Anytime you visit a therapist, you will notice they keep jotting notes from time to time. Throughout the session, the therapist will ask questions and as you answer, they record important information. Some people might feel uncomfortable with this but there is nothing to worry about. The therapist wants to learn a lot about you to be able to help you. You may have several reasons that brought you to their facility and they want to be of great value to you. The next time you visit, they want to have a starting point for progress. It is okay to be curious and want to know the purpose of the notes.
Table of Contents
- 1 Therapy Notes Templates
- 2 Why do therapists take notes?
- 3 Therapy Notes Examples
- 4 Can the therapist’s notes be recorded in medical records?
- 5 Why do therapists require a counseling notes template?
- 6 What needs to be in a therapy note?
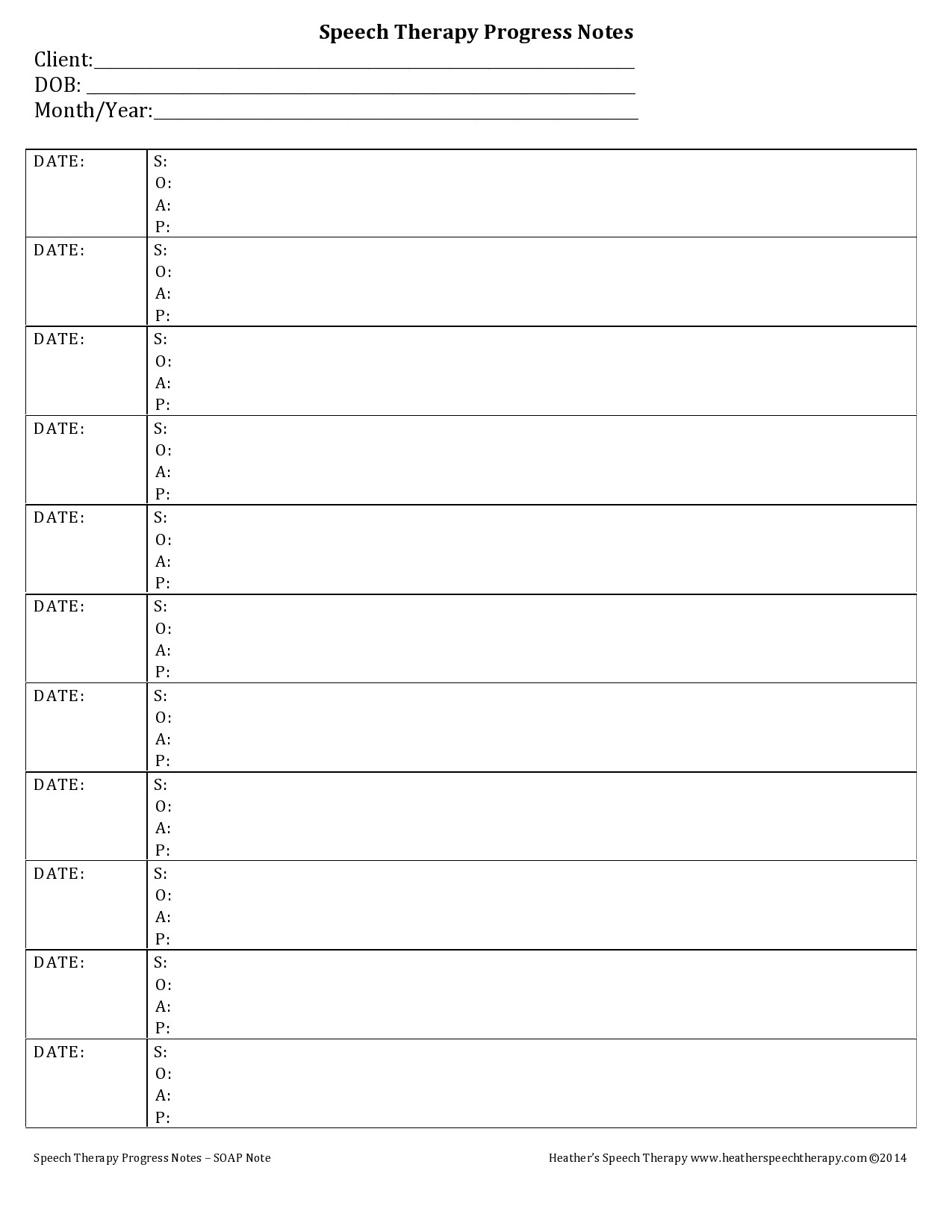
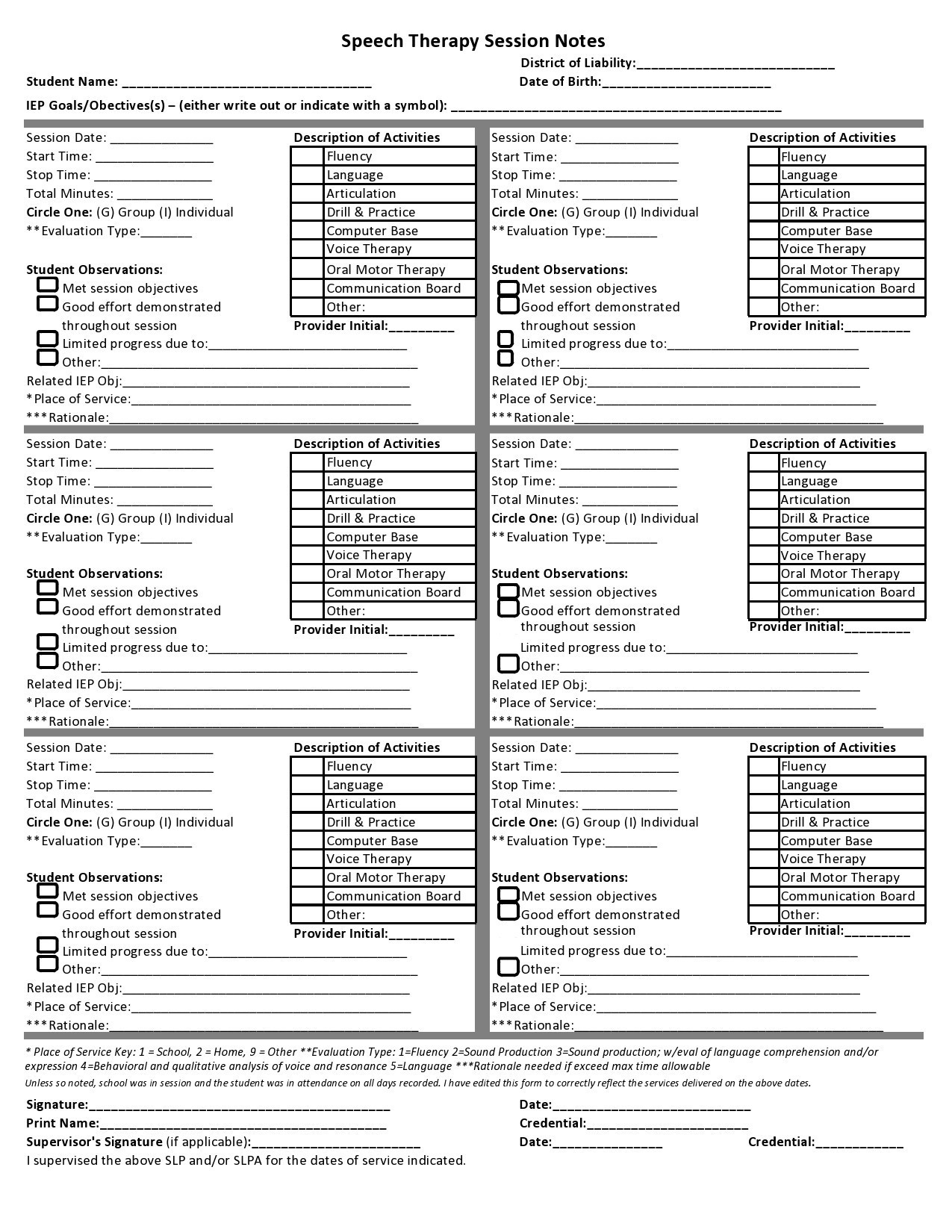
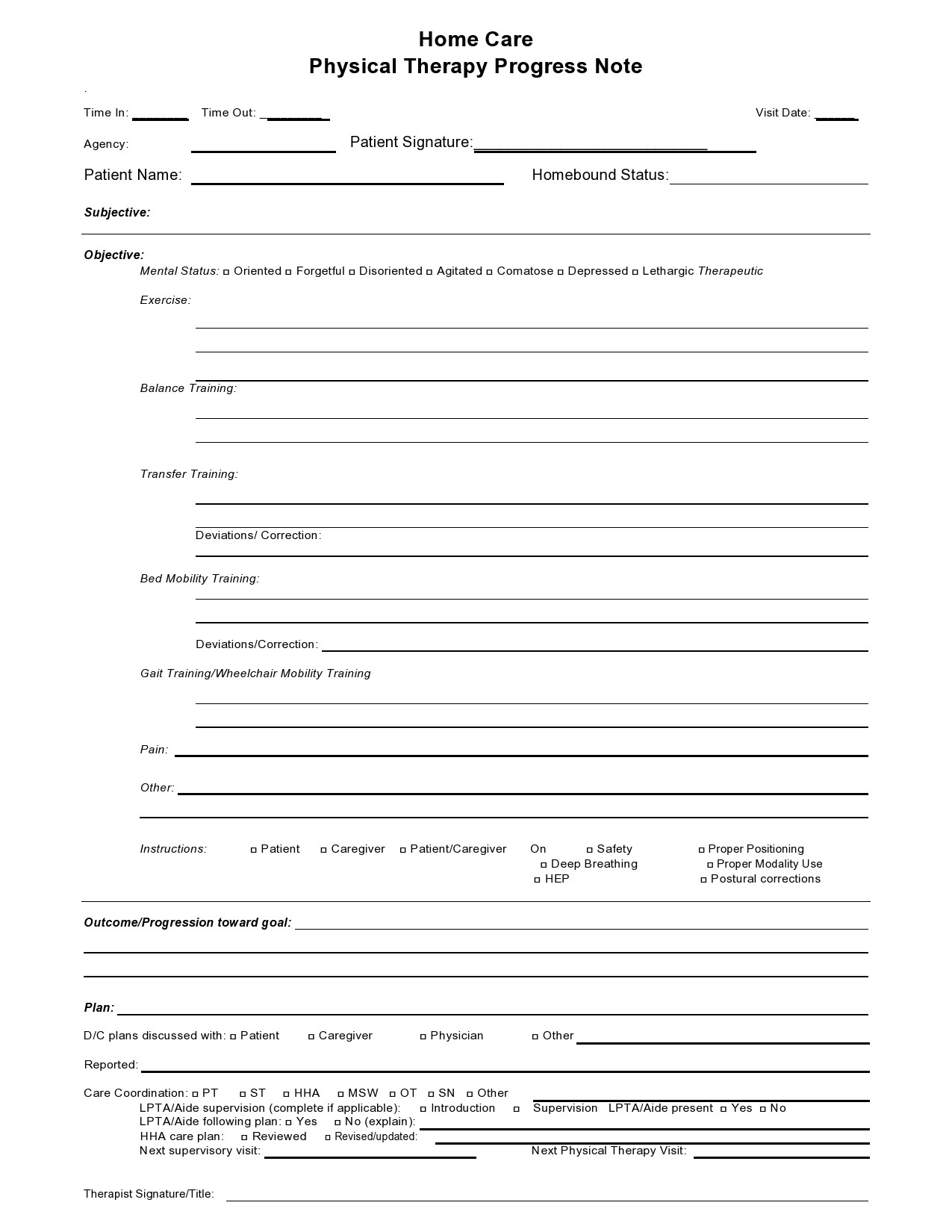
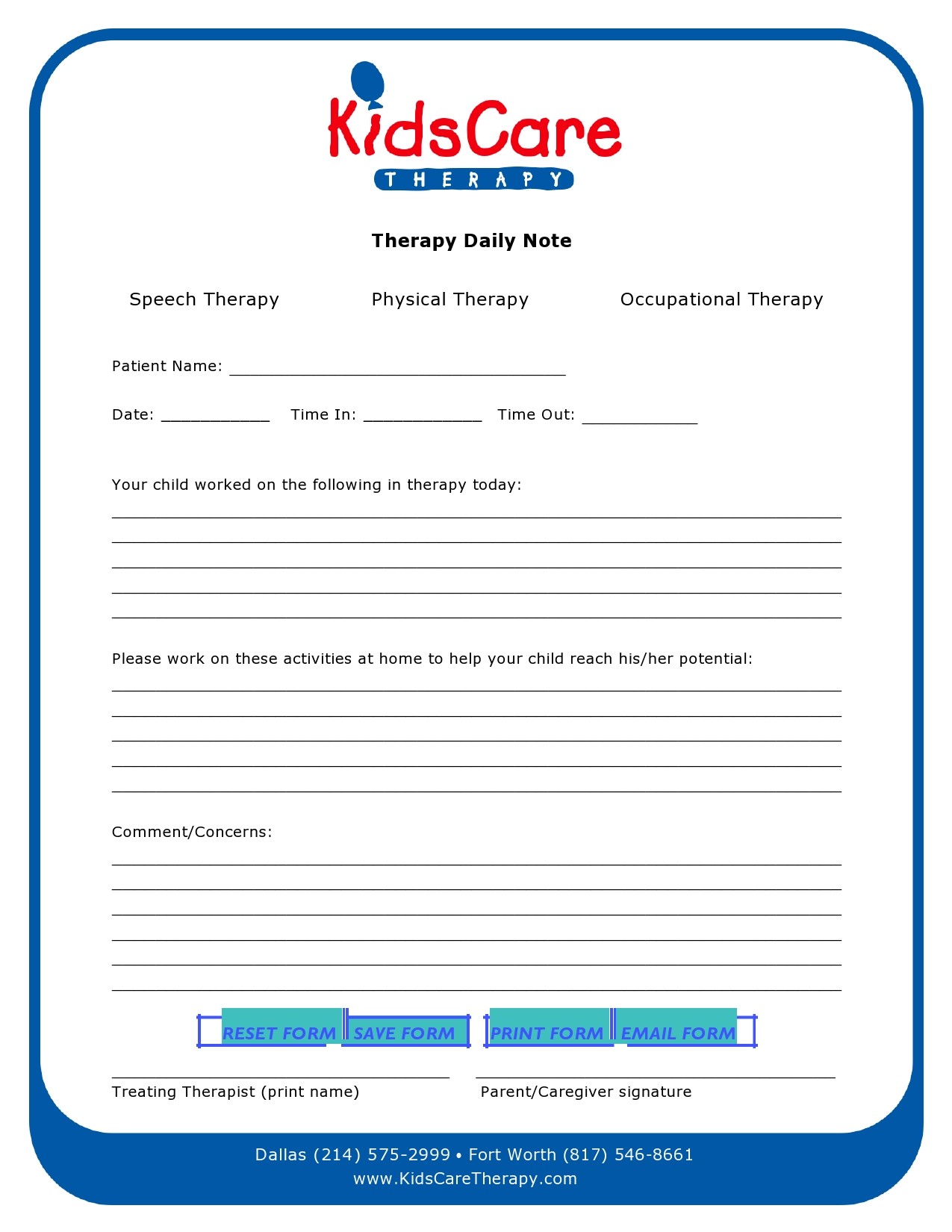
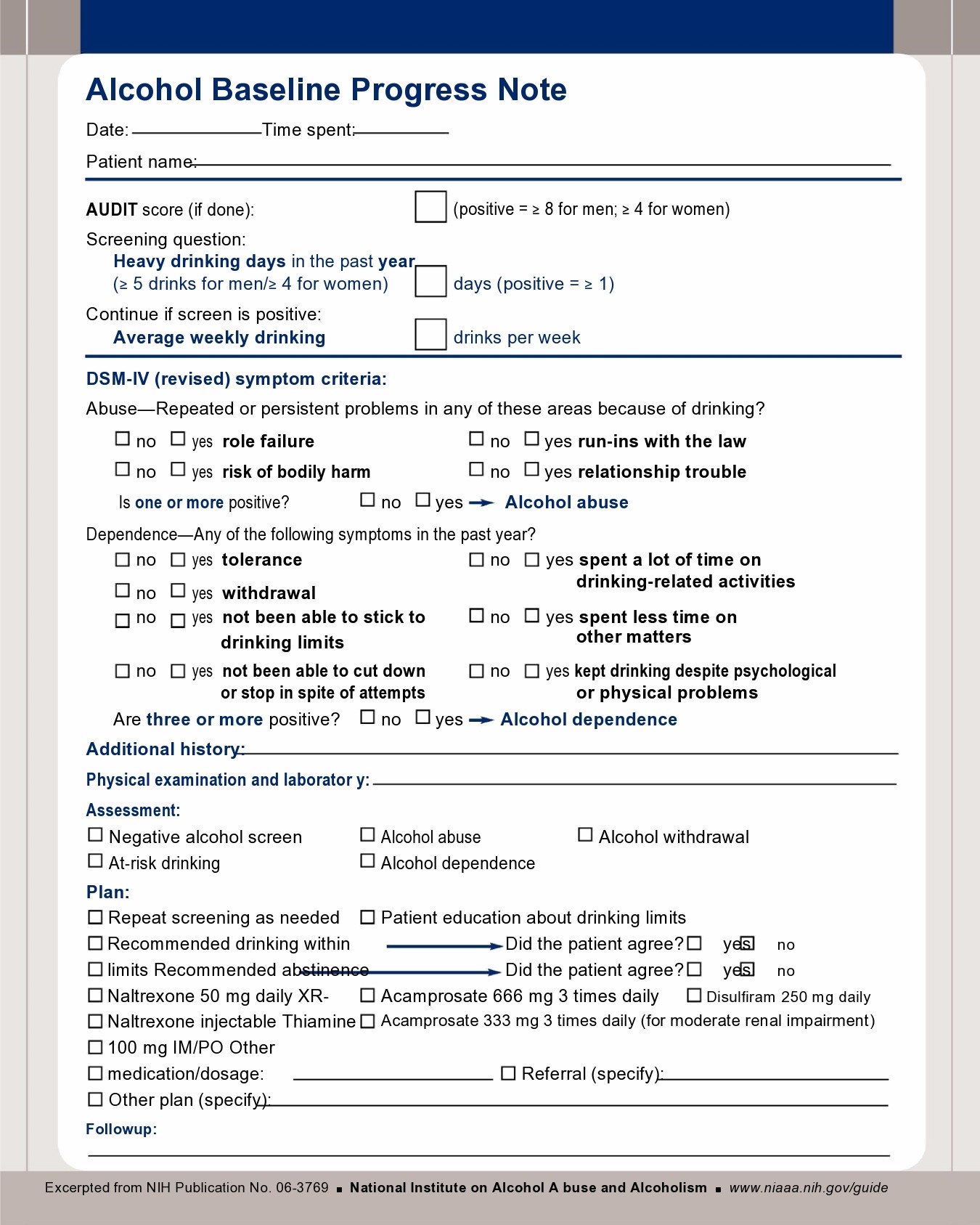
