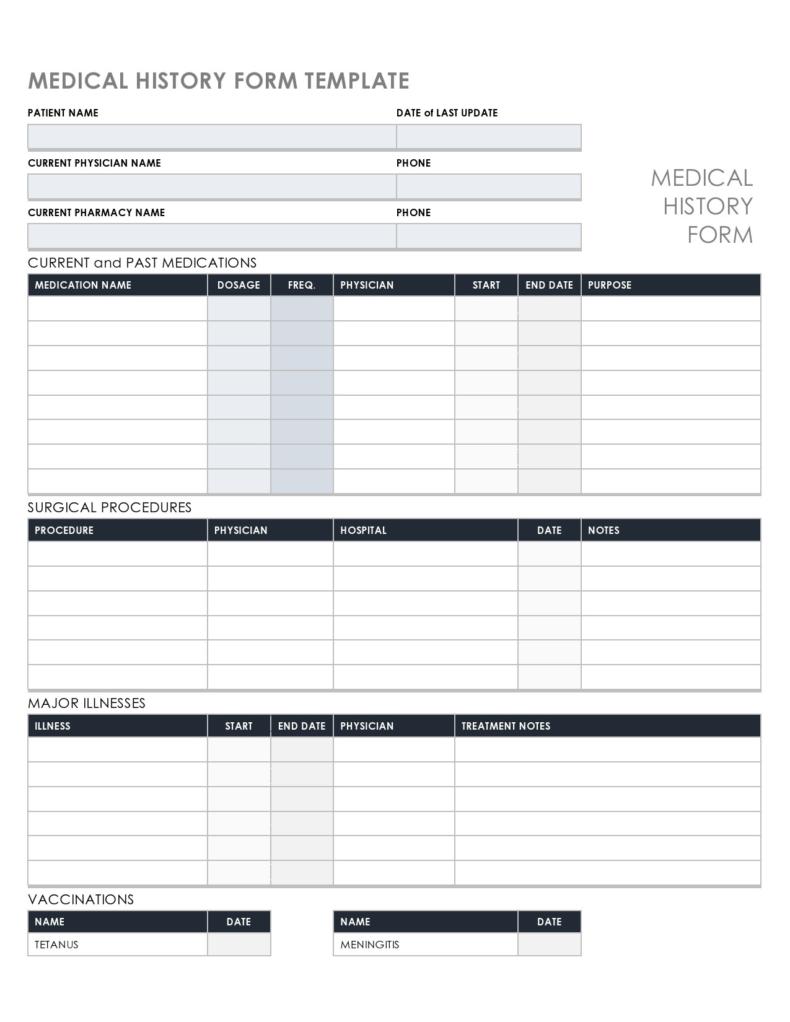
Review of Systems Templates
What is a complete review of systems?
According to the 1995 guidelines for medical documentation, there are 10 systems that constitute a complete ROS needed for Level 5 visits. When you review all of the systems with patients, you need to use documentation like a review of systems checklist.