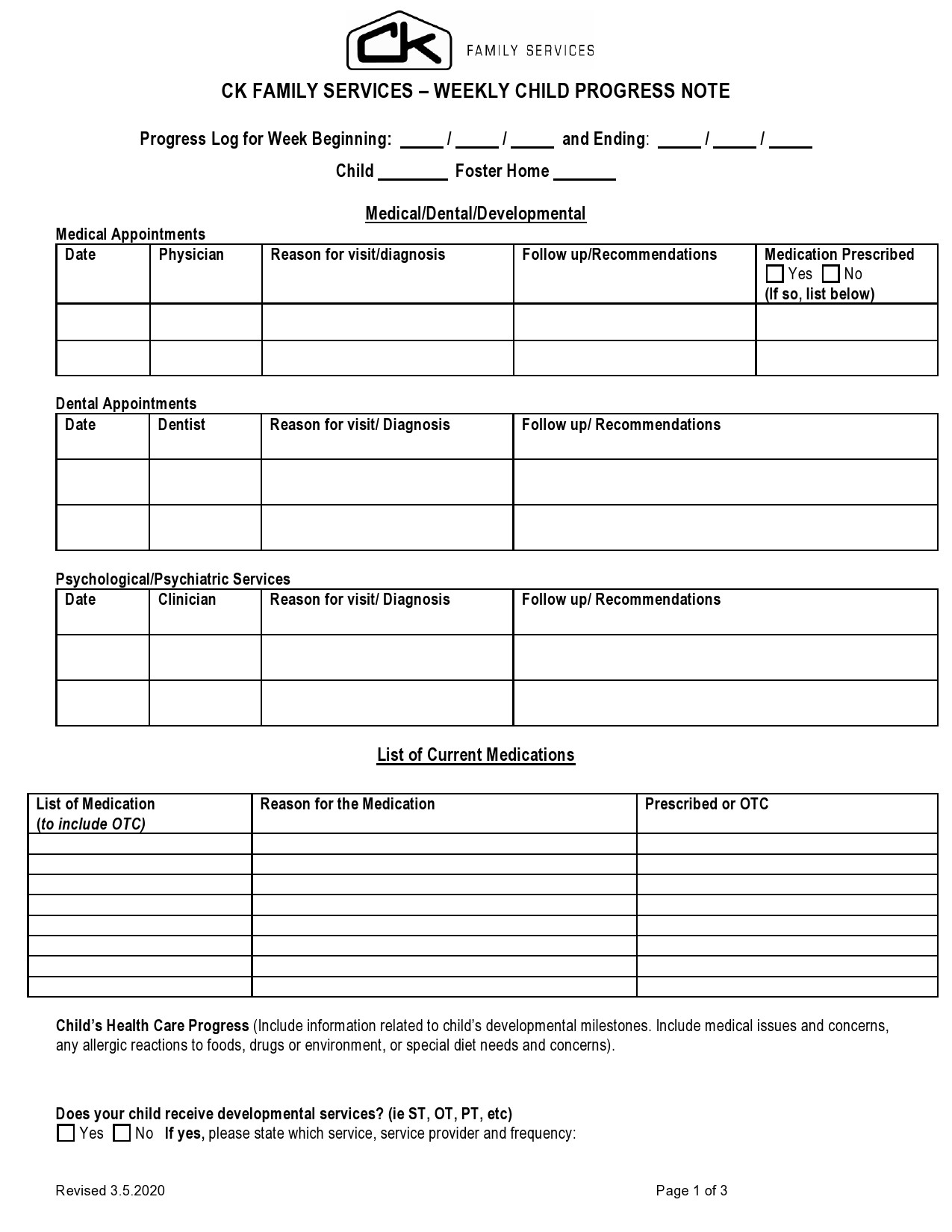
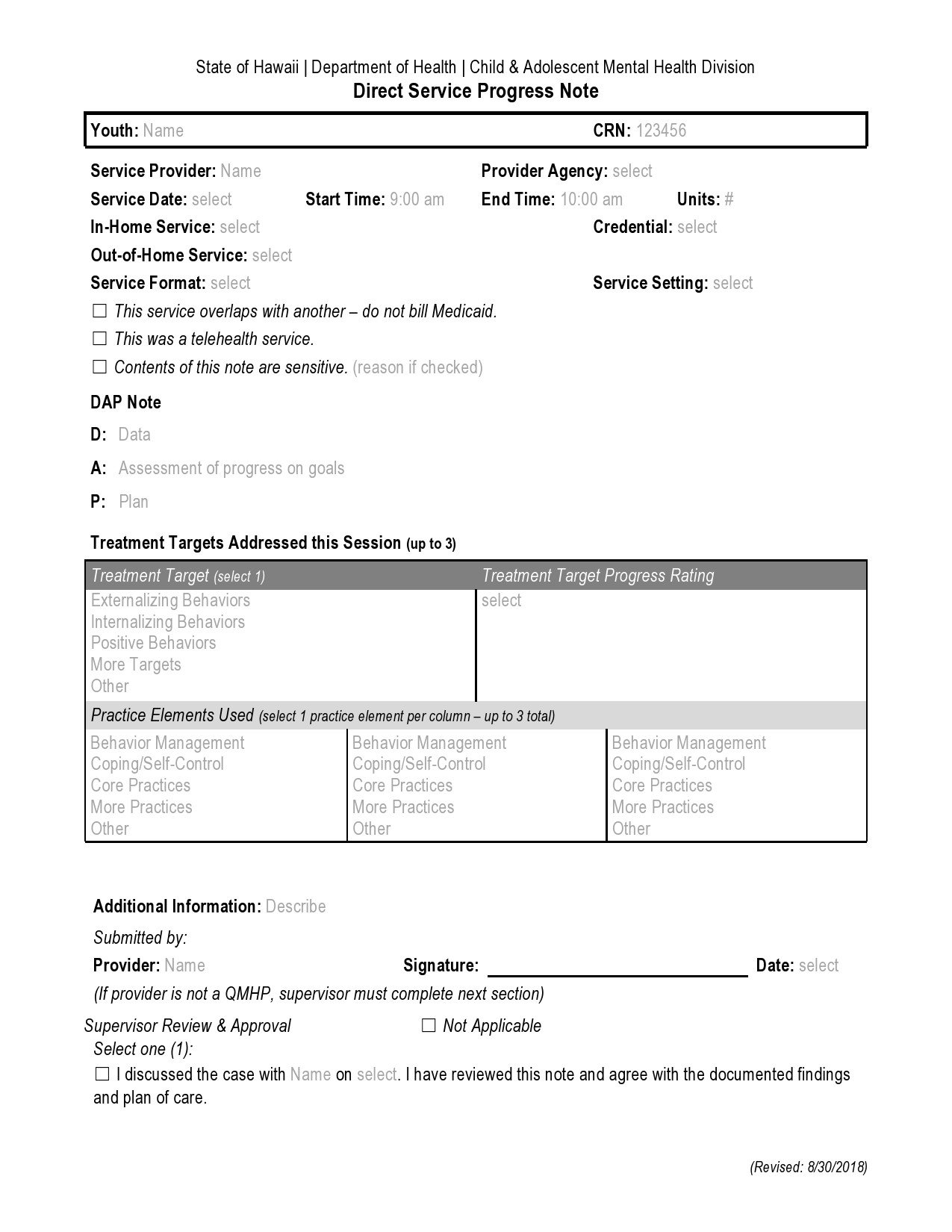
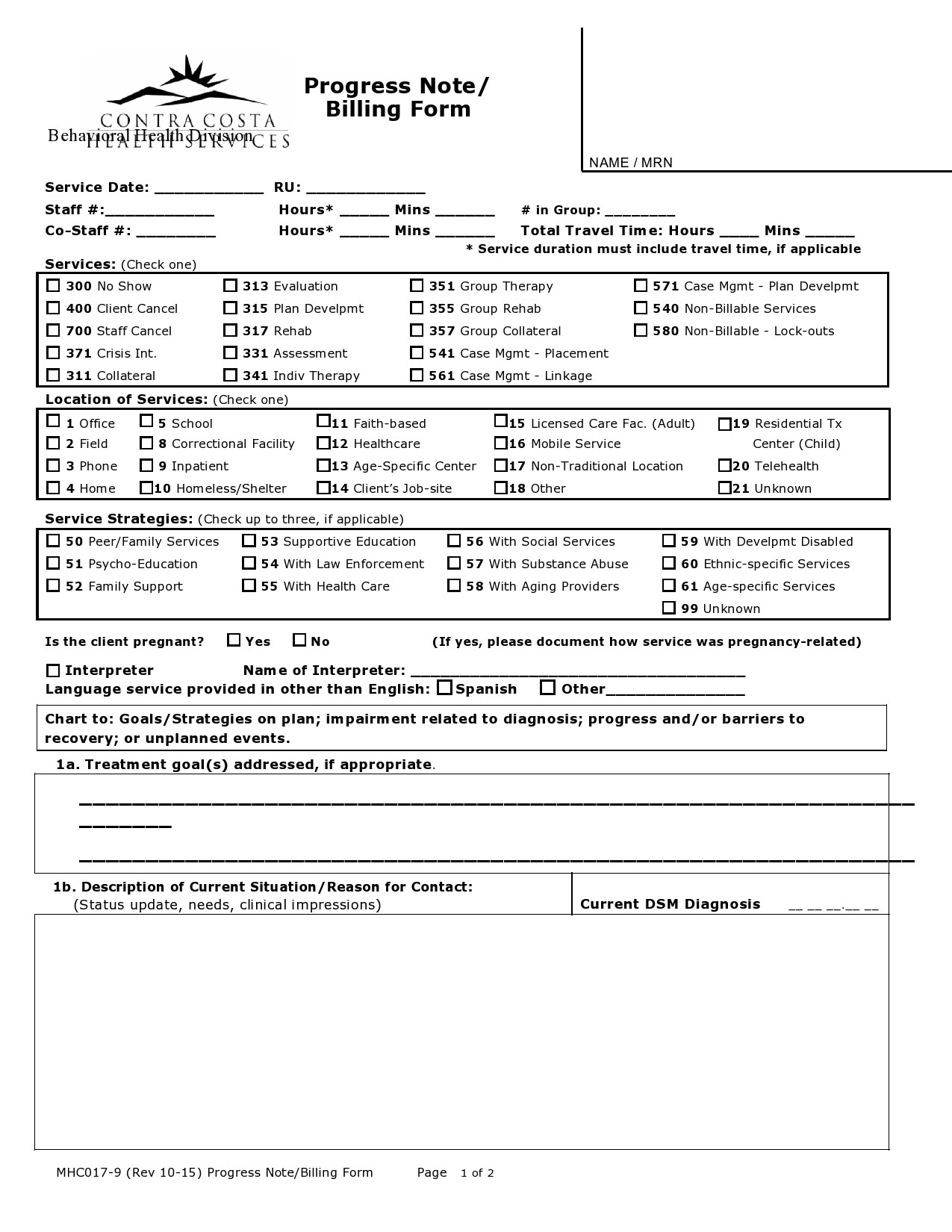
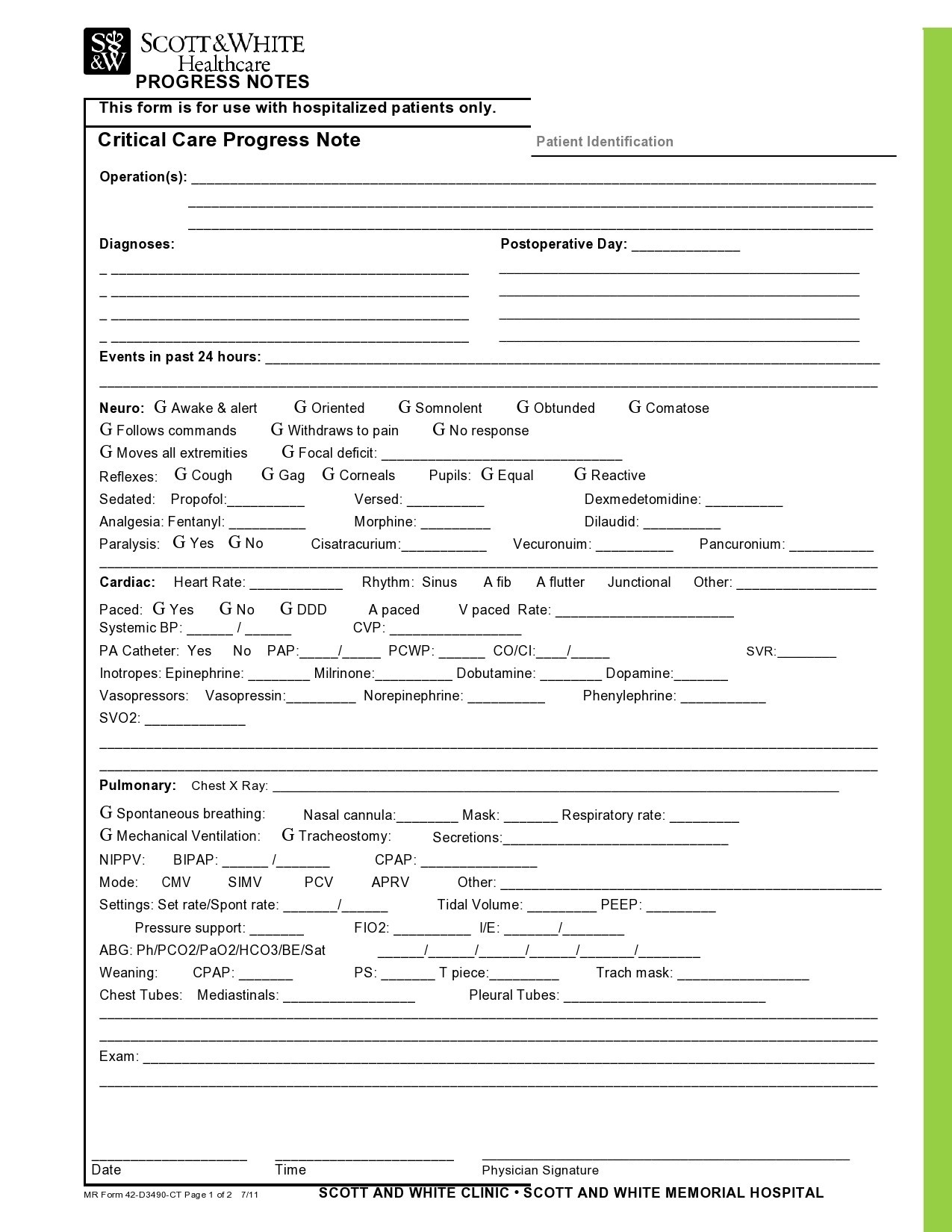
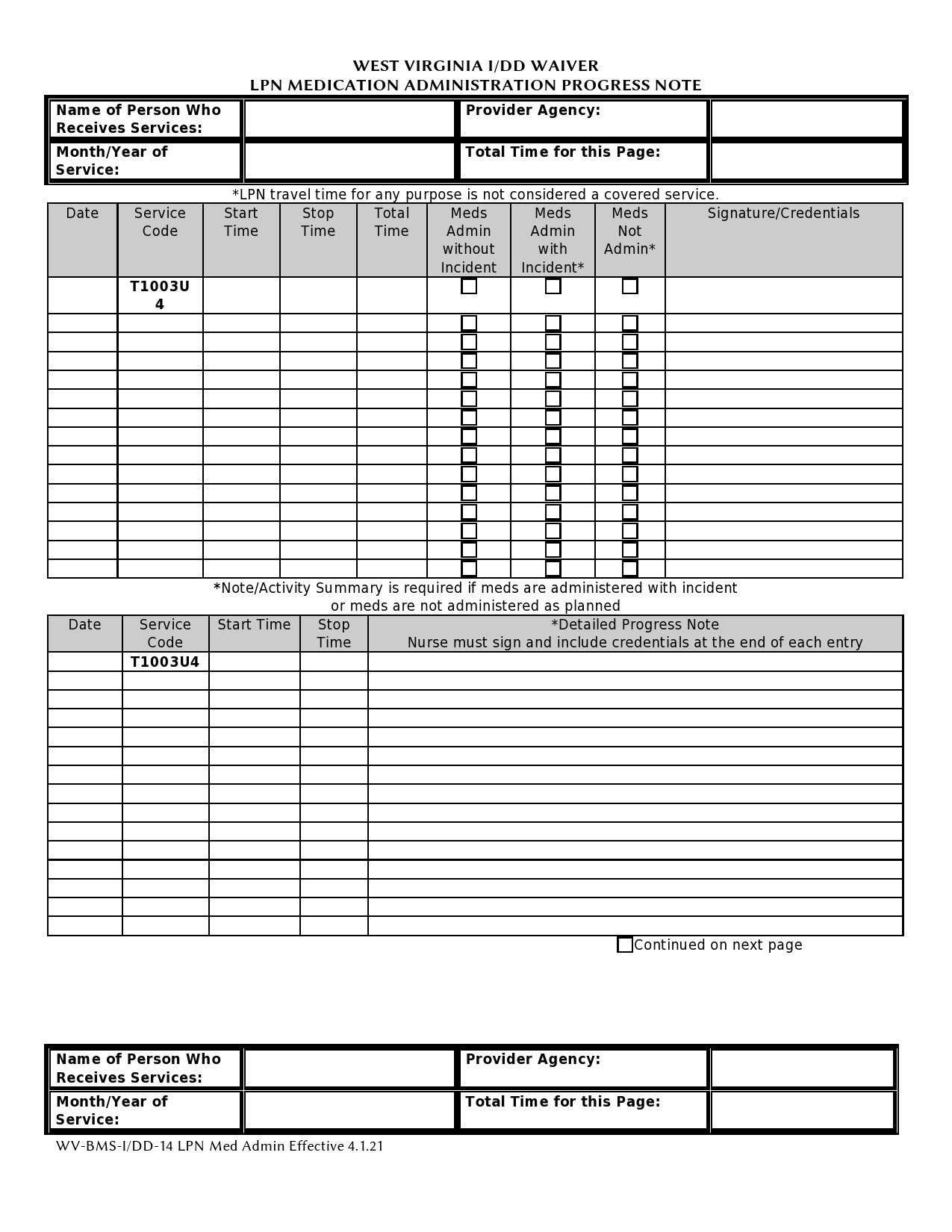
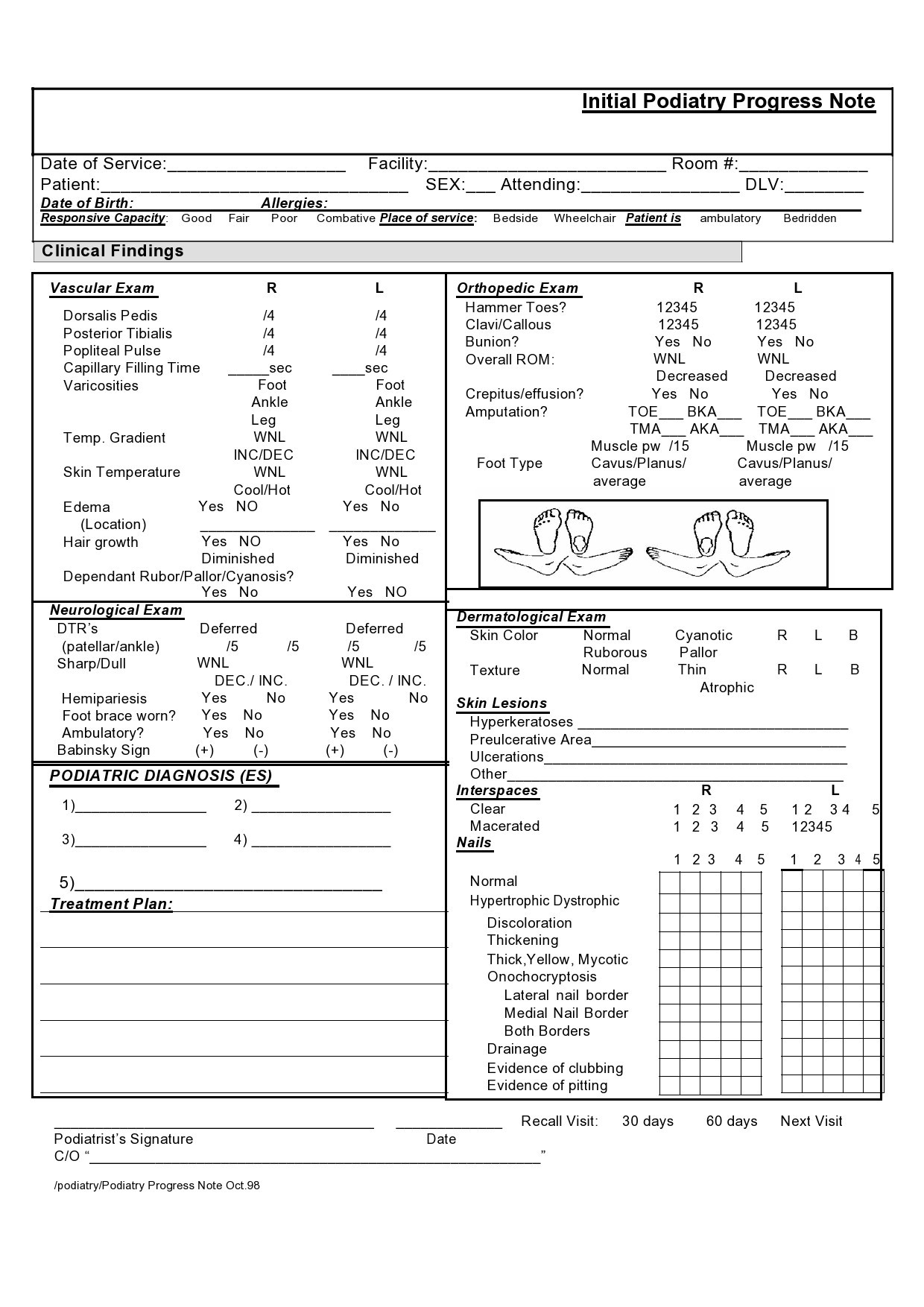
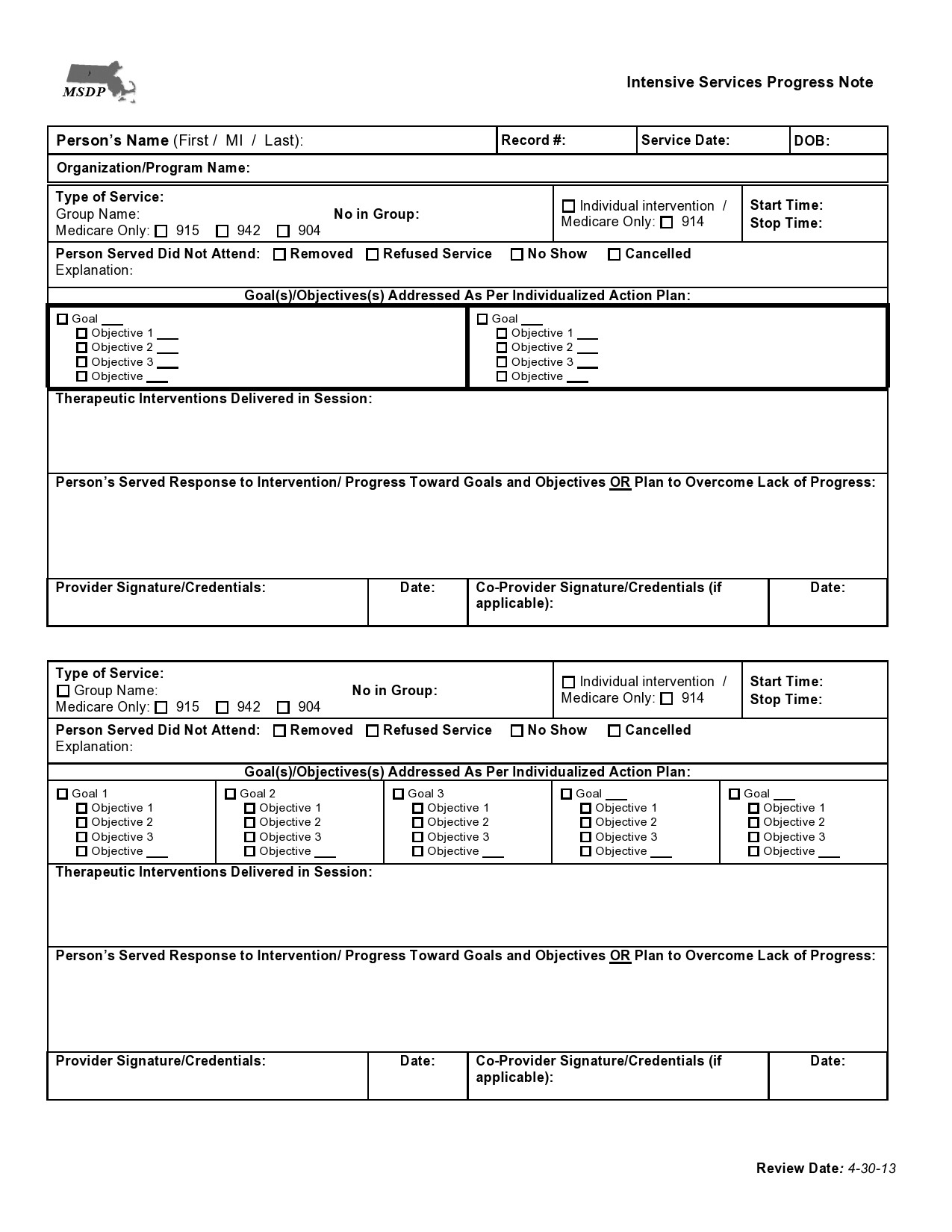
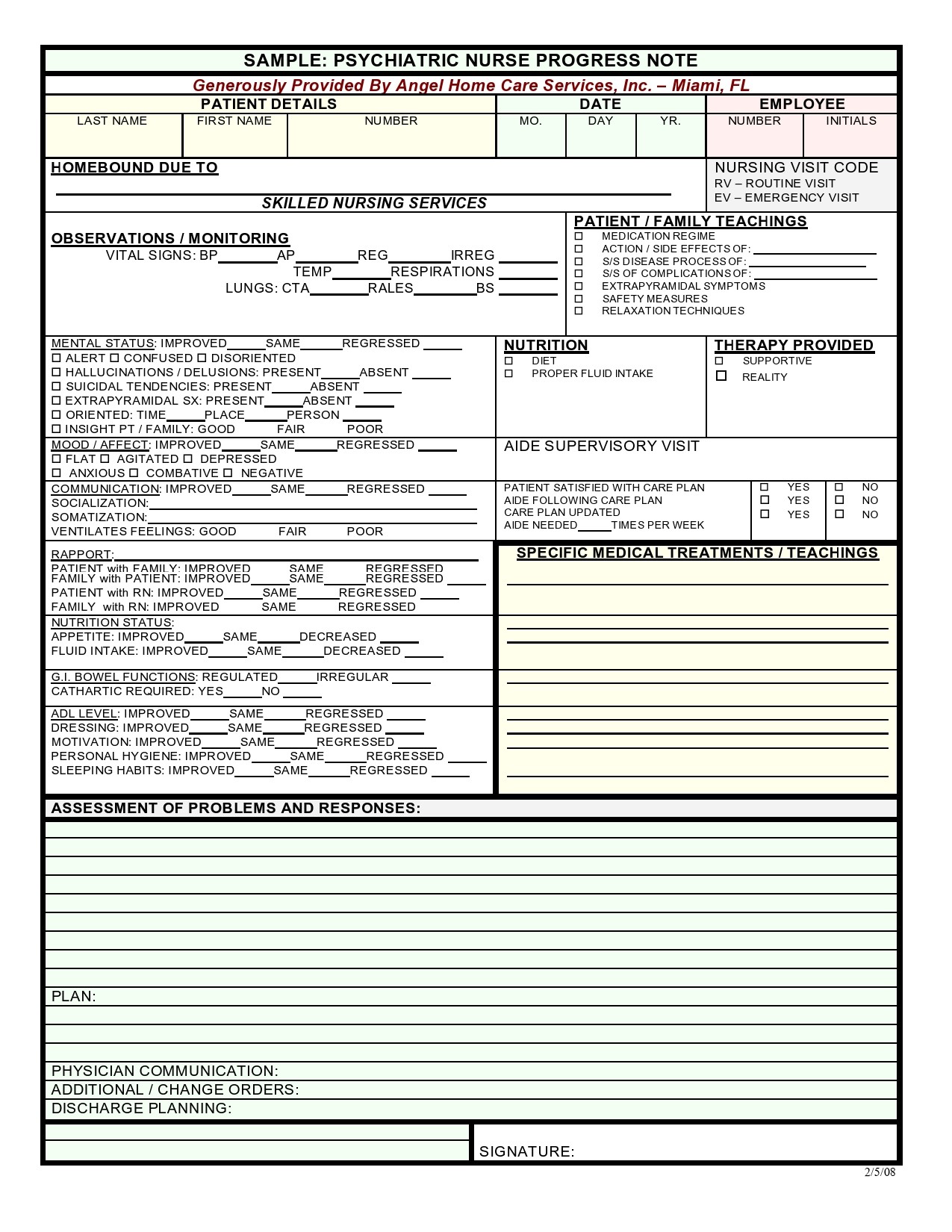
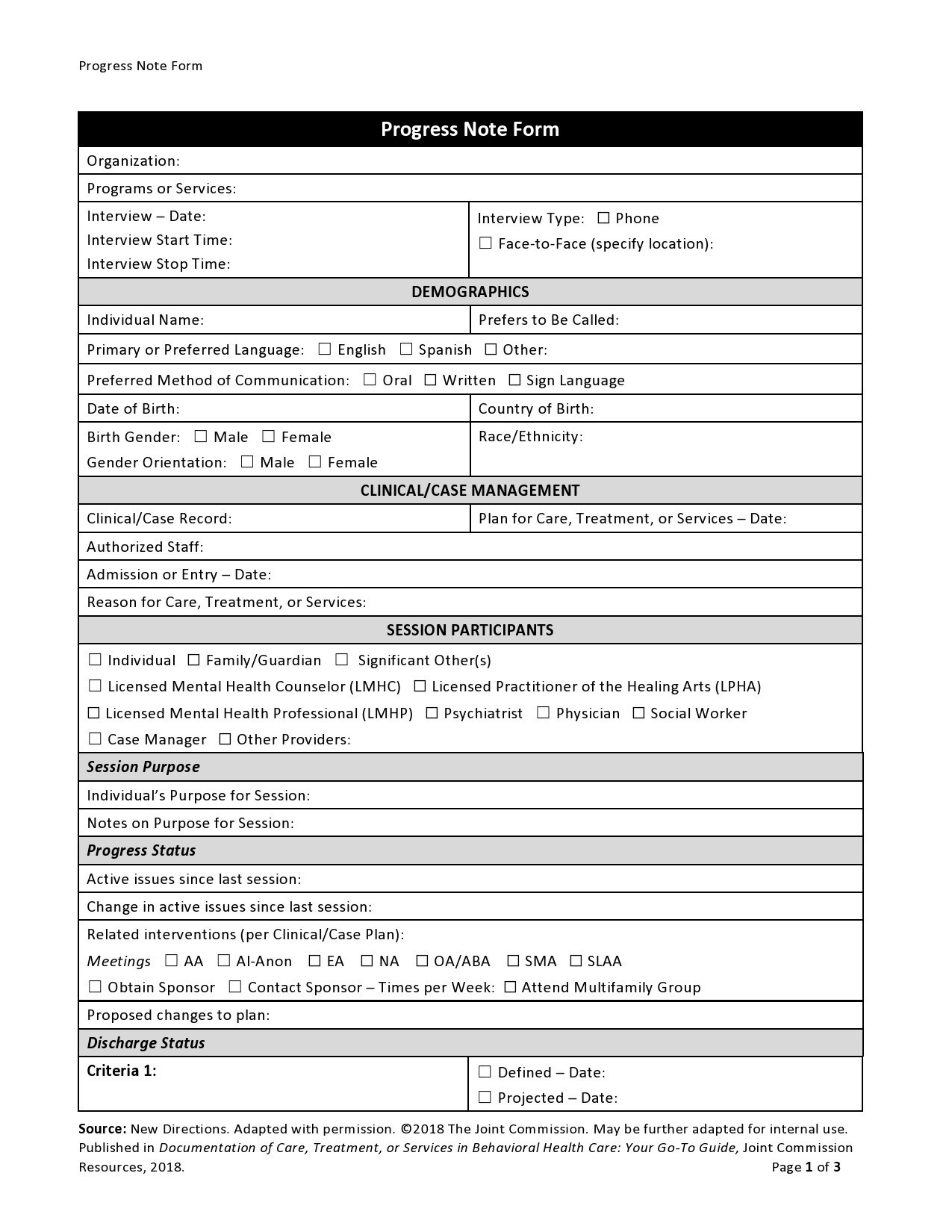
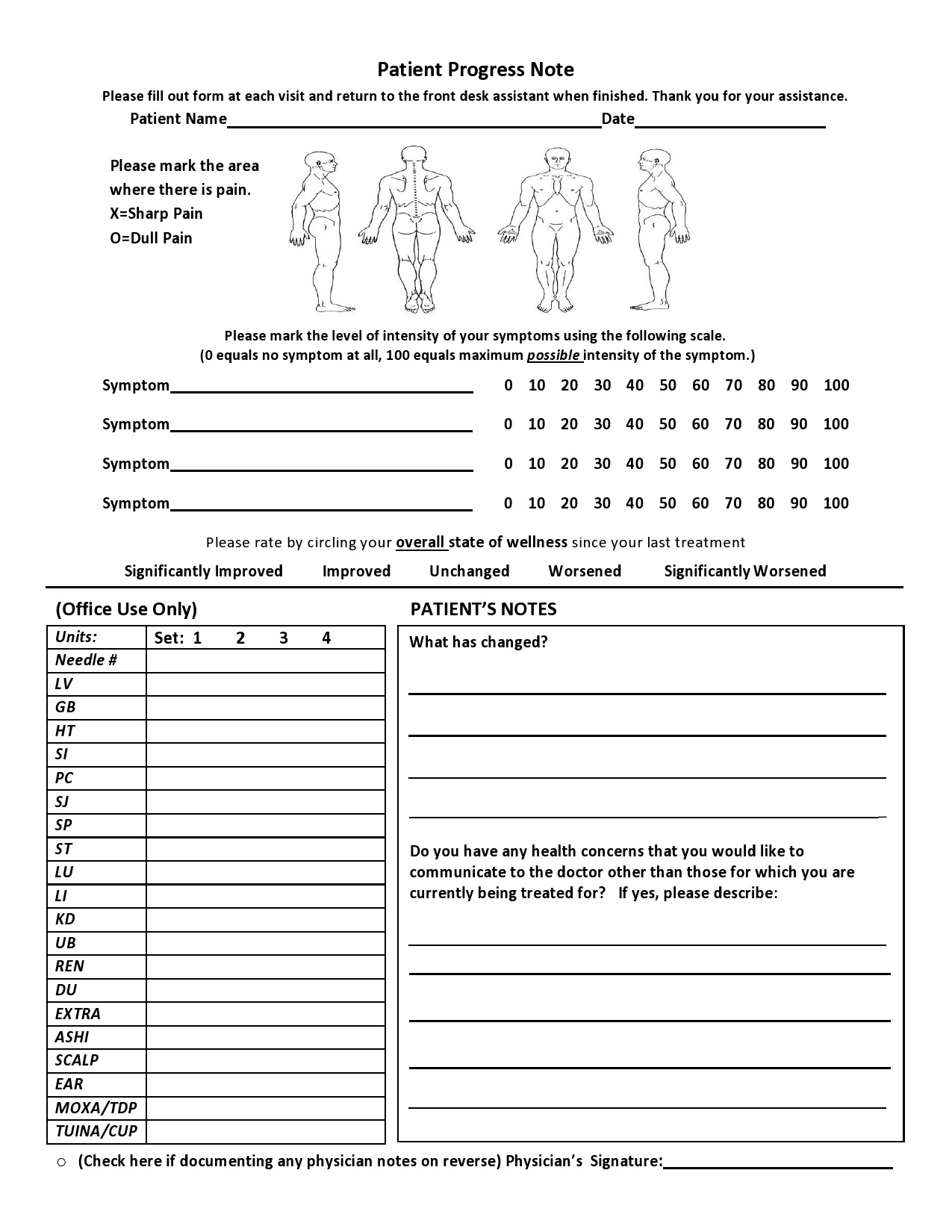
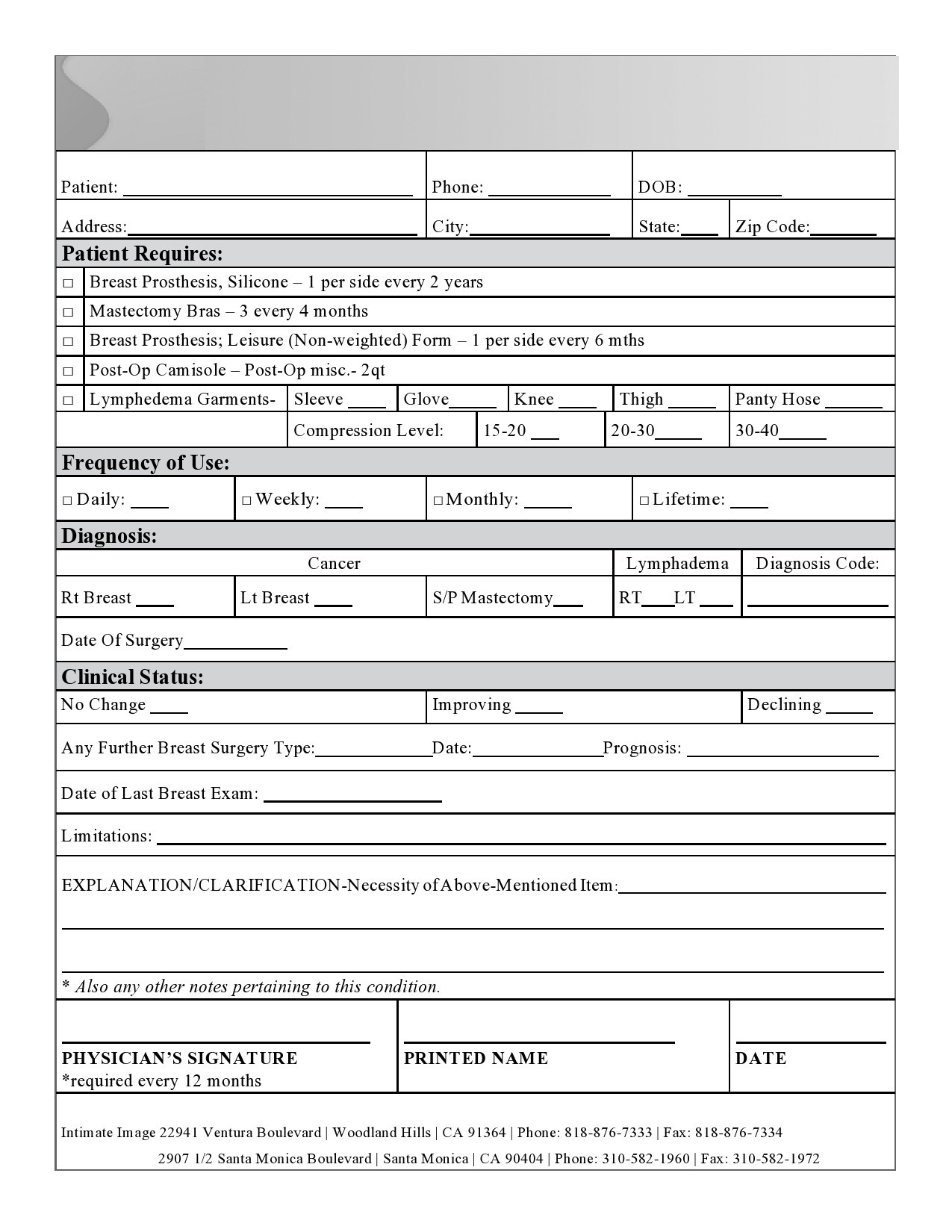
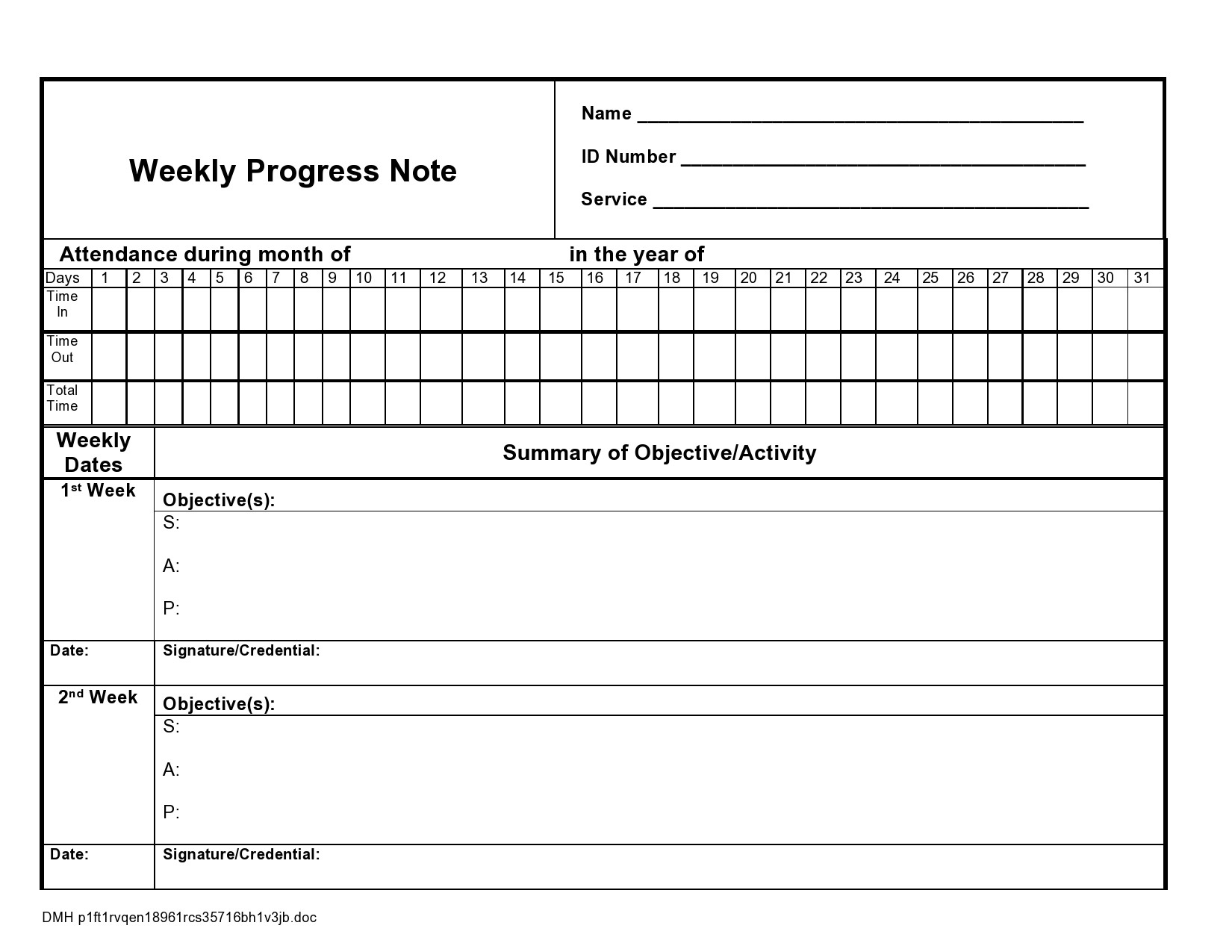
- 7 Progress Notes Examples
- 8 How do you write a therapy note?