However, there are those who don’t follow the guidelines strictly. In such a case, they may need documentation of 10 individual systems when they don’t think there is an indication that the systems got reviewed. There are also those who don’t trust EHR systems because they group responses on a review of systems cheat sheet and make it appear that you’re getting 10 when actually, it’s fewer than that.
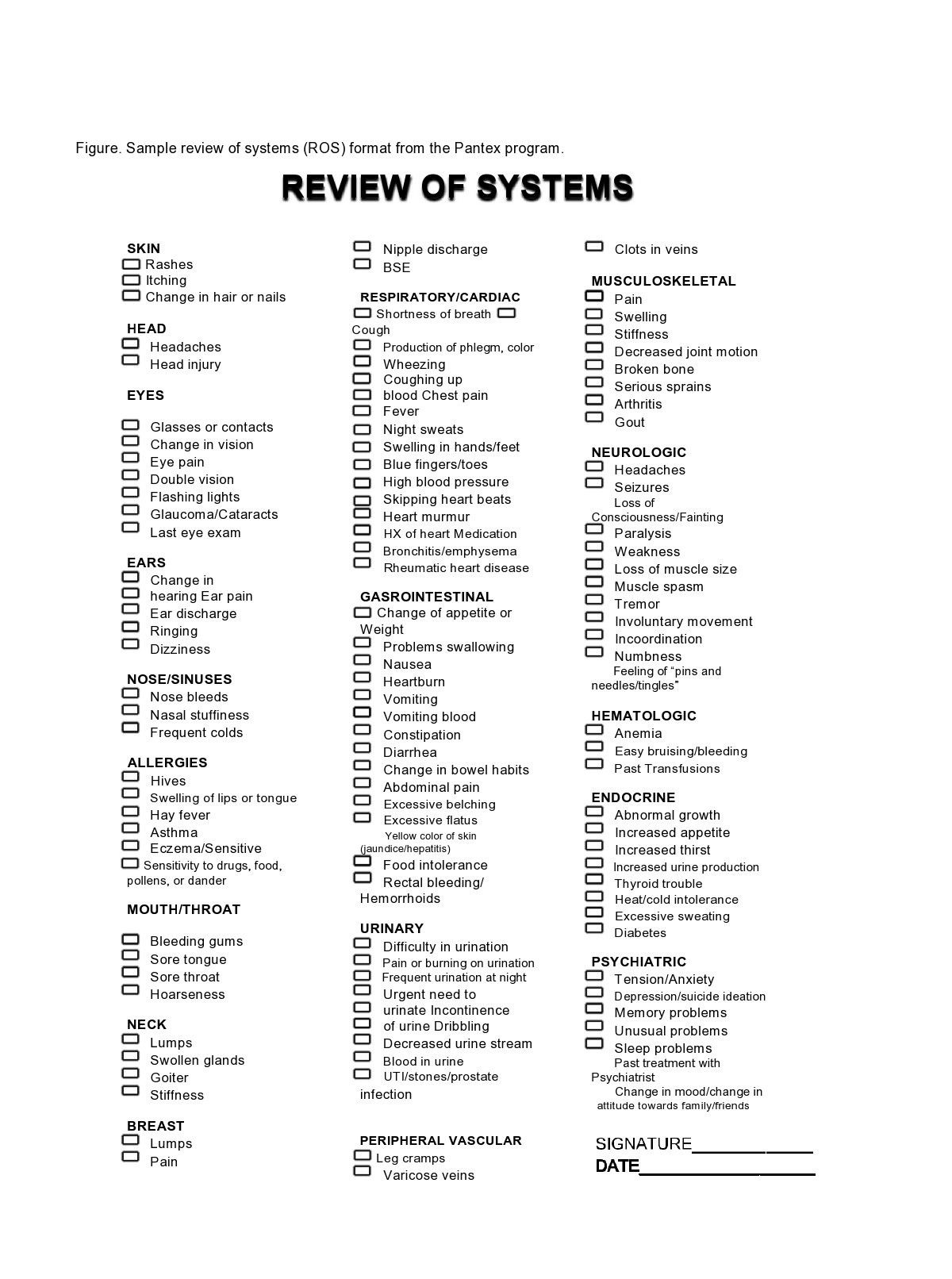
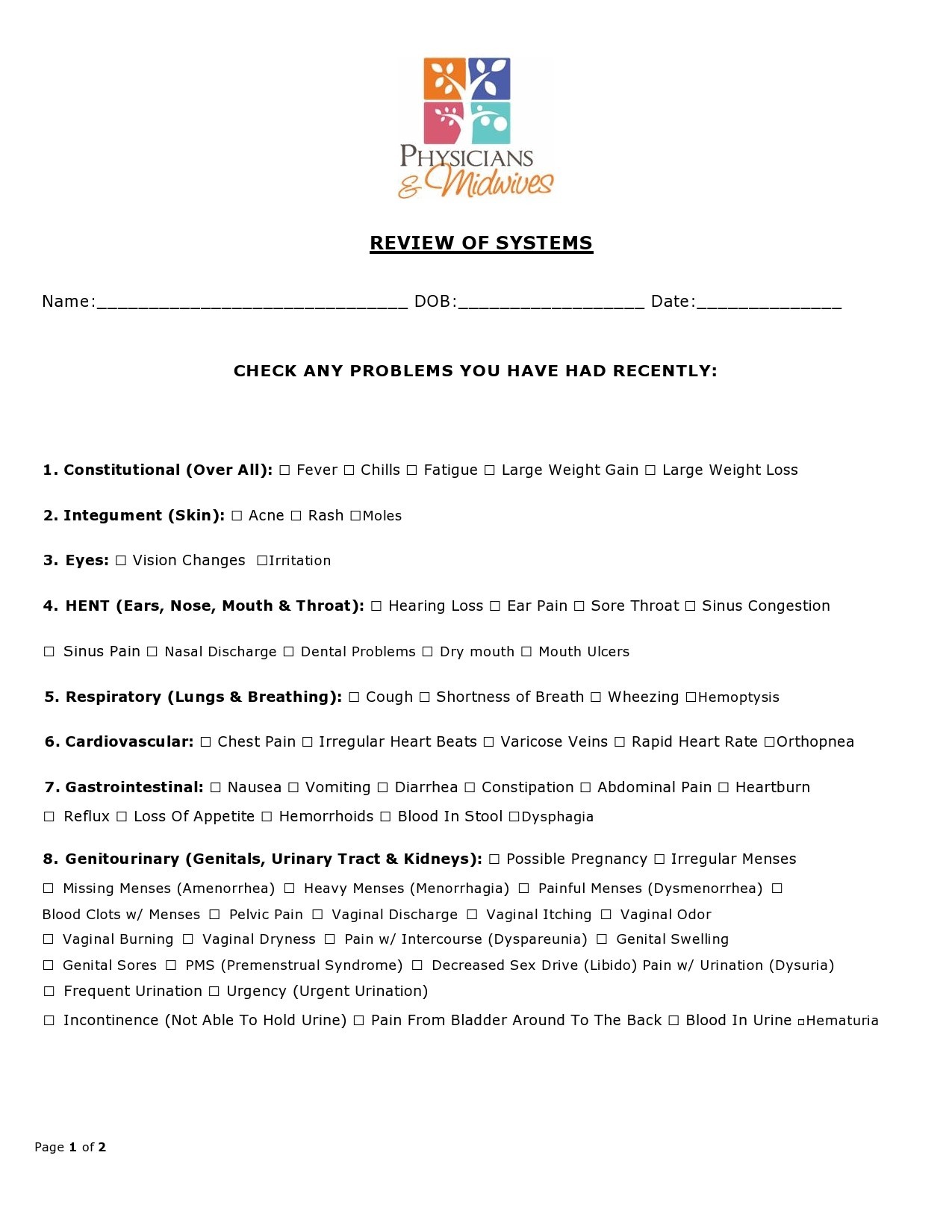
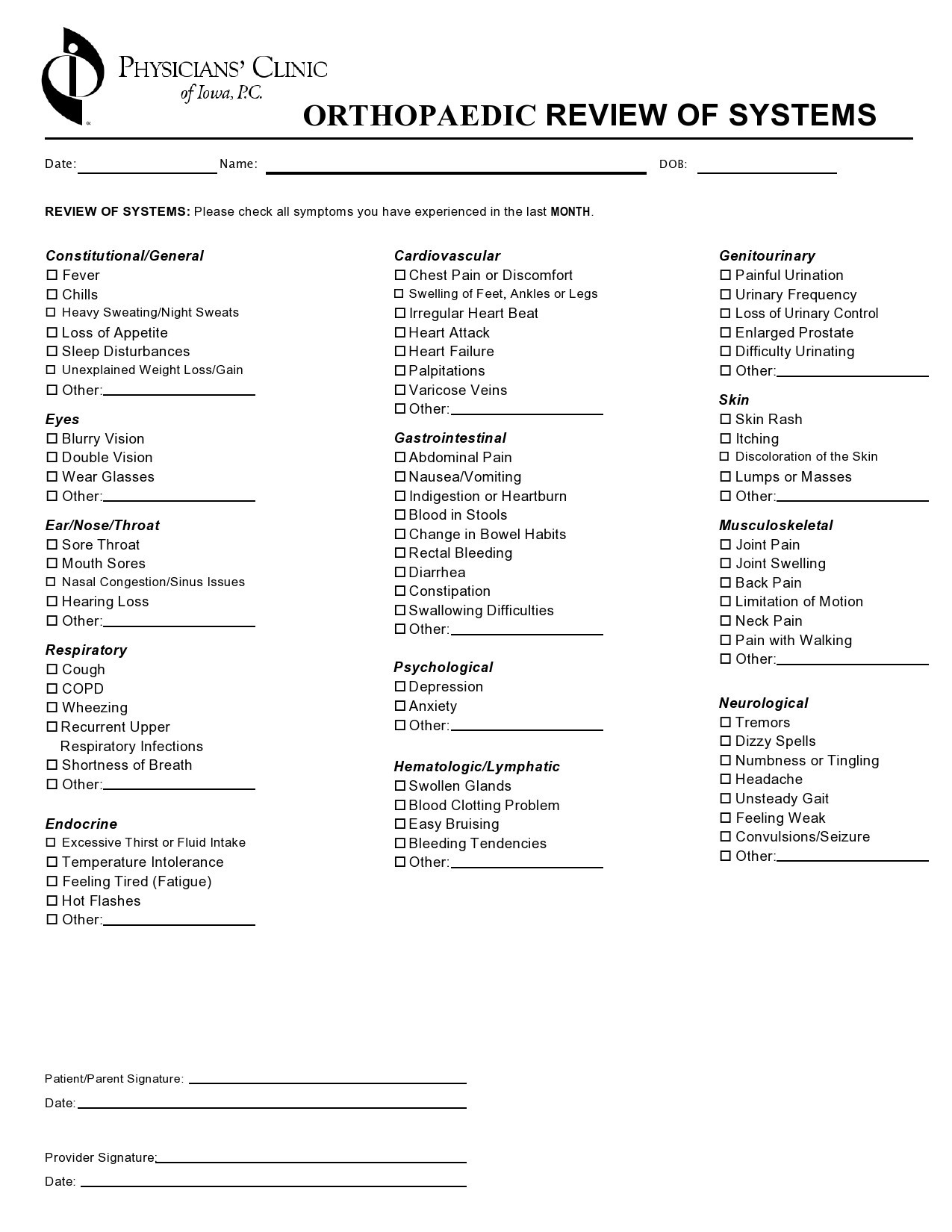
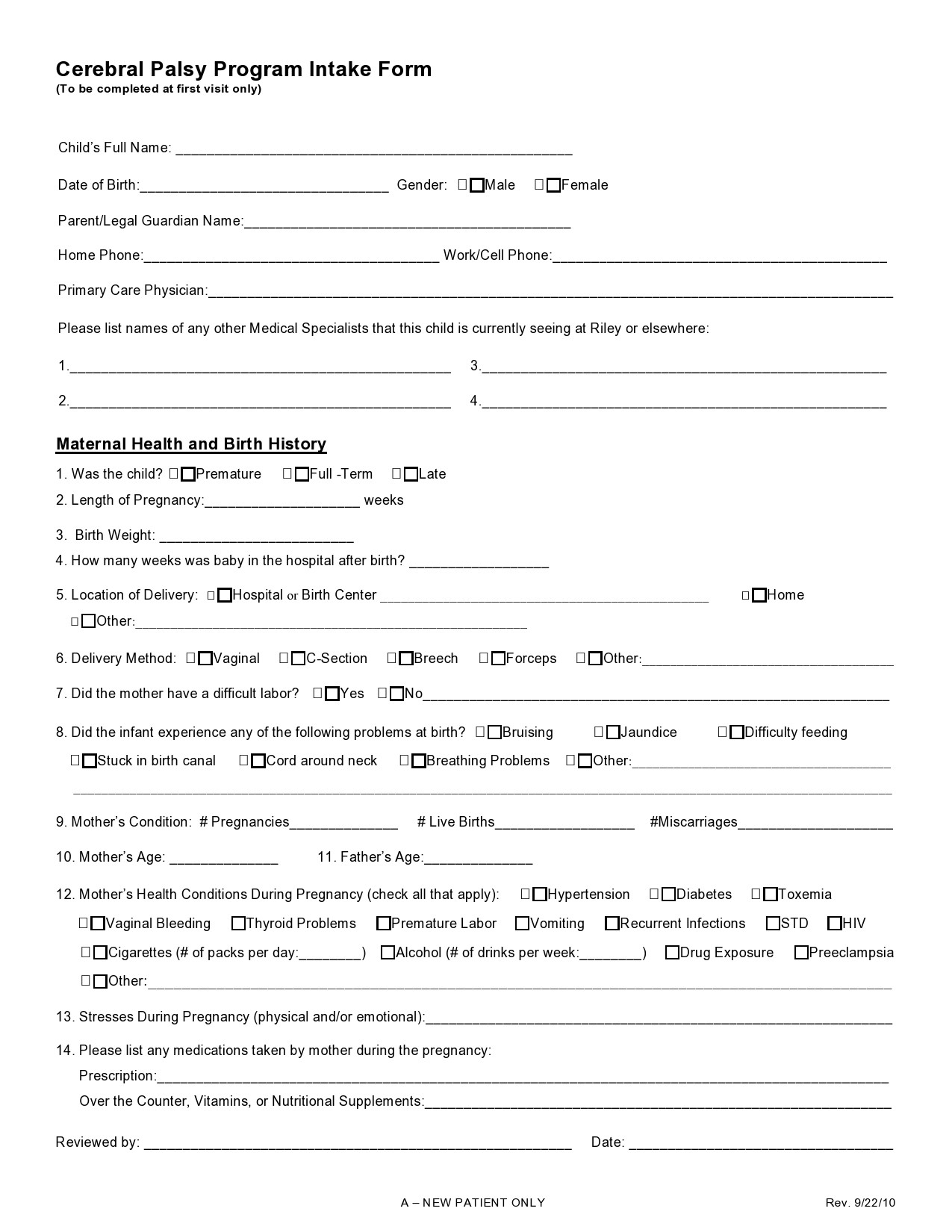
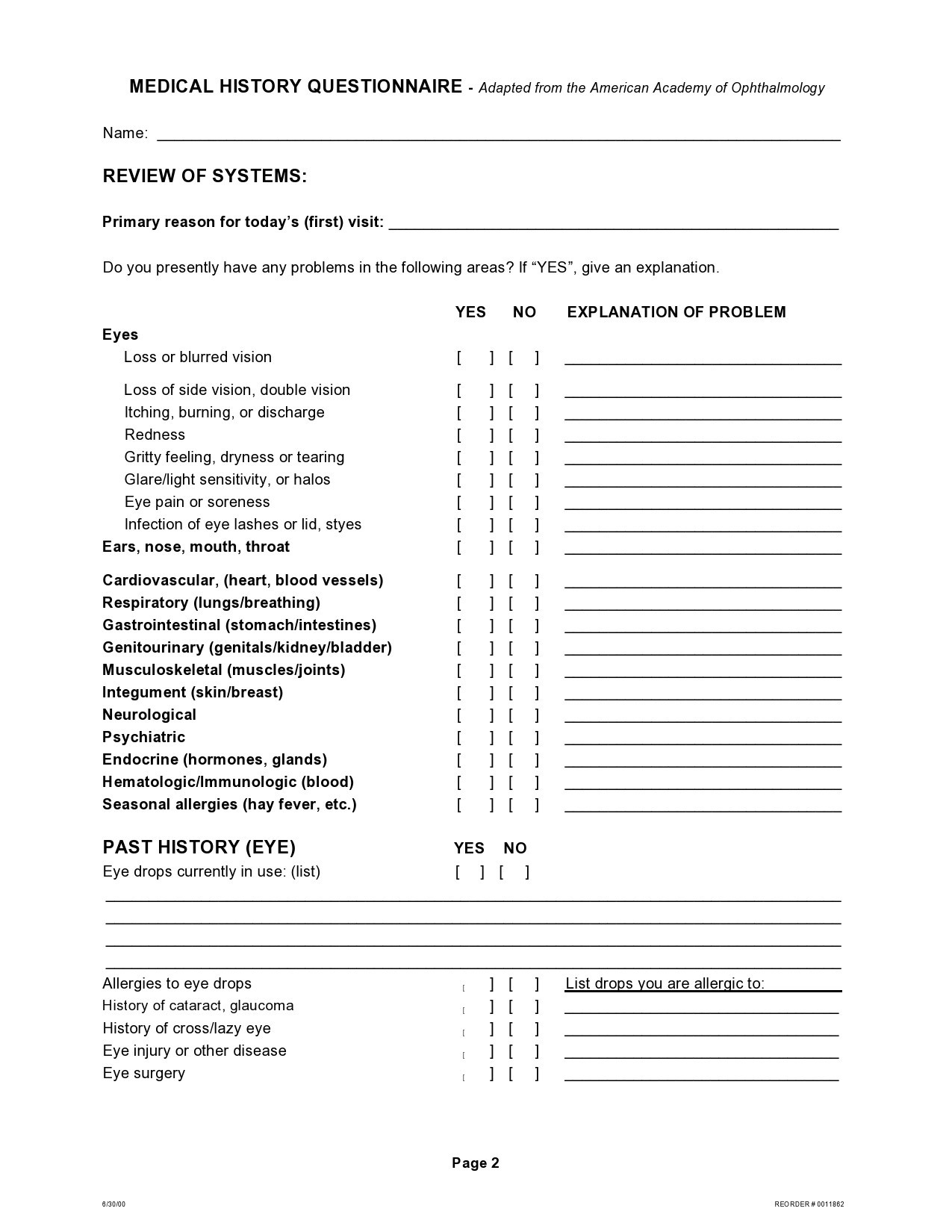
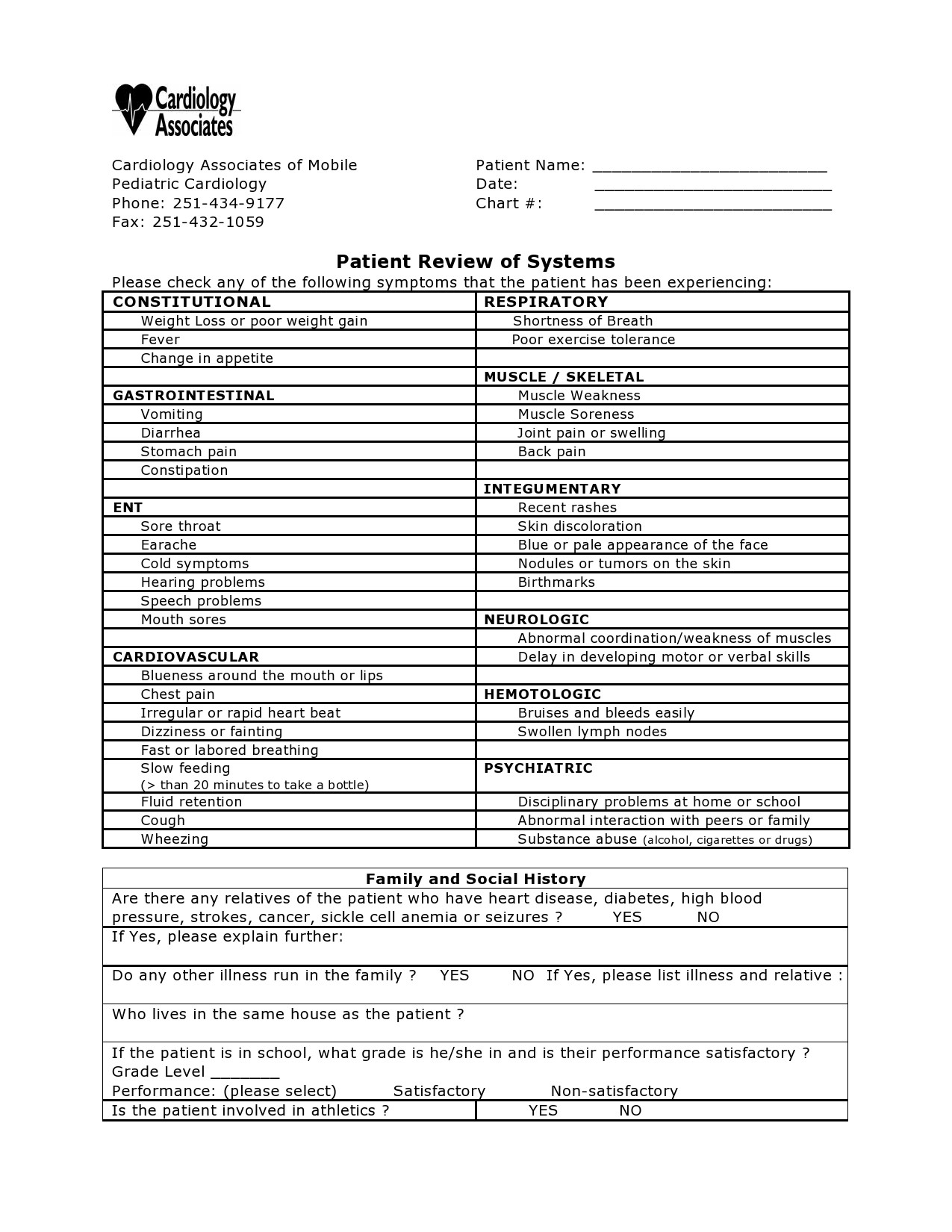
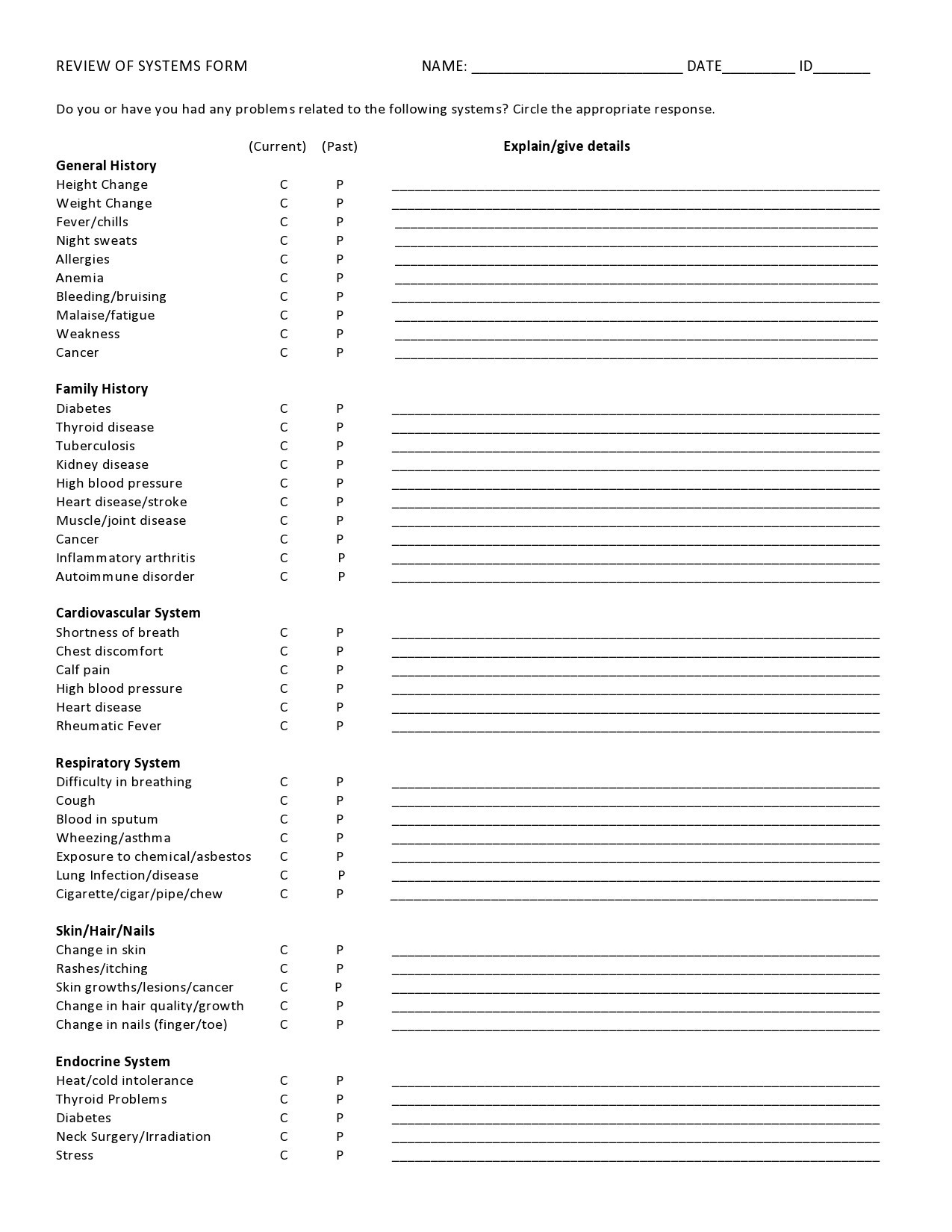
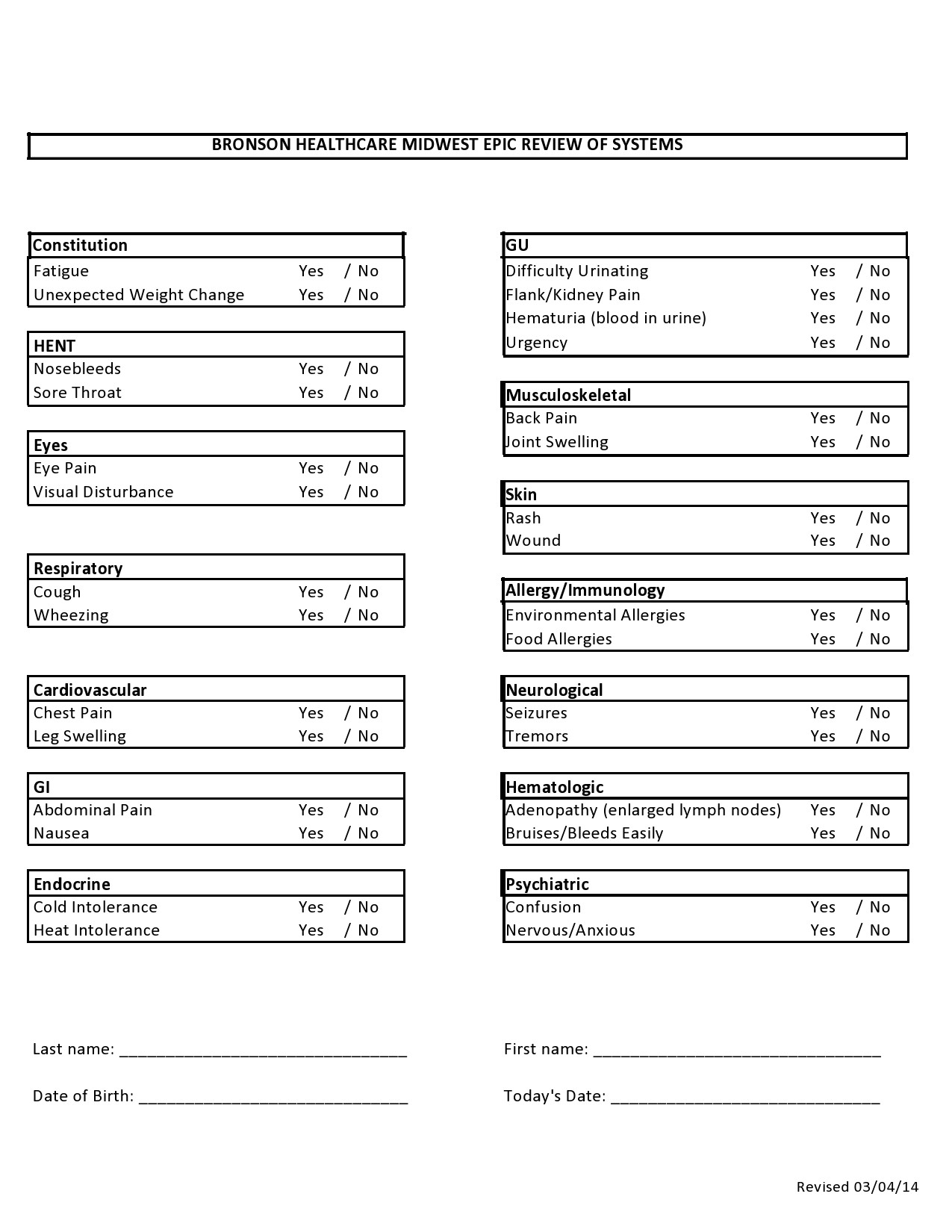
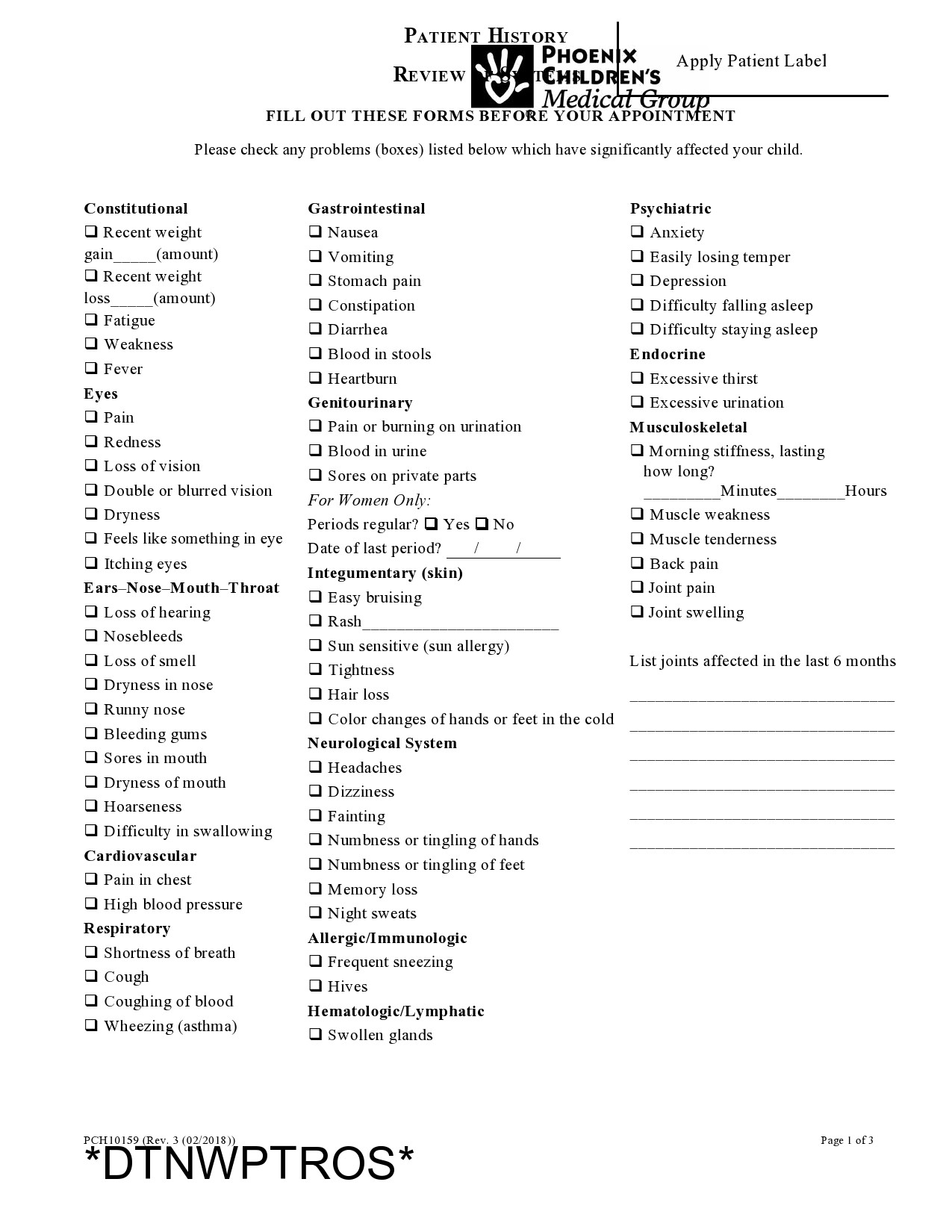
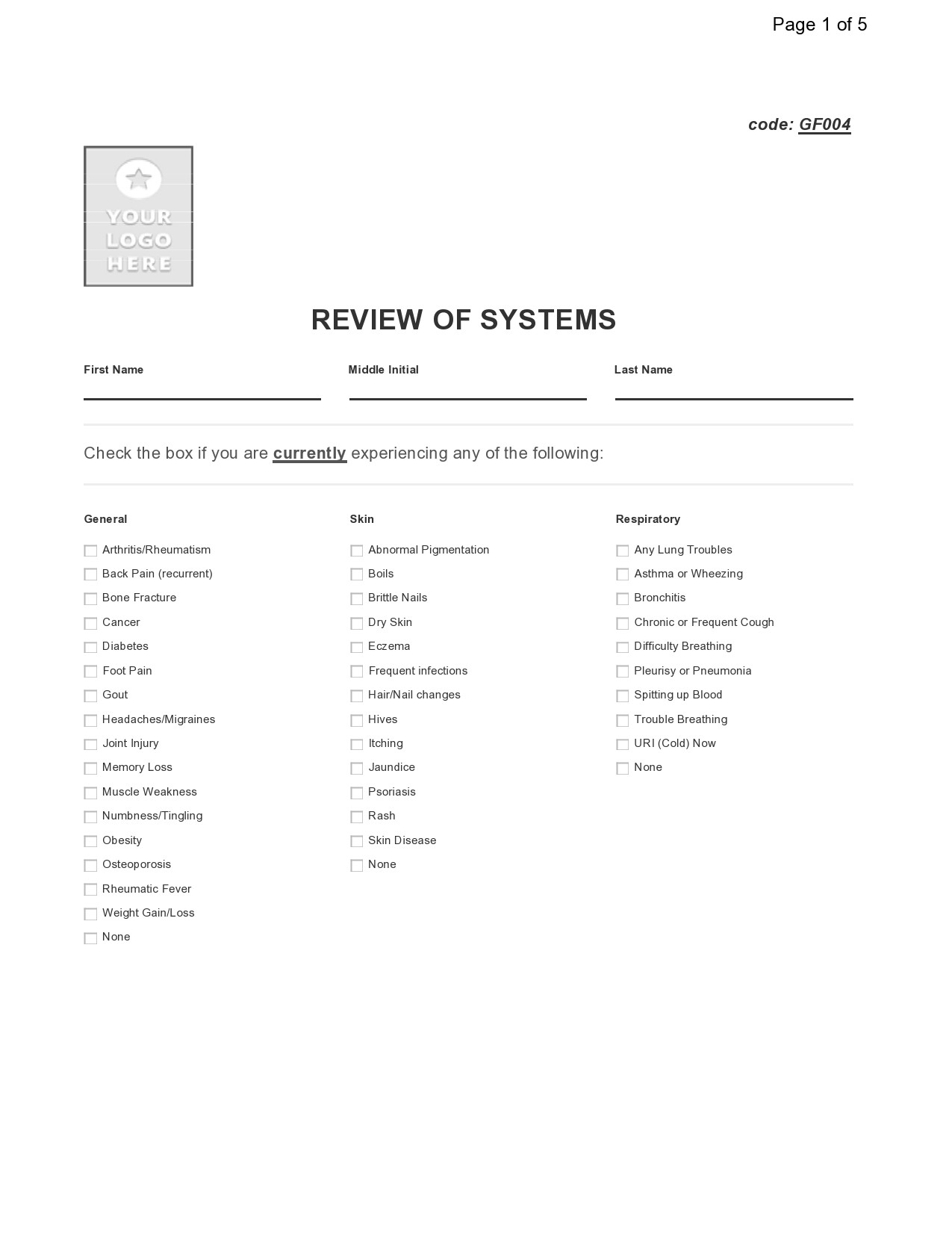
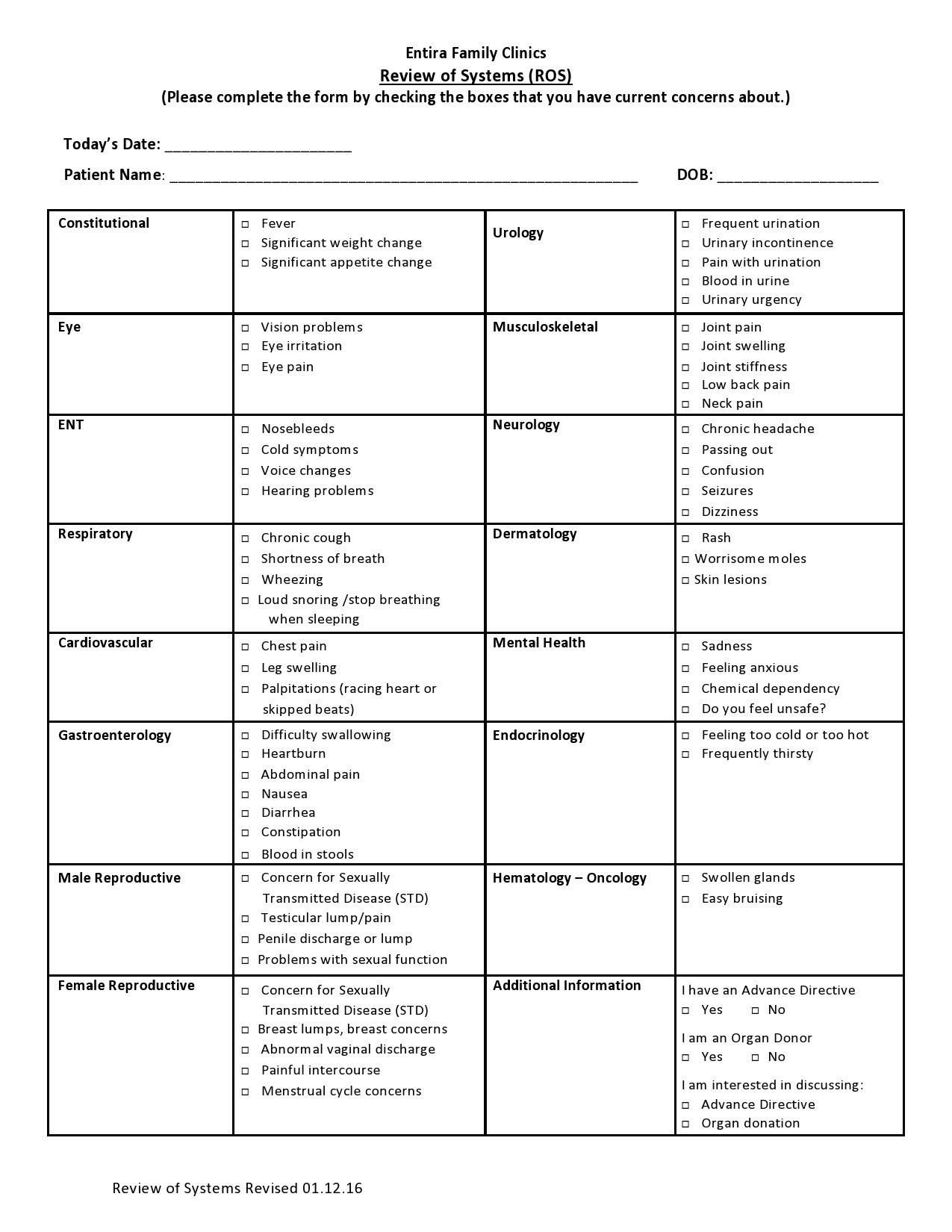
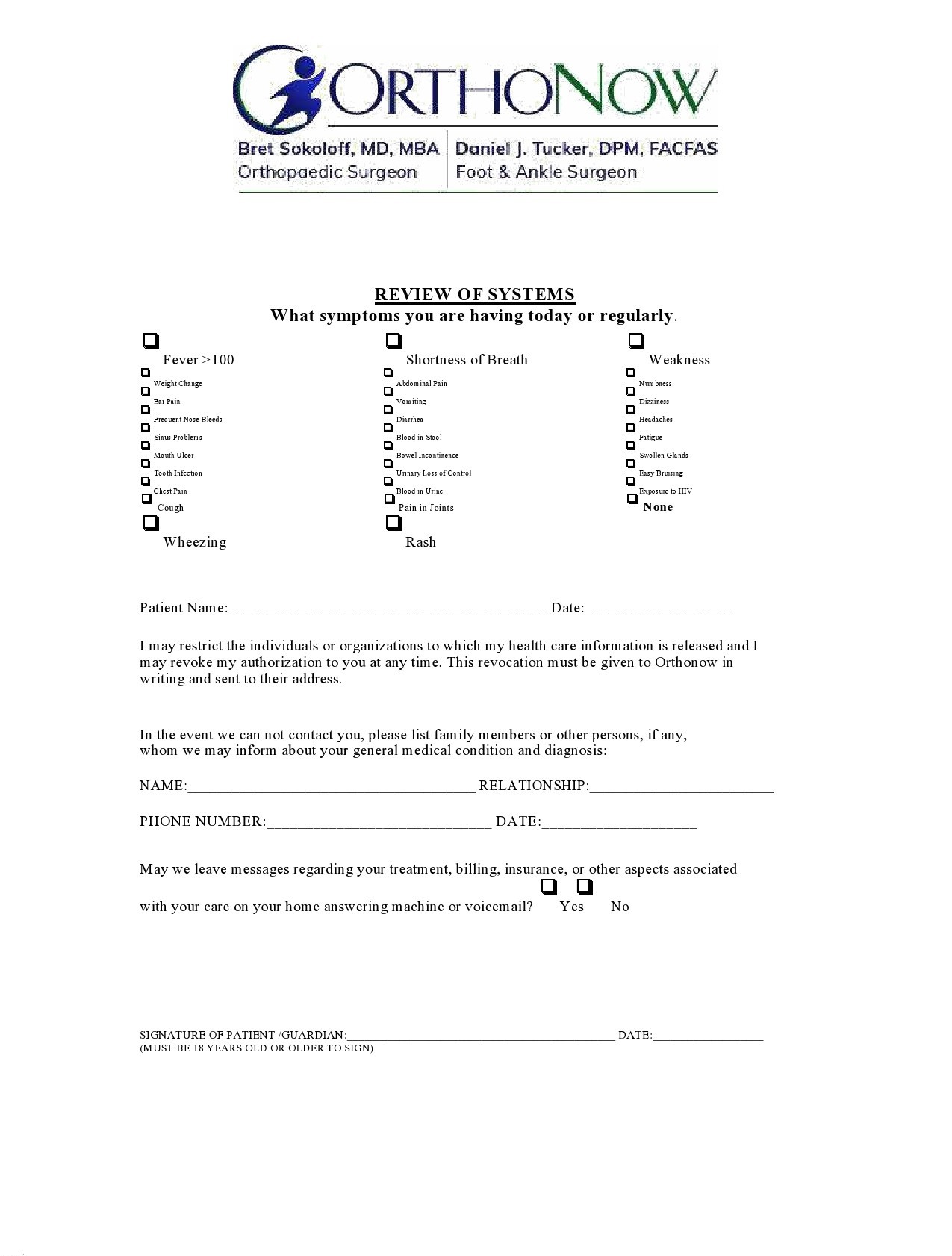
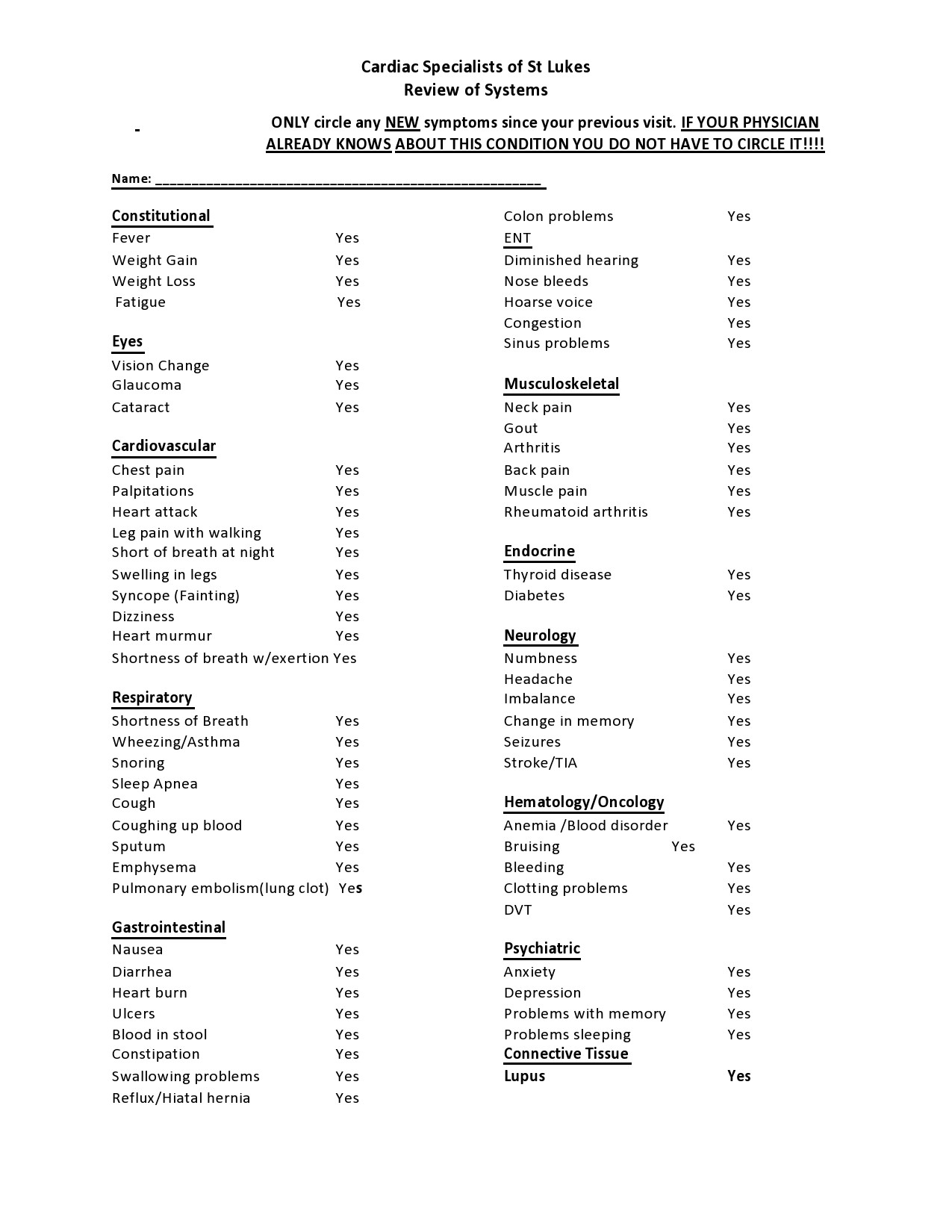
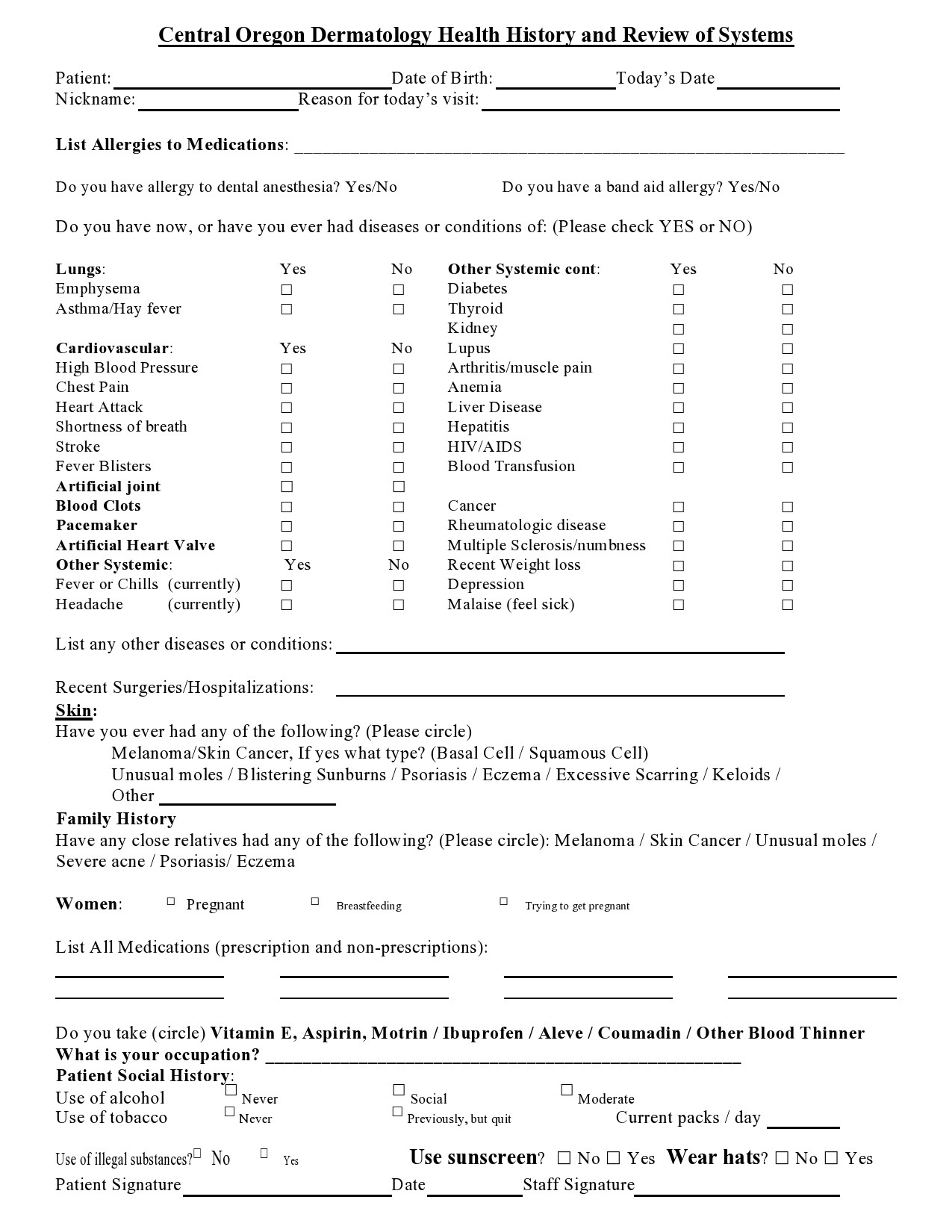
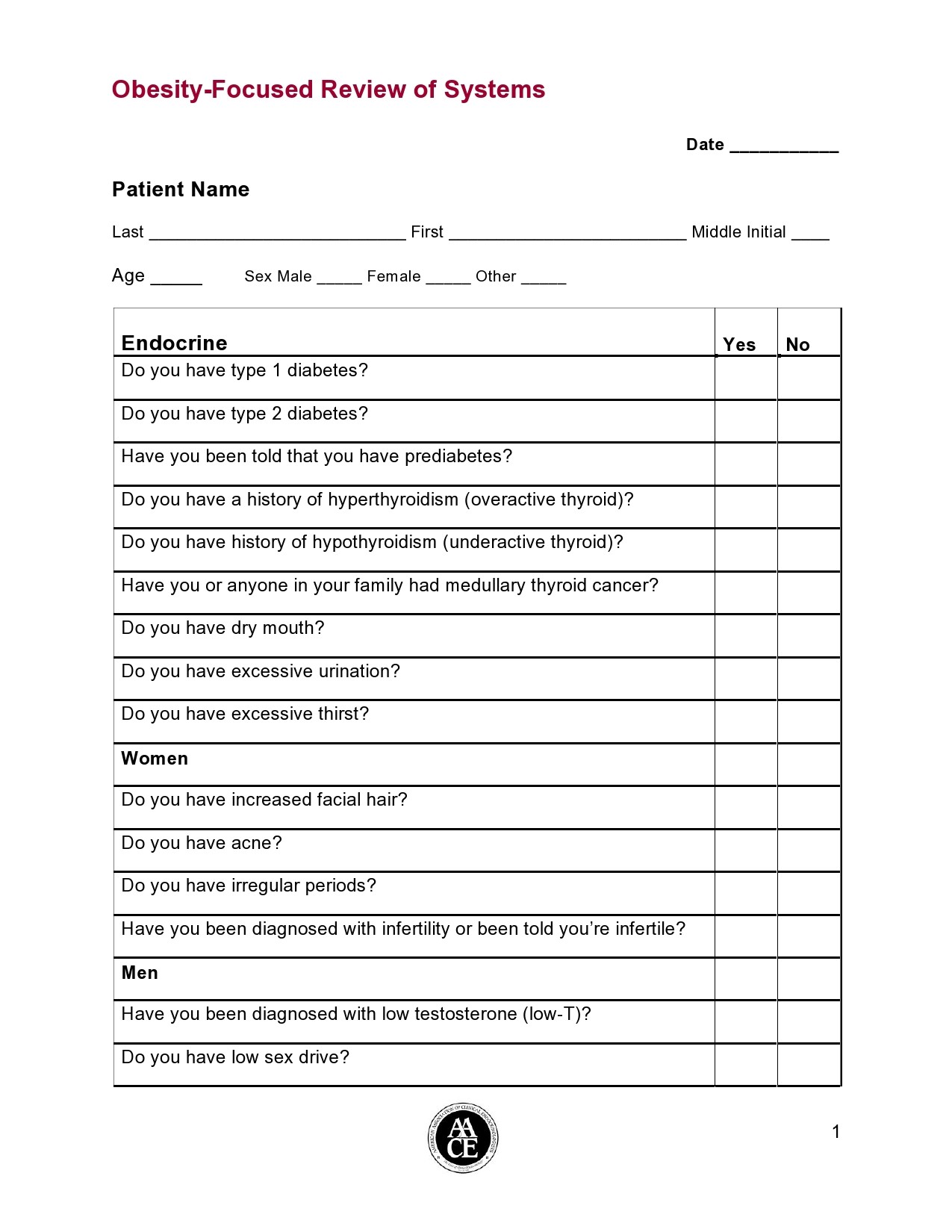
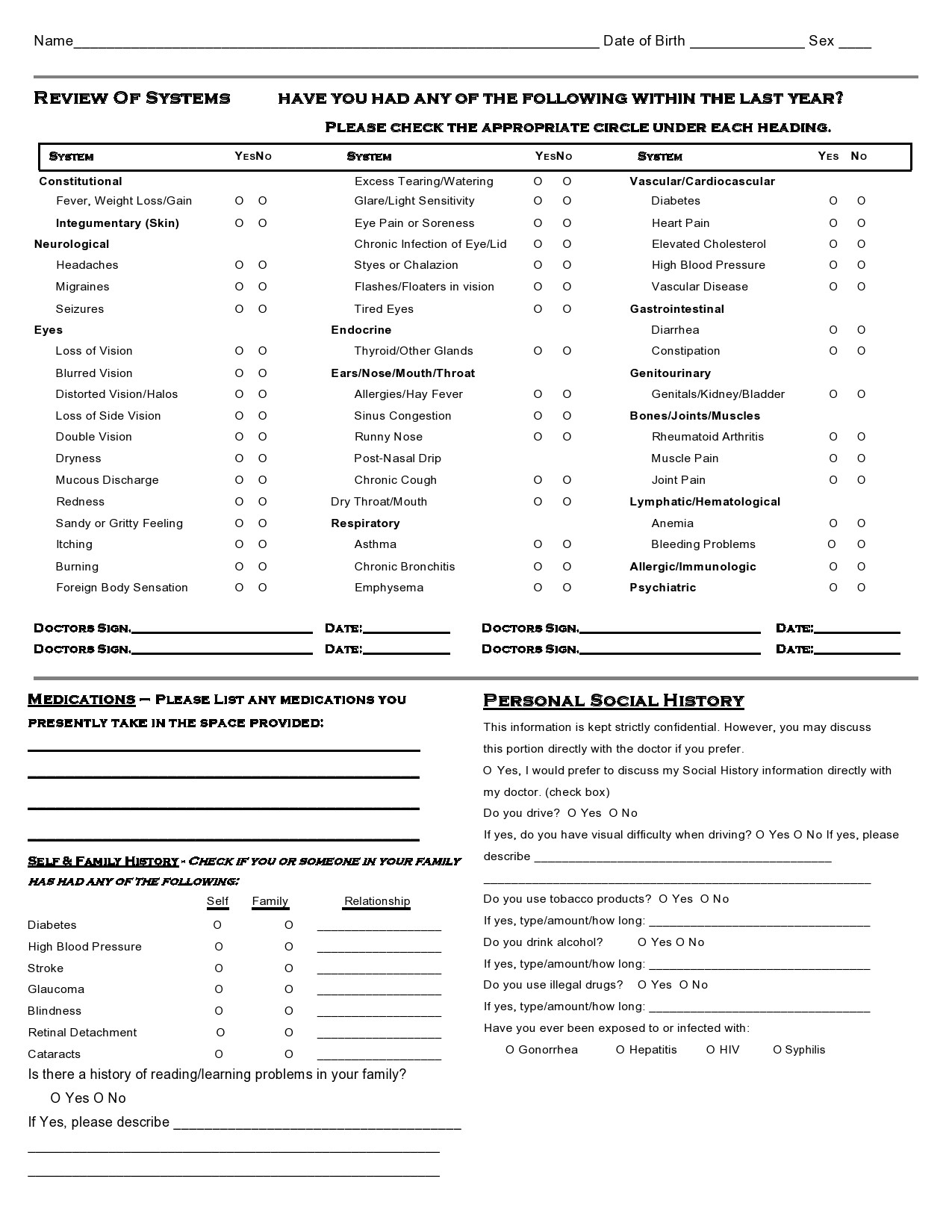
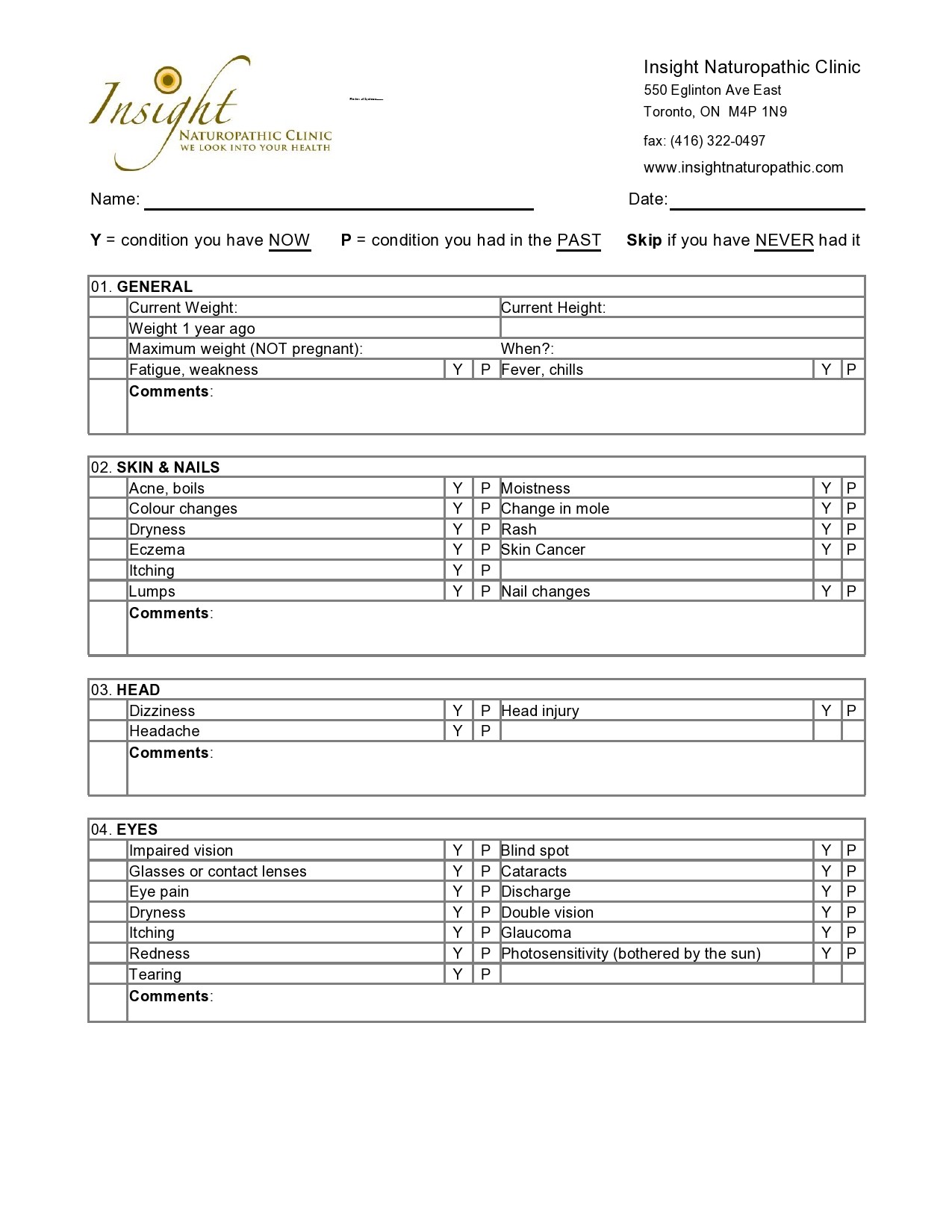
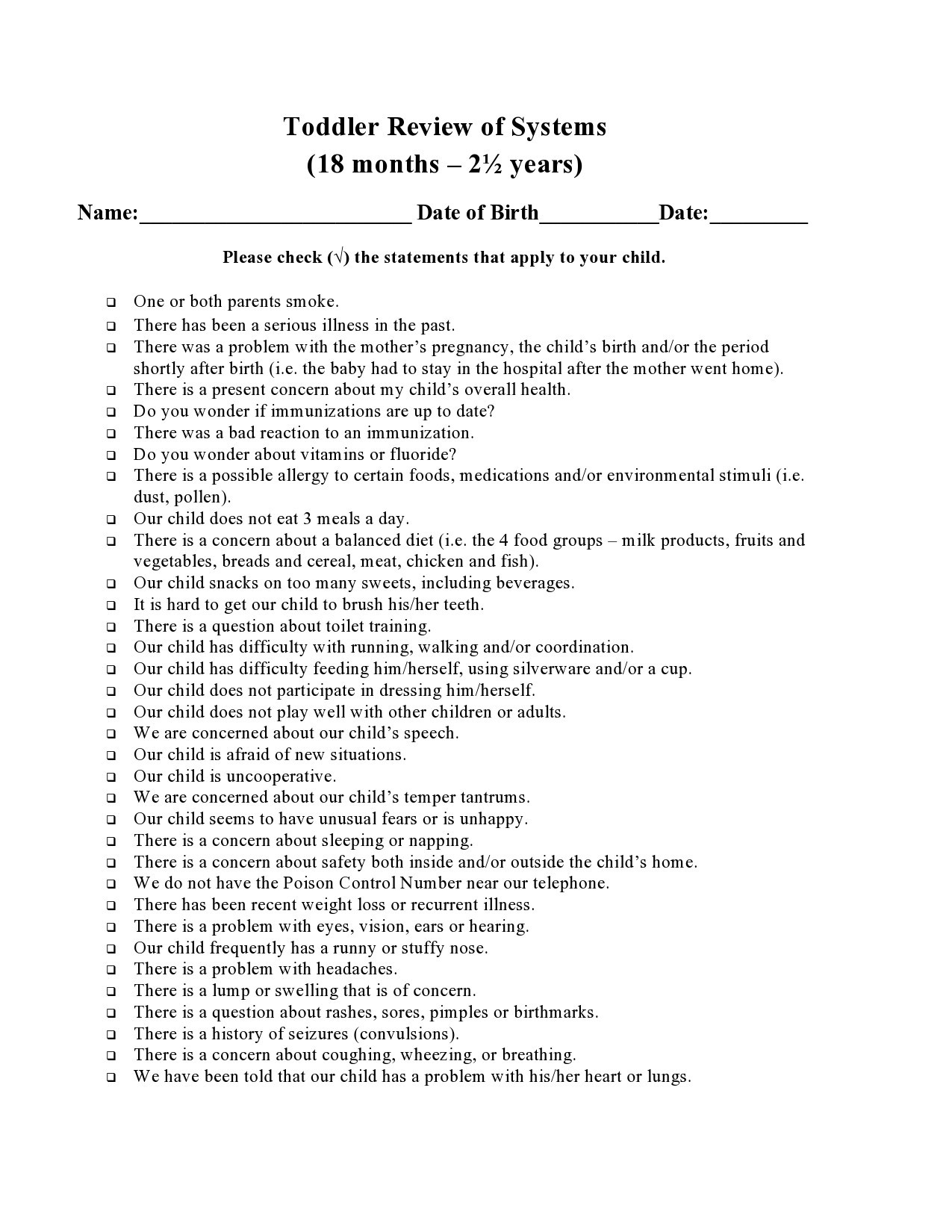
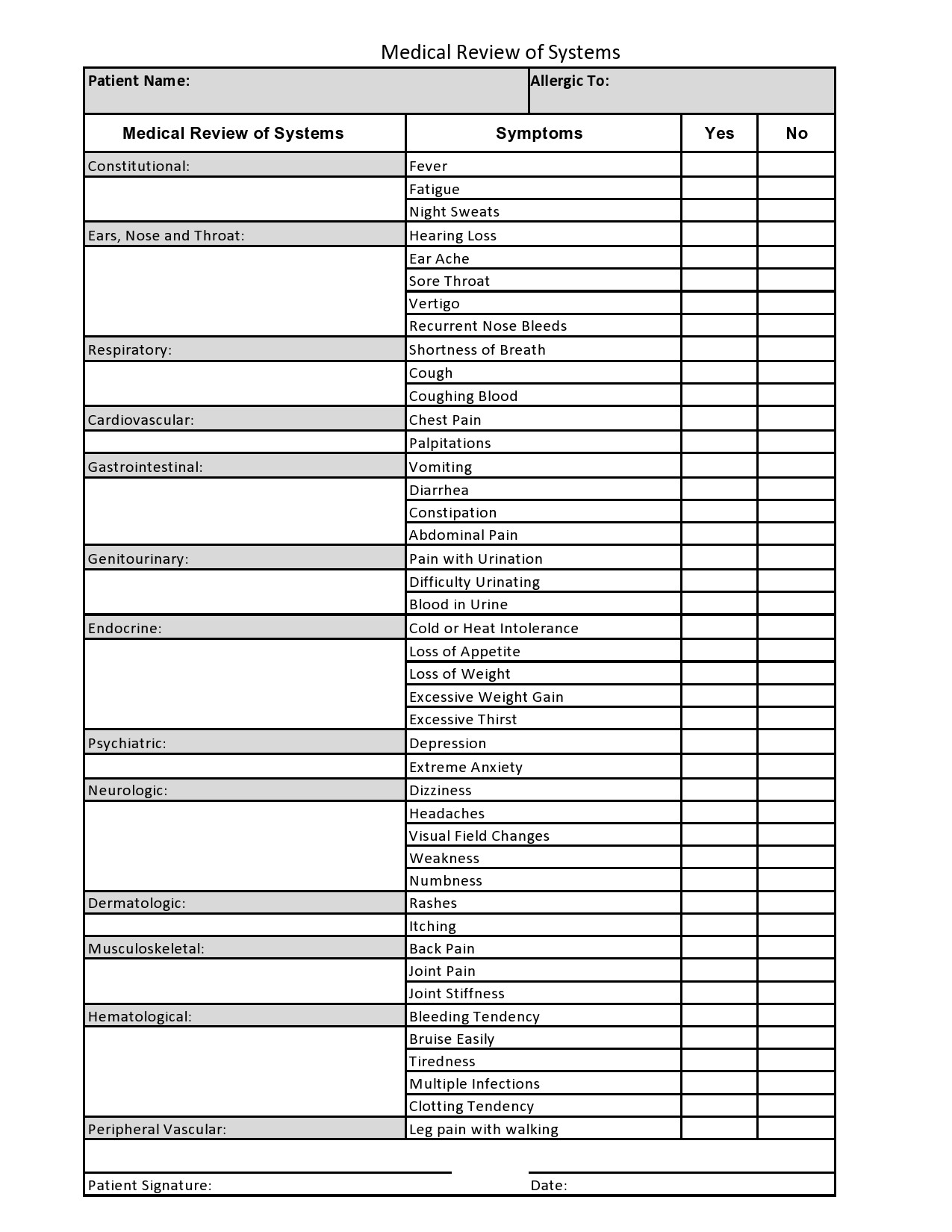
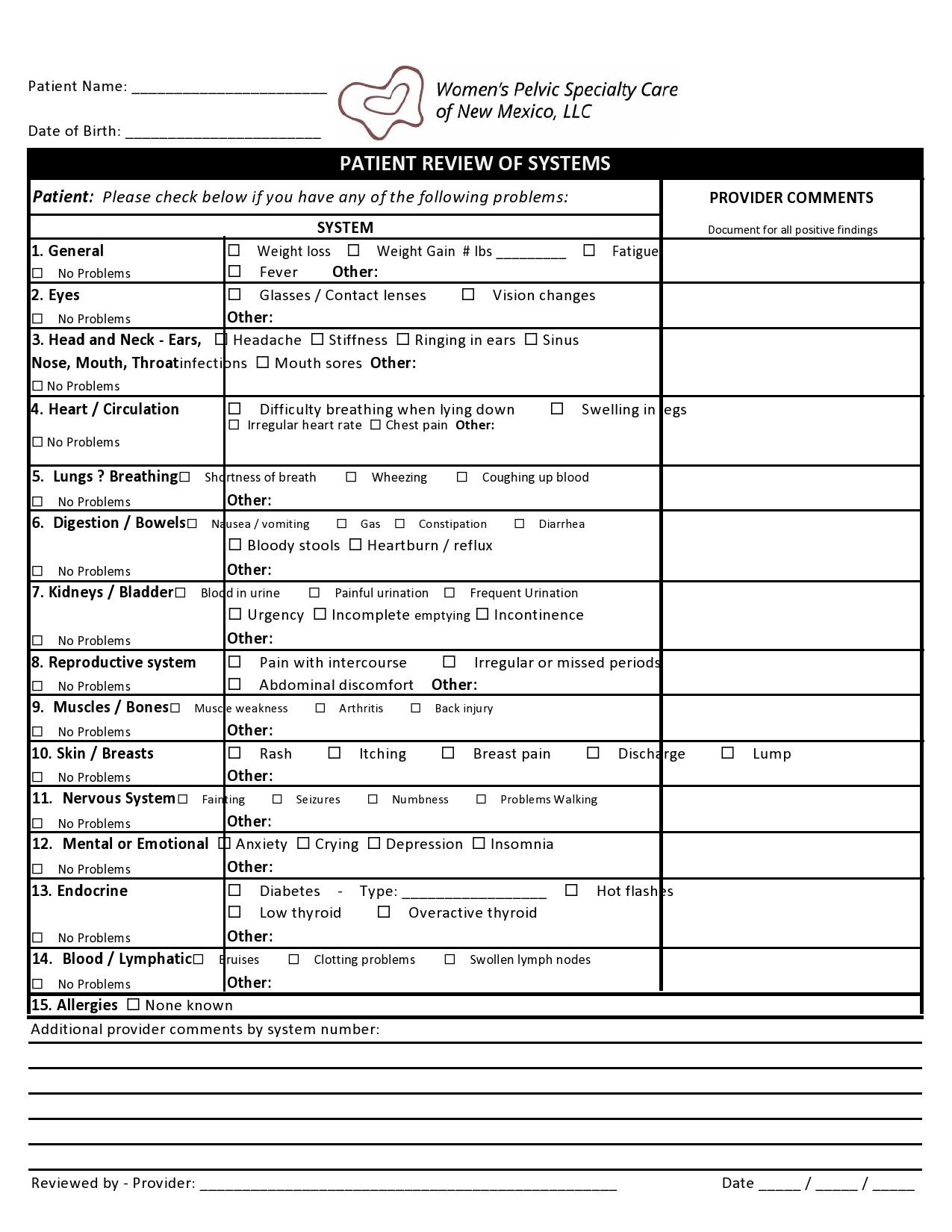
Review Of Systems Examples
The importance of a review of systems template
The definition of a review of systems template by the Evaluation and Management Documentation Guidelines is that “it is an account of body systems obtained through a series of questions seeking to spot signs and symptoms that the patient may experience or has experienced.” Consider these points that show the importance of a review of systems cheat sheet or template:
- The review of systems questions are typically conducted verbally by a physician or the staff through a patient form to find out the patient’s total problem. The process includes an explanation of why there is a need for additional testing, examination, and possible treatment options.
- The review of systems example may focus on the systems directly related to the issues pinpointed in the medical history of the patient’s present illnesses or any other body systems. You can present ROS questions using any format and should include a patient questionnaire form too.
- You may also include elements of the history of present illness (HPI) in the review. However, you should know that is a difference between the symptoms and signs shared by the patient in the HPI and those you acquire from the review of systems checklist. For one, the ROS is very precise. Here, there is always a distinct element of both the separate system review and the HPI.
- The elements of a review of systems example typically reference the signs and symptoms where you would consider both negative and positive comments. Auditors of the review watch for indicators when the medical staff or physician asks questions to the patient.
- The review of systems questions are to be medically required in order to get a complete ROS when the patient comes in for the first time. Some doctors also consider this document medically necessary to repeat the complete review for each follow-up.
Review Of Systems Questions
What is included in the review of systems?
A review of systems template is an inventory of the body systems acquired through inquiries with the purpose of identifying signs or symptoms the patient experiences. There are a total of 14 systems recognized by the Centers for Medicare and Medical Services:
- Allergic/Immunologic
- Cardiovascular
- Constitutional symptoms
- Ears, nose, mouth, throat
- Endocrine
- Eyes
- Gastrointestinal
- Genitourinary
- Hematologic/Lymphatic
- Integumentary
- Musculoskeletal
- Neurological
- Psychiatric
- Respiratory
When it comes to a patient’s medical record, there are several guidelines that you must follow. For instance, one of the key guidelines state that there’s no need for re-documentation if the ROS acquired during the initial encounter shows evidence that the doctor performed a review and updated the patient’s information.
You can document the review process and the updated information by describing if there was is a new review of systems template. You can also note that there hasn’t been any change in the patient’s information. Another guideline that you need to remember is that any member of the staff may document the ROS in medical records as long as evidence exists that the physician performed a review.
You must indicate the date of your review of systems checklist if you refer to it in your most current notes. You cannot say that the ROS remains unchanged from the previous visit without providing a date. If you also use a History Table, you can choose from the following levels:
- A ROS that’s “problem pertinent” inquires about the system that’s directly related to the issues indicated in the patient’s HPI. Documentation should include the pertinent negatives and positive responses for the system-related problems.
- A ROS that’s “extended” inquires about the system that’s directly related to the issues indicated in the HPI along with a few of the body systems. The documentation must include the pertinent negatives and positive responses for 2 to 9 systems.
- A ROS that’s “complete” inquires about the system that’s directly related to the issues indicated in the HPI along with all of the body systems. You should review at least 10 systems and provide individual documentation for those systems with pertinent negatives and positive responses.
Take note of the wordings you use for each of the levels mentioned above. That way, your ROS questions can be directly related to the patient’s problems.
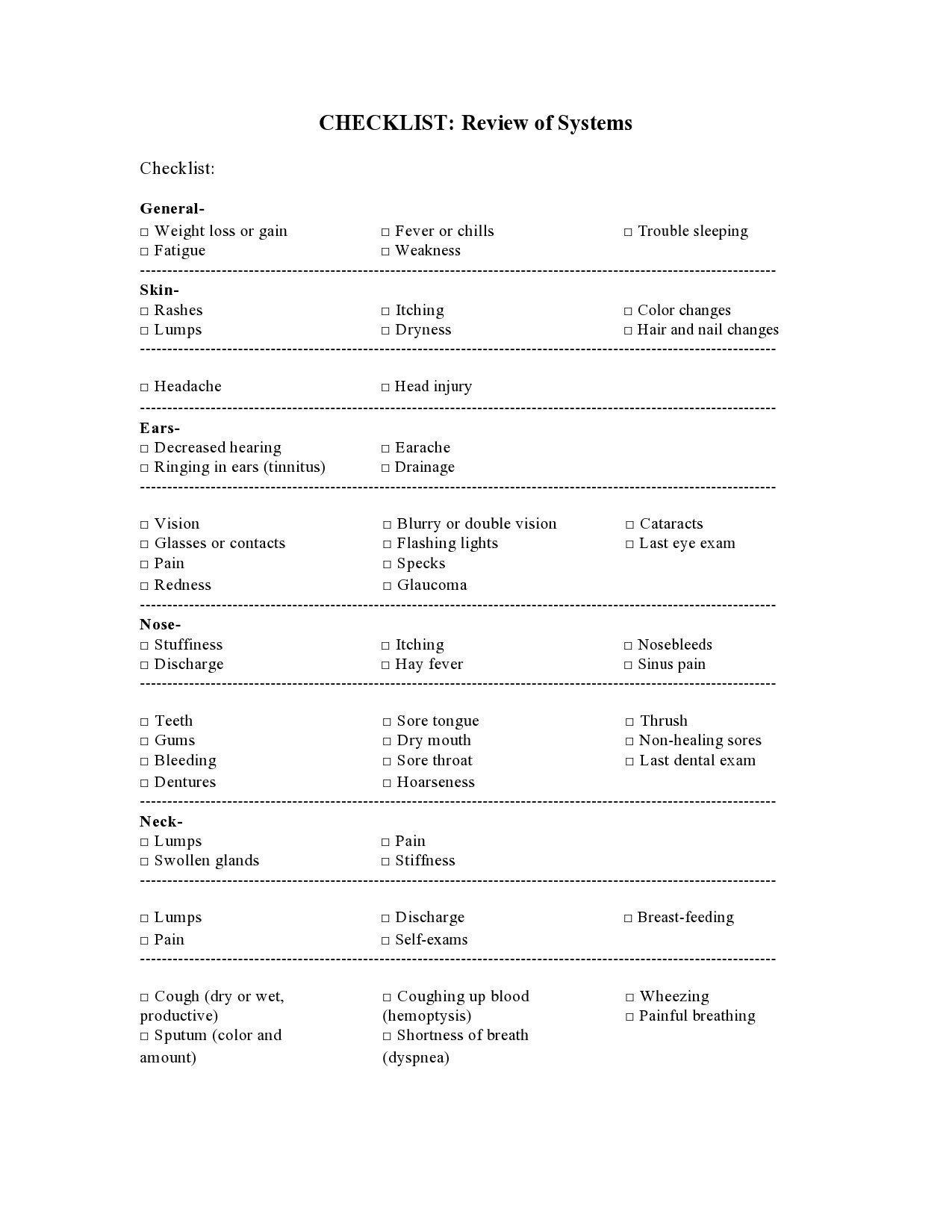
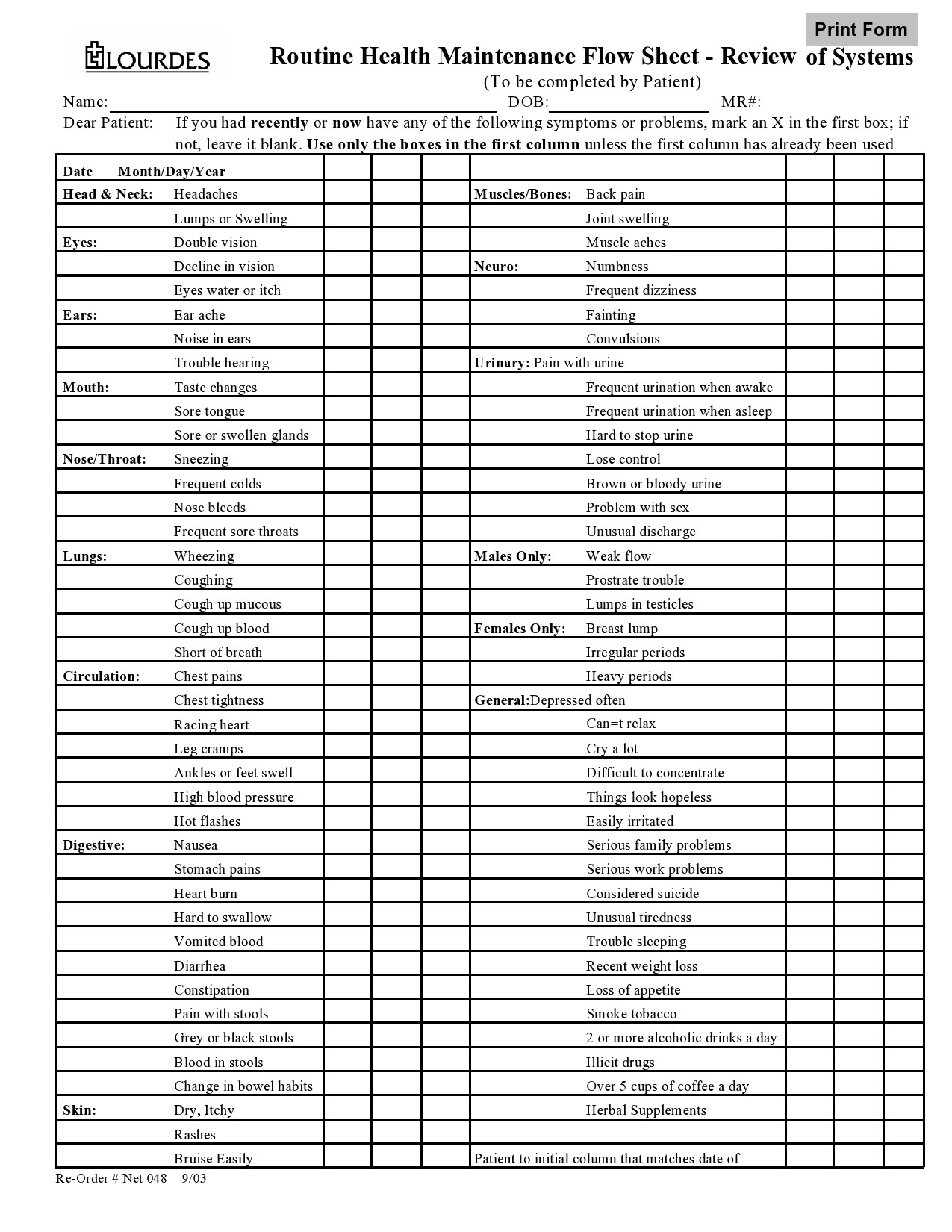
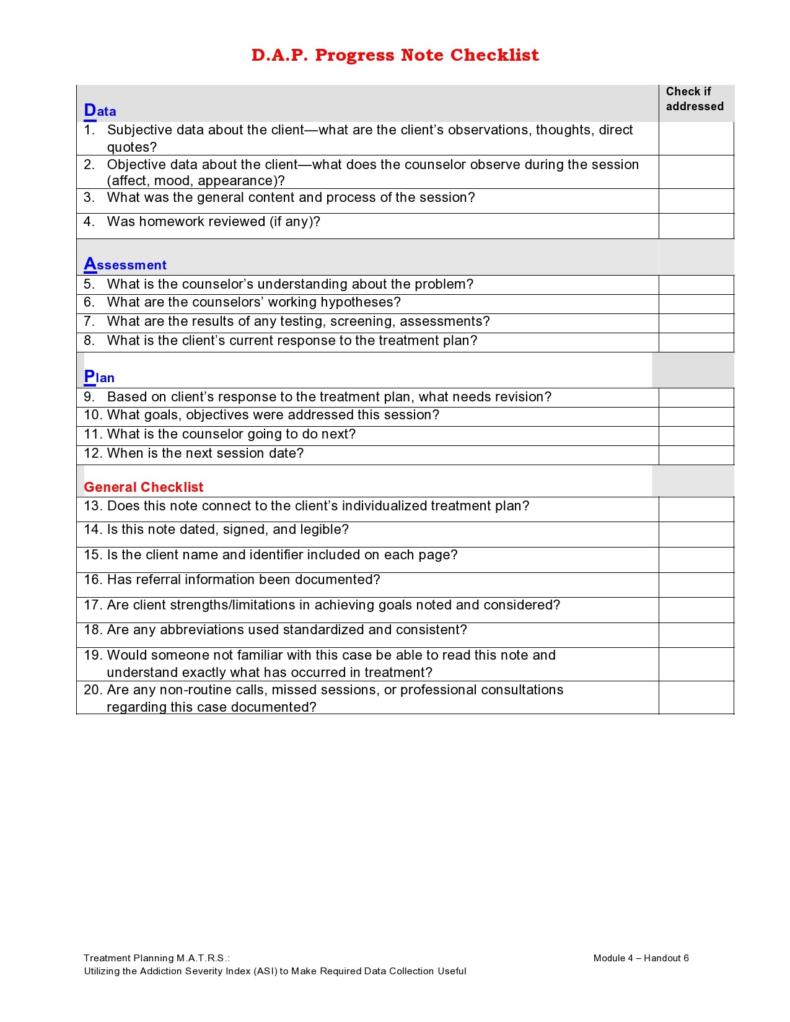
Review Of Systems Checklist
Applying a review of systems template
You can also consider a ROS as a list of questions arranged according to organ system. It’s designed to reveal disease and dysfunction. This is a very important document as you can use it in a number of ways:
- As a tool for screening for each patient that the clinician encounters.
- Ask ROS questions only to patients classified under a specific risk category. For example, reserving questions are only for determining occult diseases of the prostate of men aged 50-years-old and above.
- To better establish the most probable causes of a present symptom as described by the HPI section. For example, doctors can ask patients experiencing chest pains detailed pulmonary and cardiac ROS questions.
So, what is the best way to use a review of systems cheat sheet? It’s best used as a screening tool for broad applications. When you use it this way, the following statements would hold true:
- The questions to ask would reflect a range of important and common clinical conditions.
- These disorders could go undetected if the patient wasn’t prompted specifically.
- Identifying these conditions has a positive impact on mortality or morbidity.
Unfortunately, there is little evidence that supports these assumptions except for the few very specific screening tools. In fact, even the positive responses to an ROS screening aren’t very clear in their significance. These might even create more problems by creating additional questions and low-value testing results to make the matters complex.
Because of this, many clinicians are in-favor of a more thoughtful and targeted application of ROS questions based on specific patient characteristics like sex or age and risk factors like history of diabetes to vascular ROS questions. This approach is more revealing and efficient. The more experience you gain, the more you can make informed decisions about how to use the ROS into your strategies for patient care.
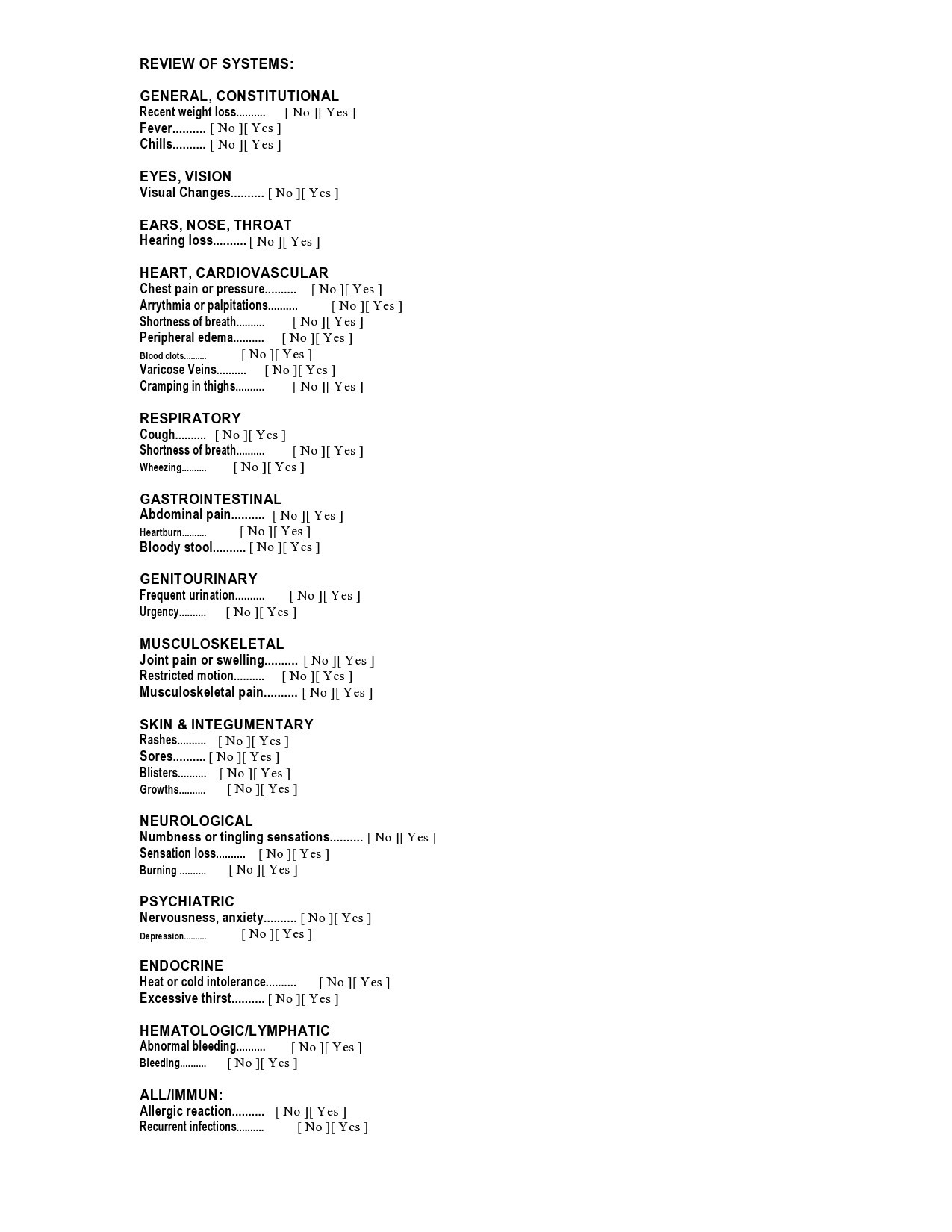
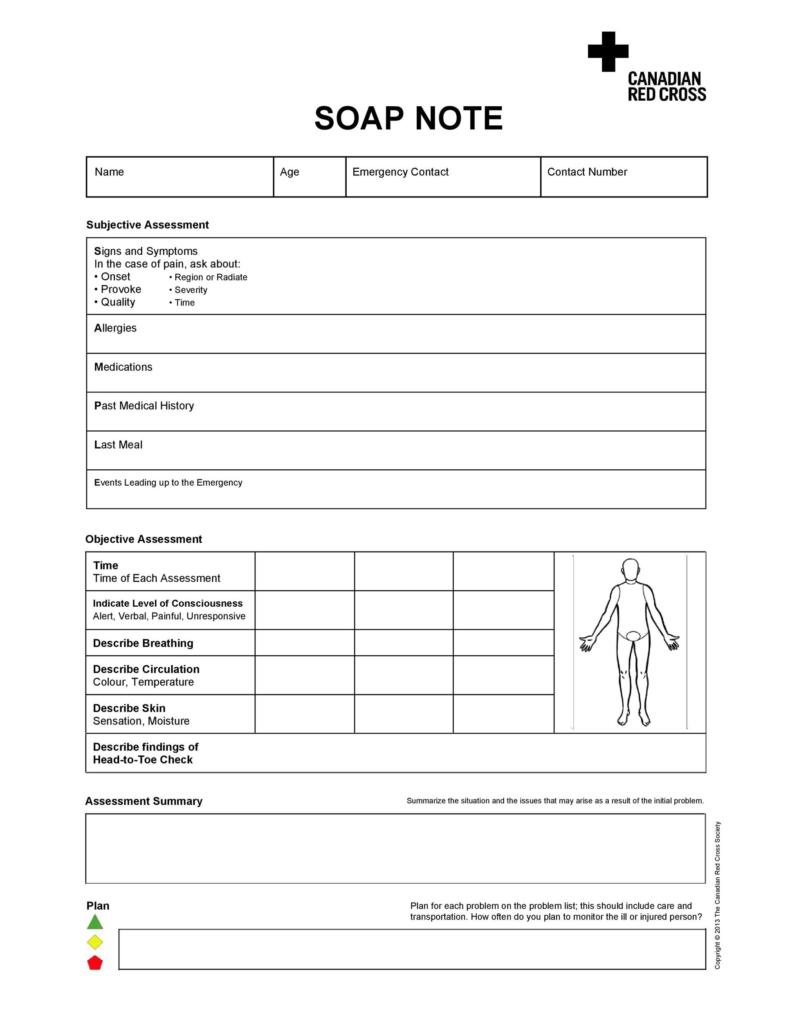
Review Of Systems Cheat Sheets
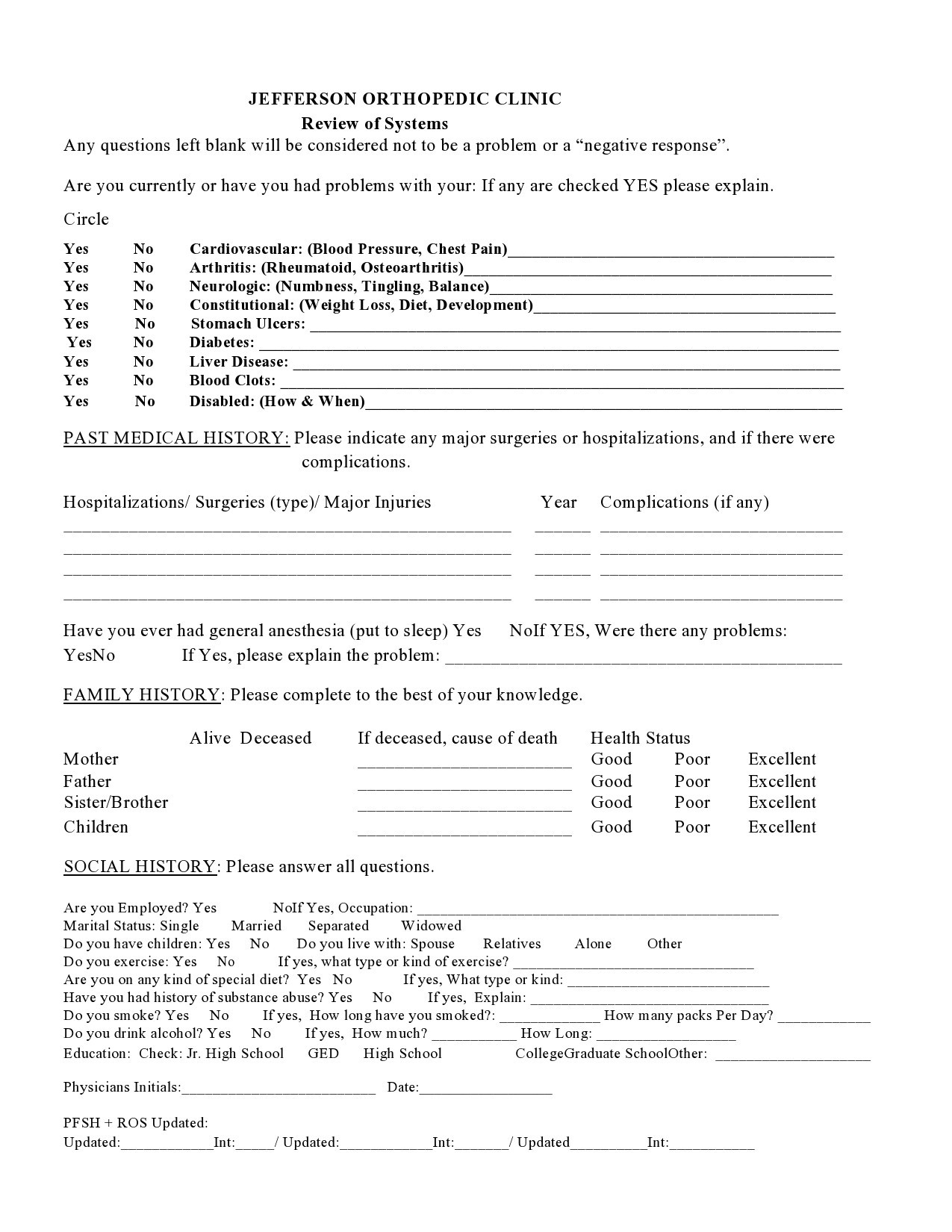
The difference between a review of systems and a history of present illness
In summary, the review of systems template is an inventory of body systems obtained through questions needed to find out identifying signs and symptoms that the patient experiences or has experienced. Then there are the three levels of a ROS that we had already gone through: the problem-pertinent ROS that involves the review of one system, the extended ROS that involves the review of 2 to 9 systems, and the complete ROS where the documentation should indicate the review of 10 or more body systems.
Although ROS and HPI can have similarities, the former differs from the latter because it includes queries related to the body systems. Here are some points that explain the difference between the two:
- Documentations of ROS must show that the physician asked a question to the caregiver or the patient. In cases where the notes don’t have their own ROS section, you should search for specific terms that indicate that the caregiver or patient answered the questions the provider asked.
- In the determination of whether to consider a history element as either an HPI or a ROS, give the credit to ROS but only if the provider did pose the question. You should only count each word or phrase should once, otherwise, you would do what’s known as “double-dipping,” where you would count something under both ROS and HPI.
- You can meet the documentation requirements for a complete ROS only if all pertinent negatives, positive responses, and a statement that includes the words “all,” “complete” or “remainder” get documented.
- Always remember that you can gather ROS through the questions asked either through a questionnaire or through verbal communication. Do not count a word or phrase under both HPI and ROS. If it appears that the information got obtained through a question asked, then count it as a ROS.