- 9 The common types of session notes
- 10 Counseling Notes
- 11 Other categories of therapy session notes
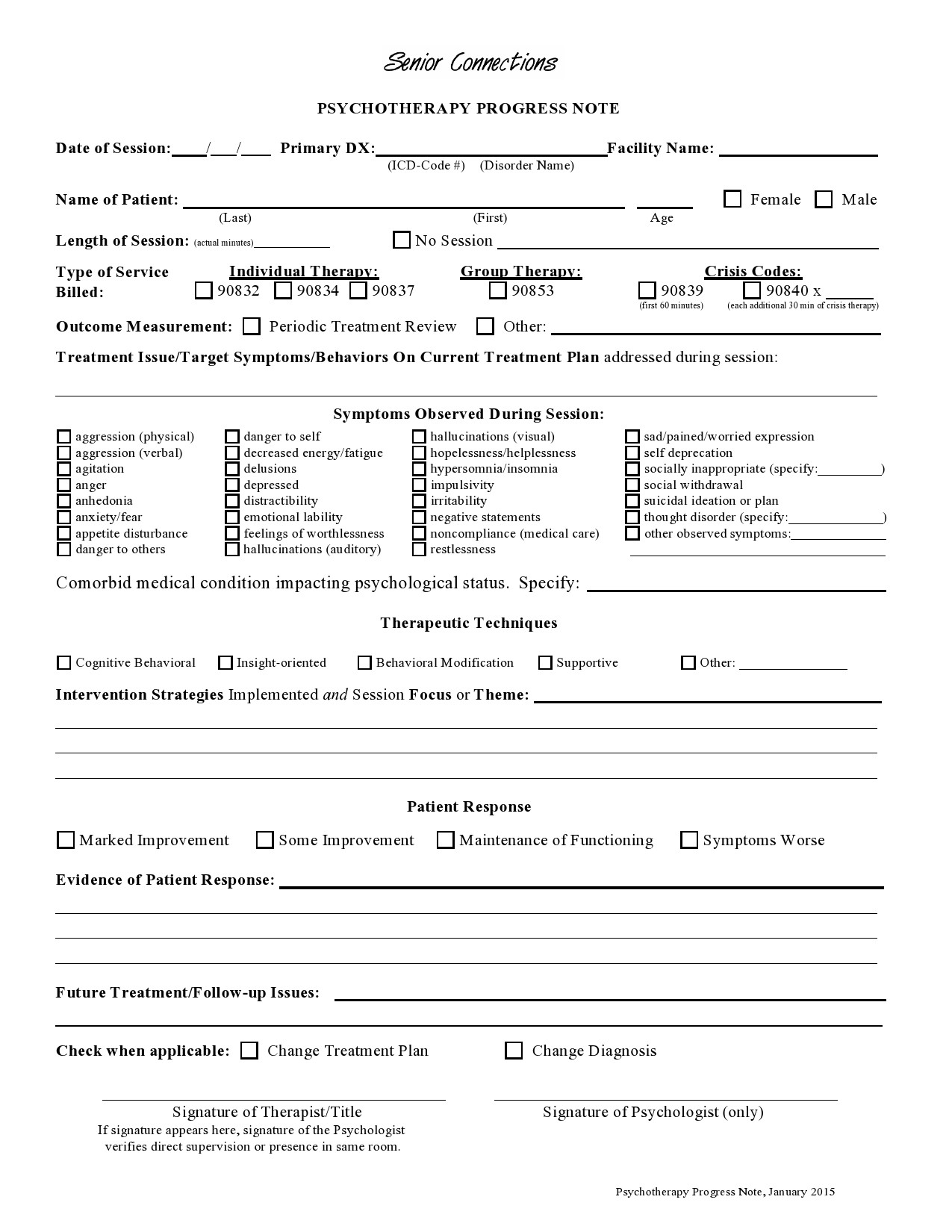
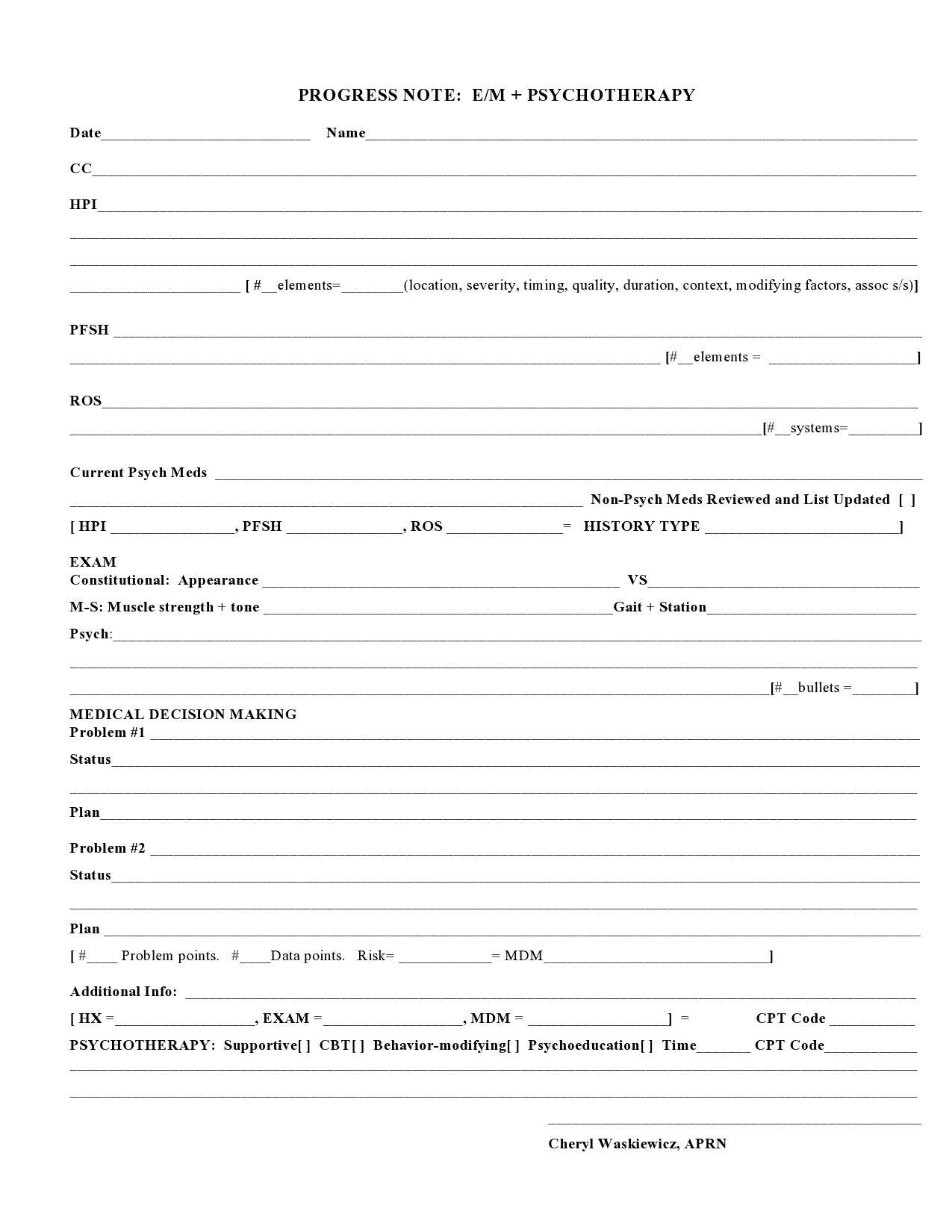
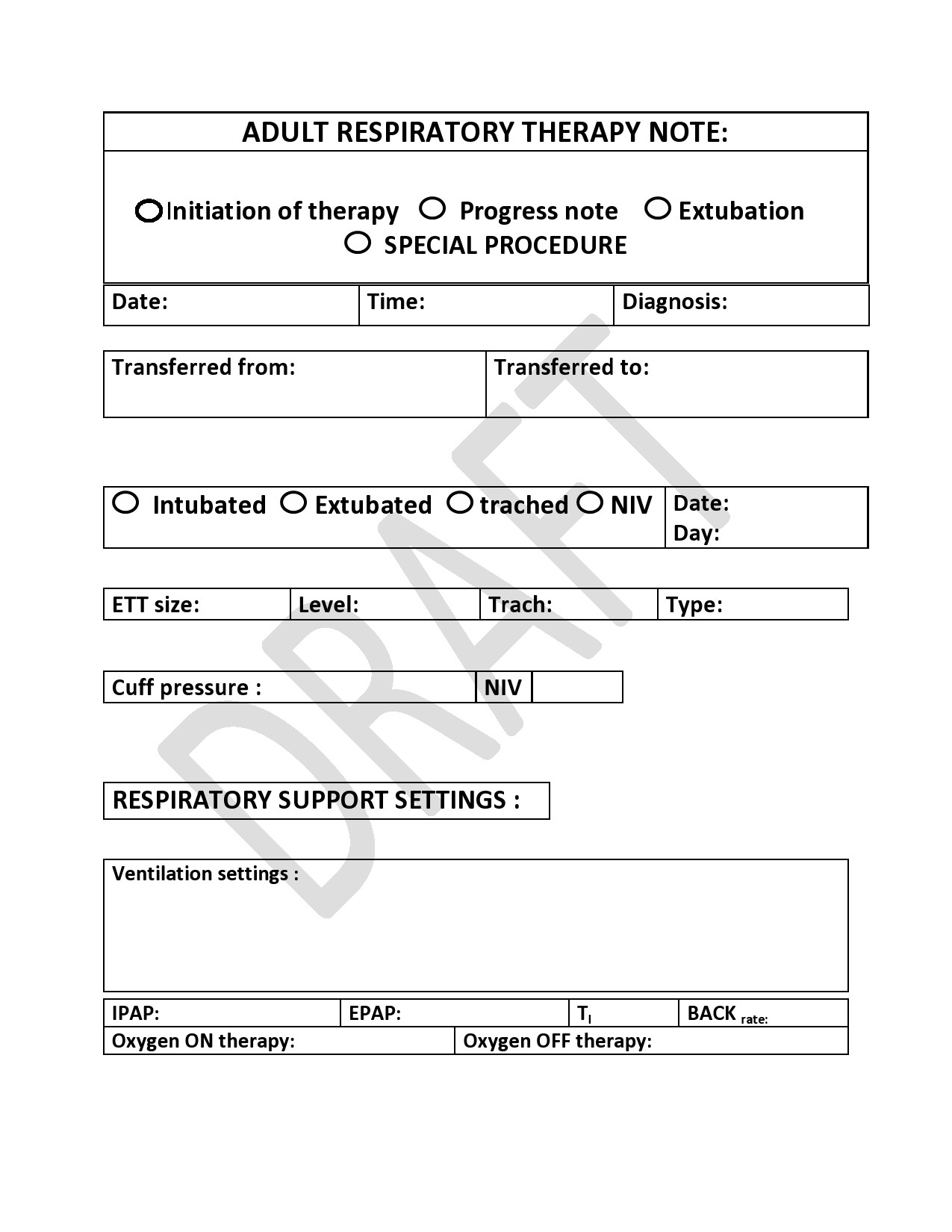
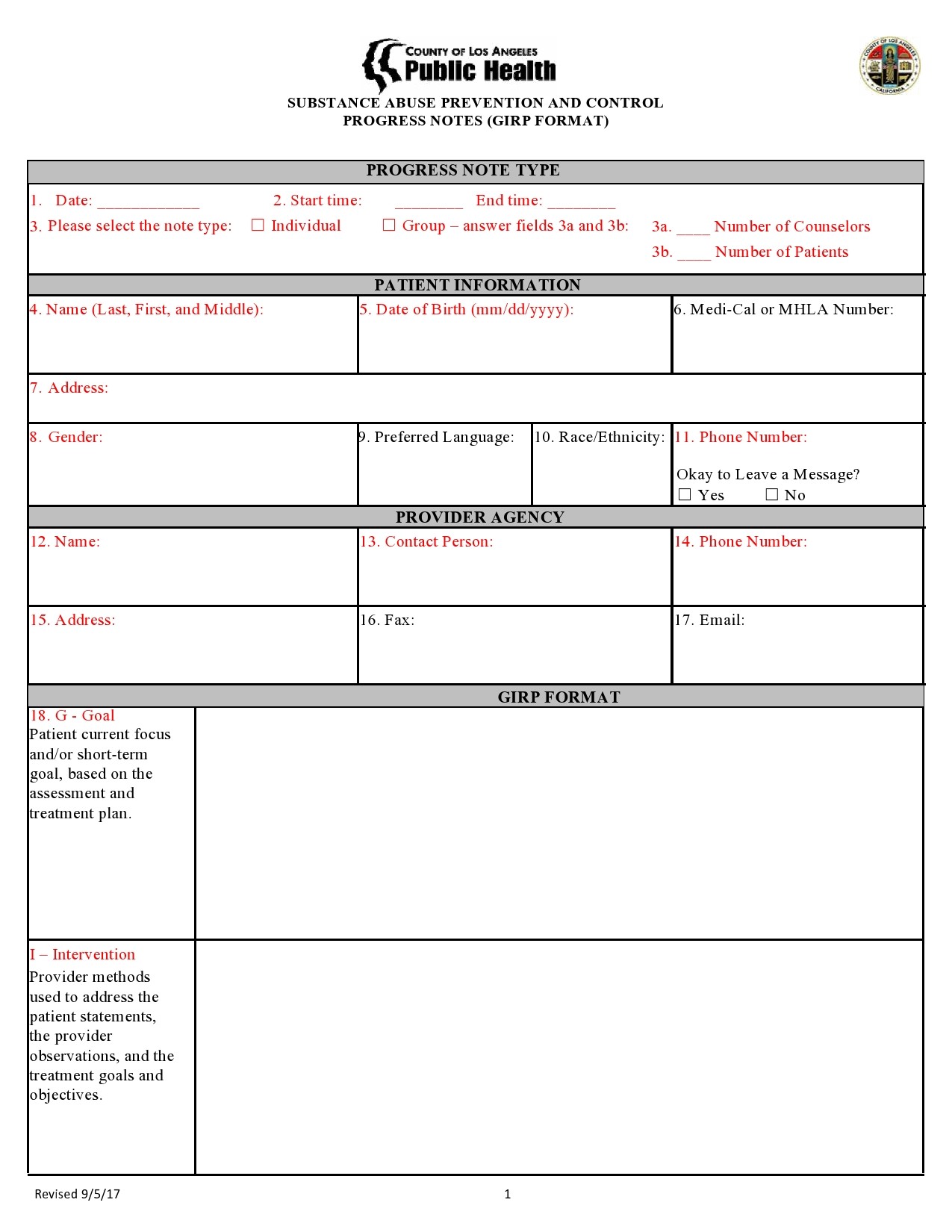
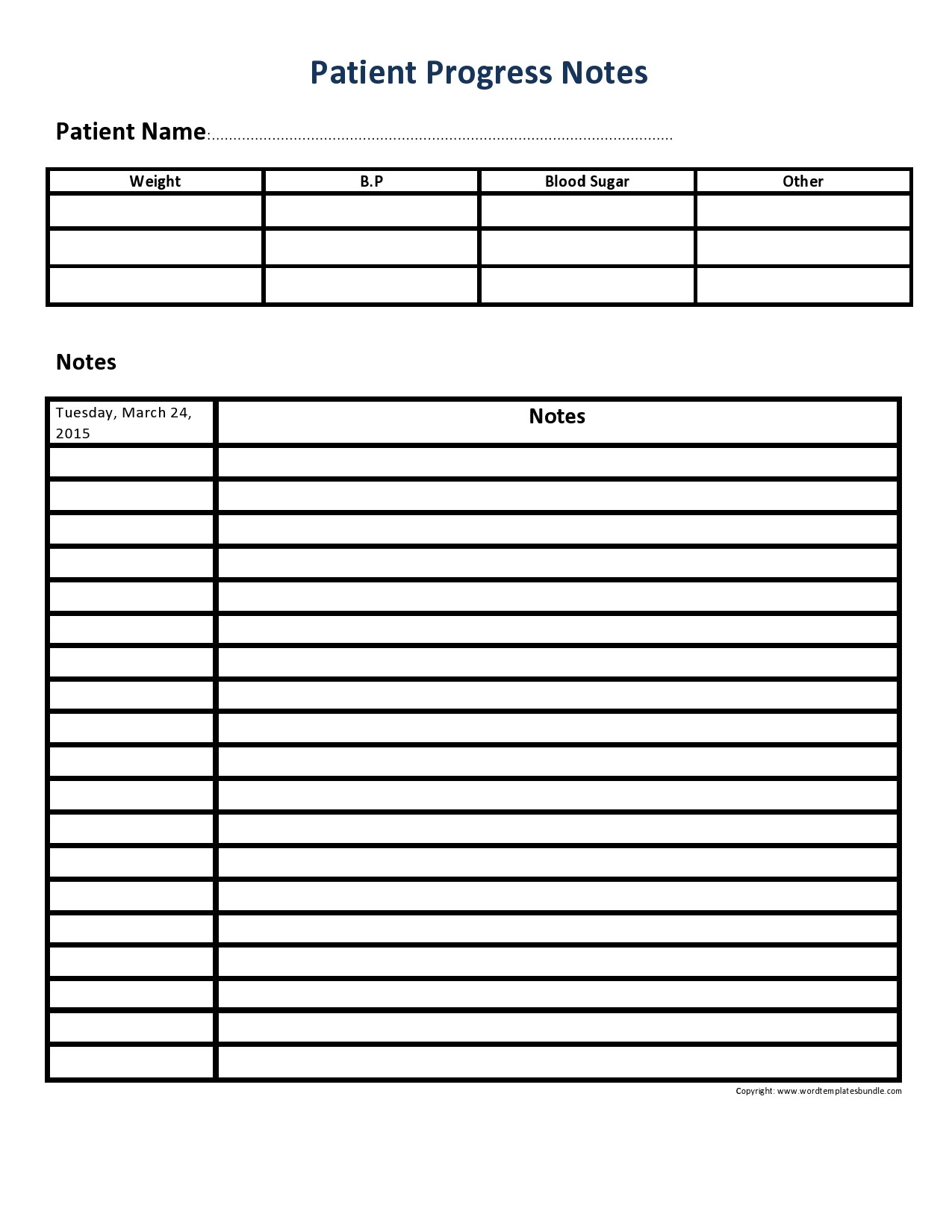
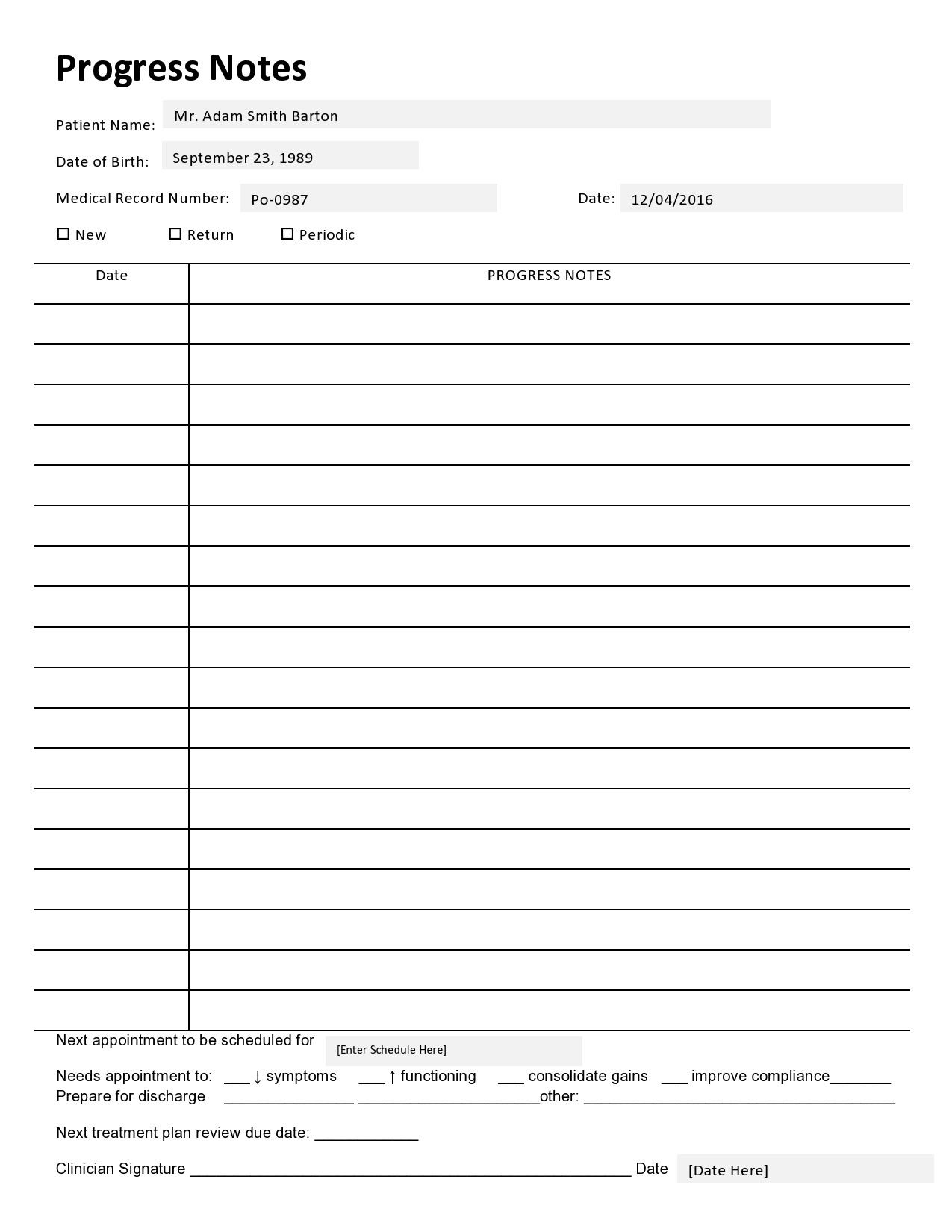
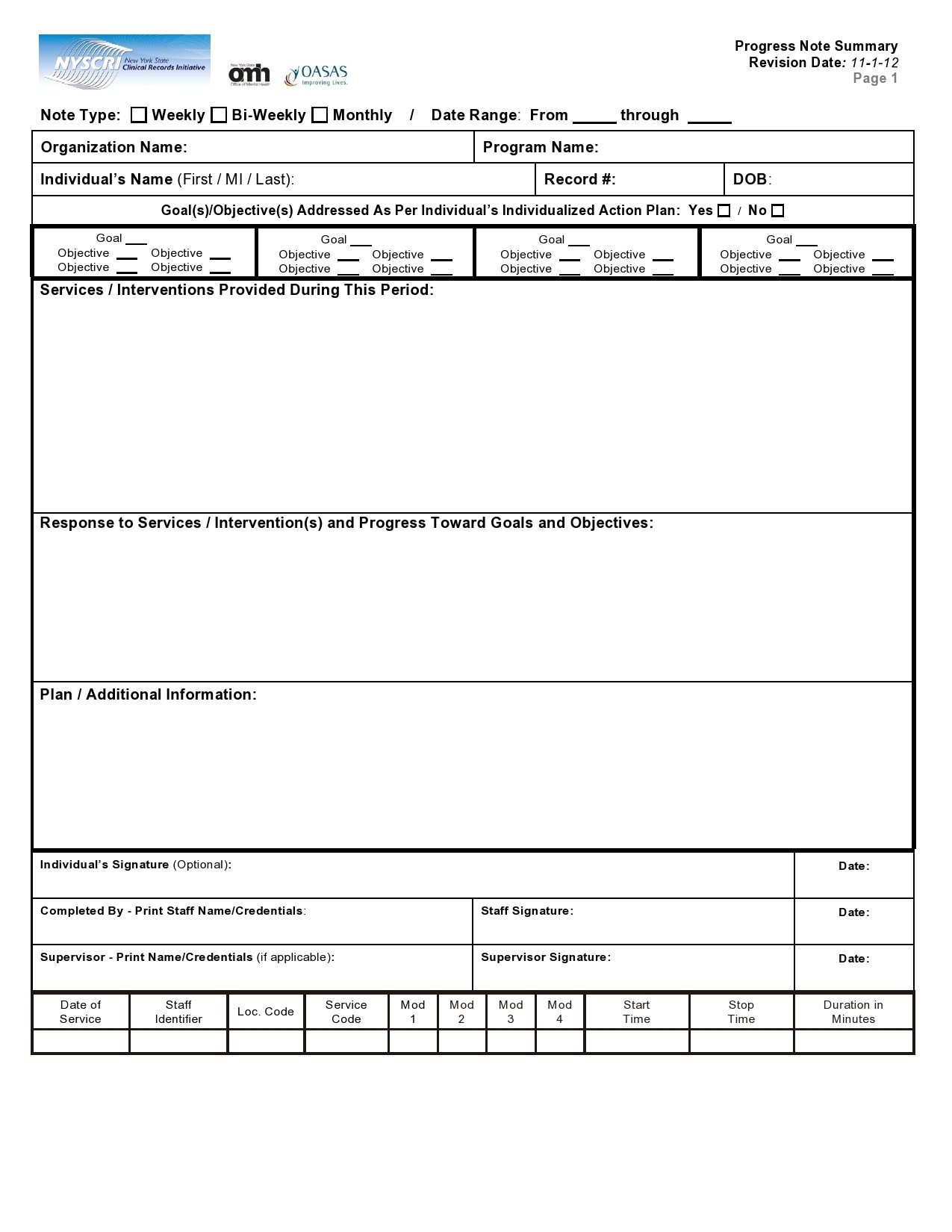
Therapy Notes Templates
Why do therapists take notes?
The most common reasons why therapists take notes are as follows:
They want to conceptualize your issue
The therapist wants to have a broader idea about your case. Before they help you, they must first understand the issue fully. To do that, they need to keep recording the important points they feel will help. This is what will bring out the bigger picture of the case before they begin to help you.
They want to record their thoughts
As you share your case, the therapist will want to investigate deeper. What you share is very important but there are specific things you might forget or leave out. The therapist will keep getting new ideas as you talk.
They will have new thoughts or feelings. If they don’t record them at that moment, they will forget. Recording helps them to remember every important detail or idea. These are the ideas they use to investigate further so that they will be valuable to you.
For future sessions
The therapist doesn’t want you to keep repeating your story from scratch every time you visit. It would be beneficial to take the case from where it stopped in the last session. If there are new issues to explore, they are explored based on where you left. Notes will help eliminate the inconveniences of having to repeat the background all the time.
It helps keep progress records
The purpose of therapy sessions is to help you heal emotionally. Your therapist should tell how you are progressing with each session. What will help them is the notes they’ve been taking from the time you visited first. They look at the history of your situation then and compare it with your current situation. From there, they can advise whether you need more sessions or not.
You might want to claim reimbursement
After your therapy sessions are complete, you might want to claim reimbursement. Your health insurer will want to prove that you visited a therapist. The therapy notes will be useful to help you successfully claim reimbursement from your insurance company.
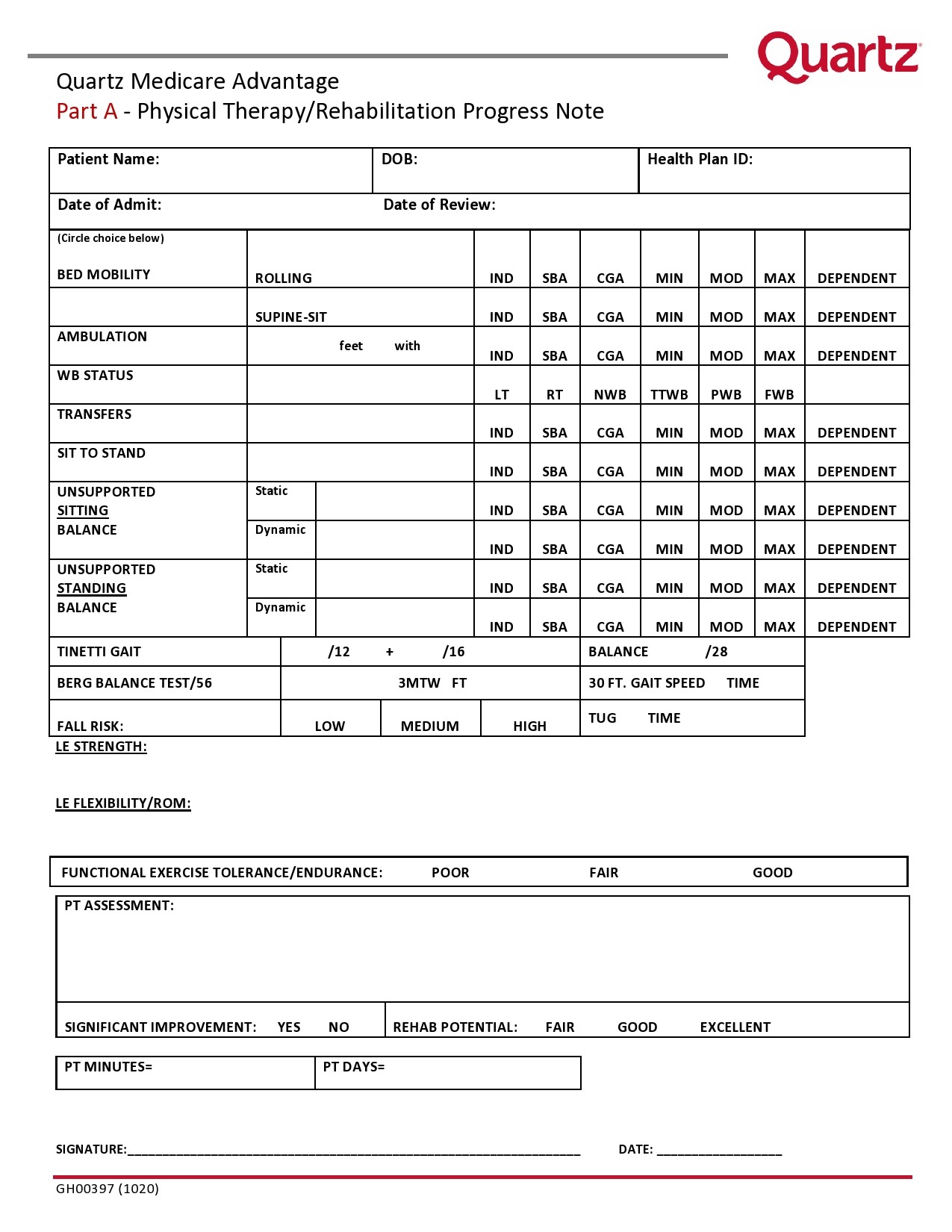
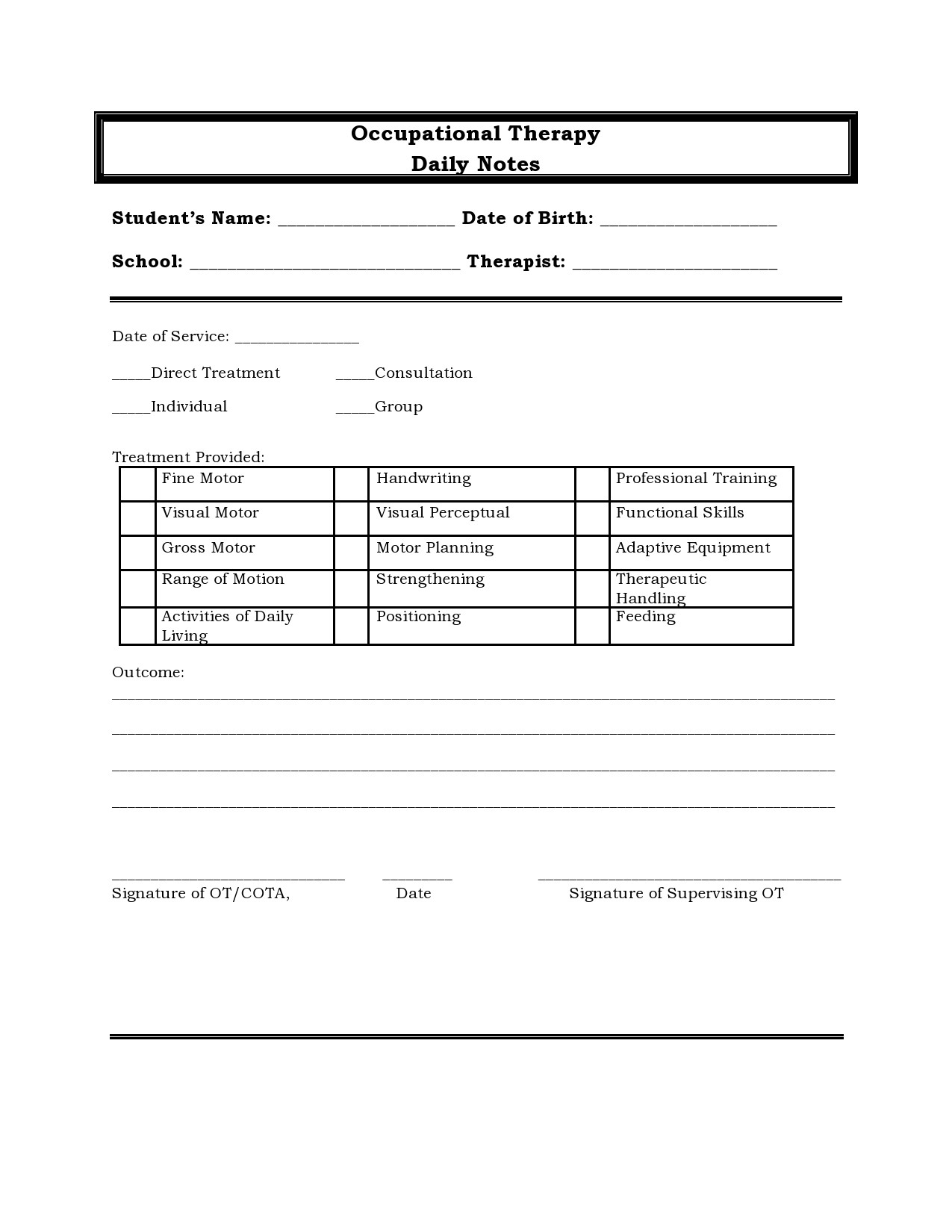
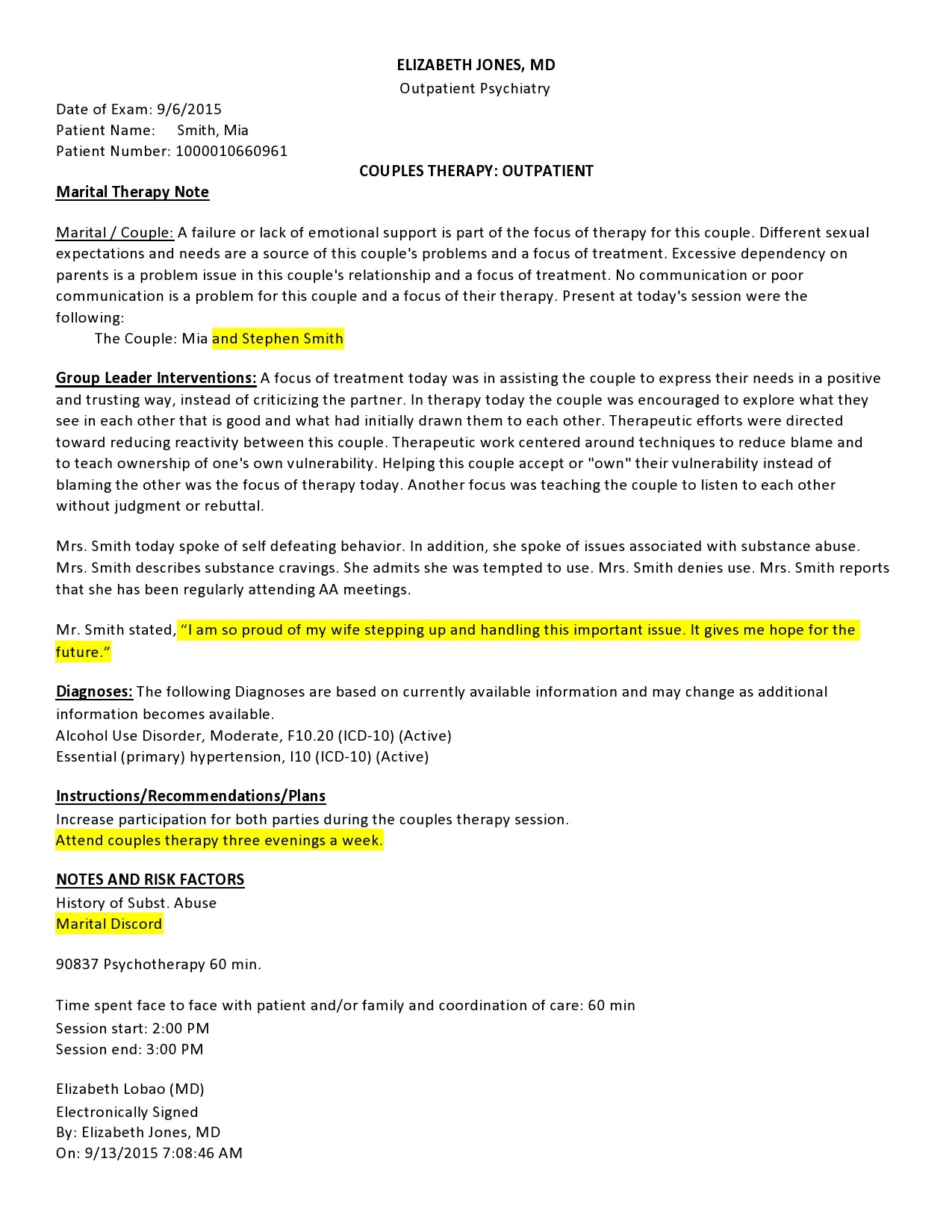
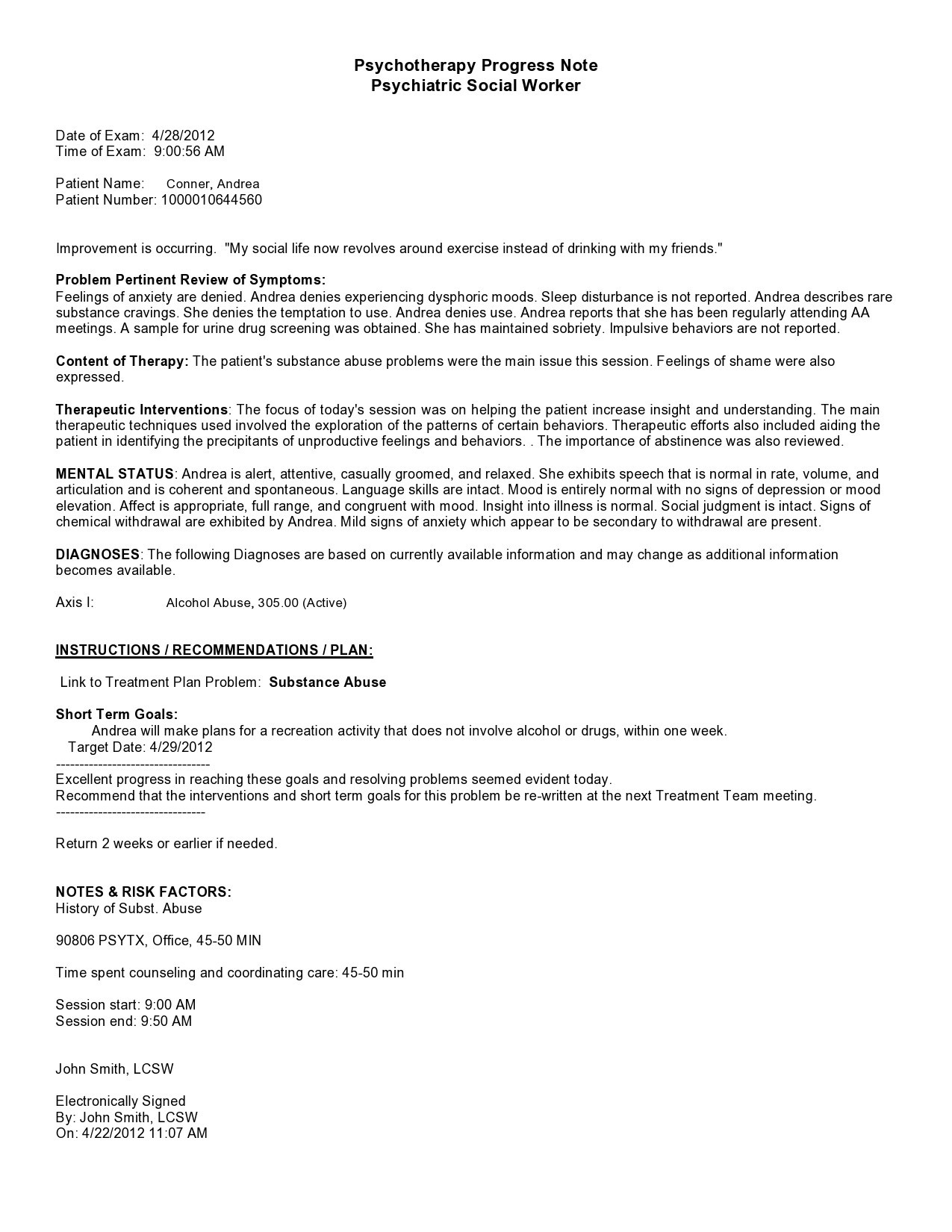
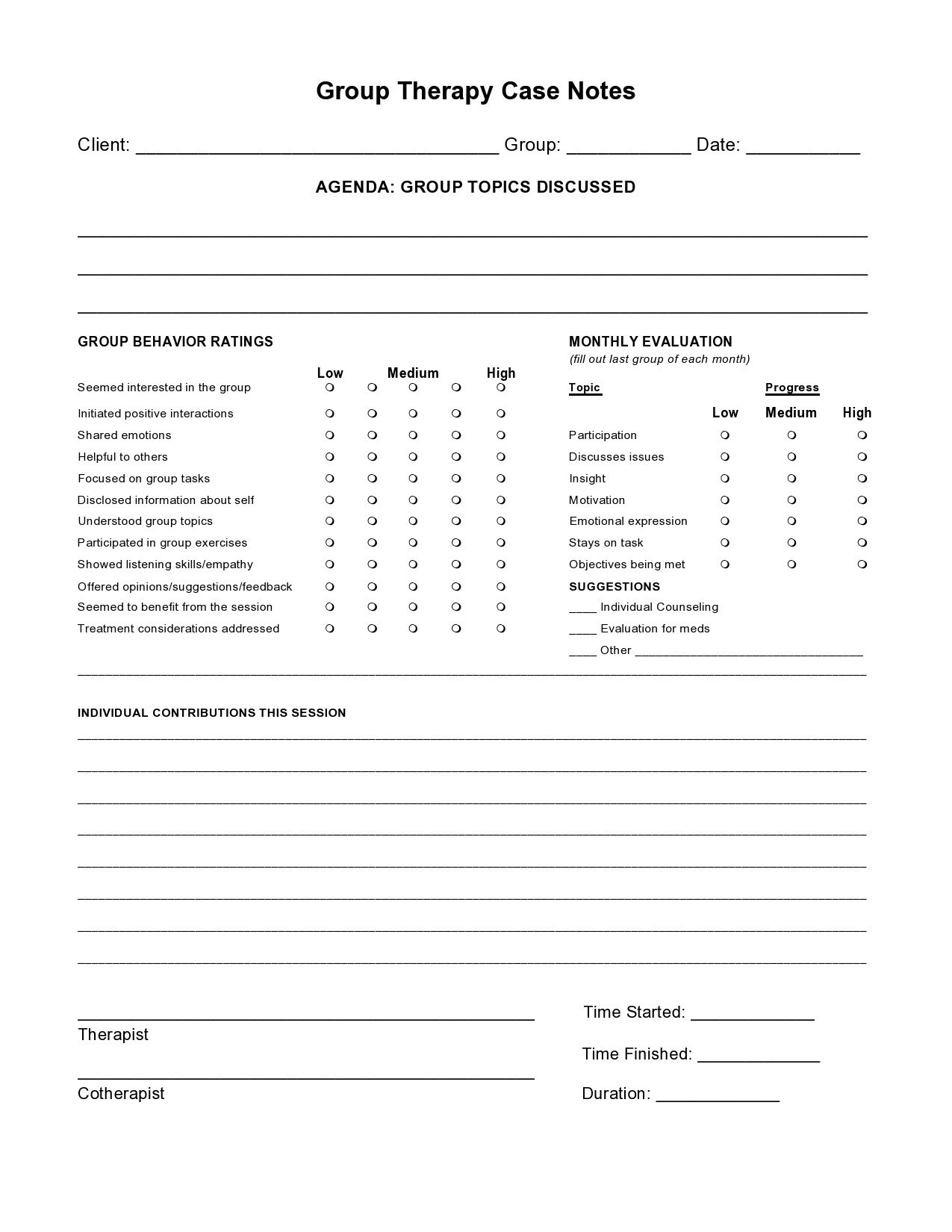
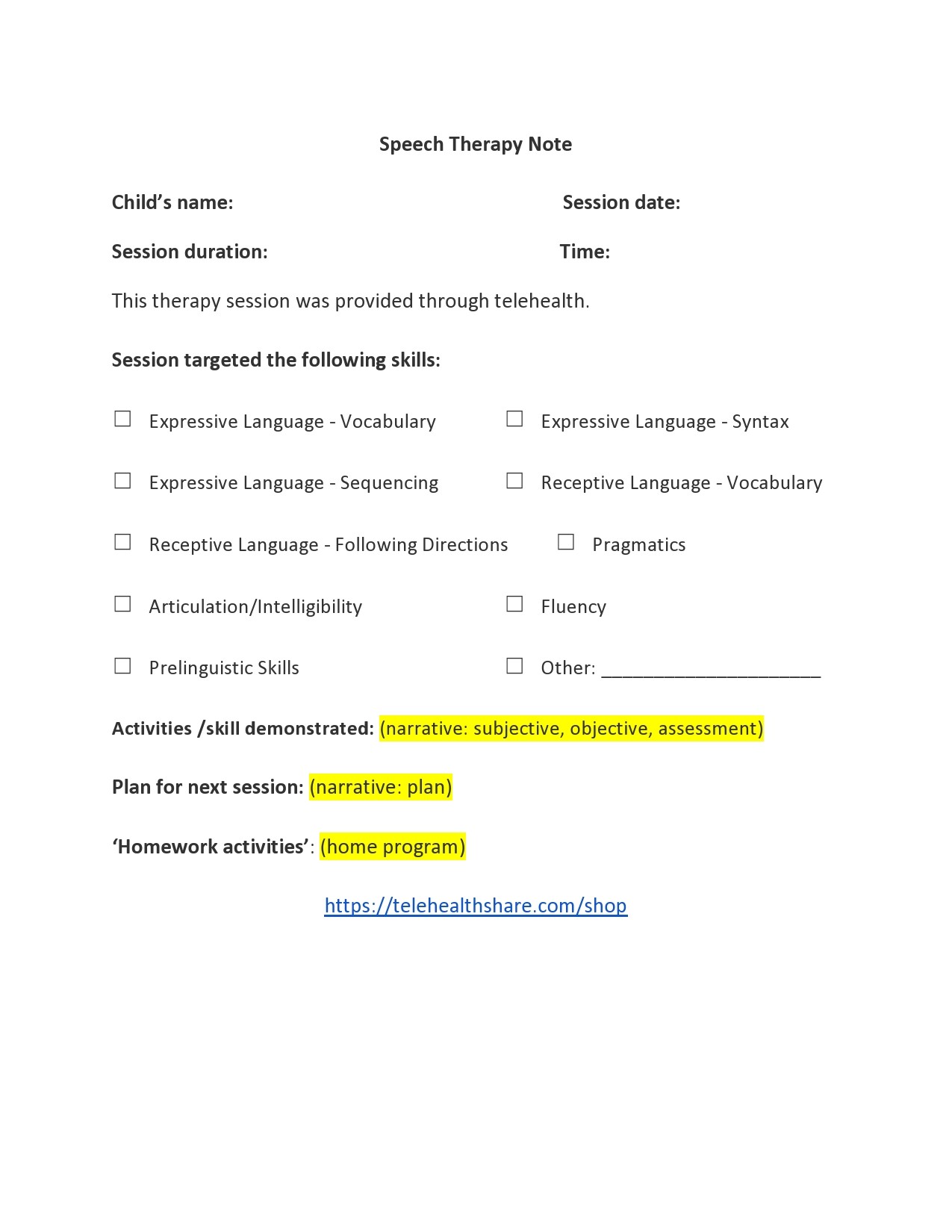
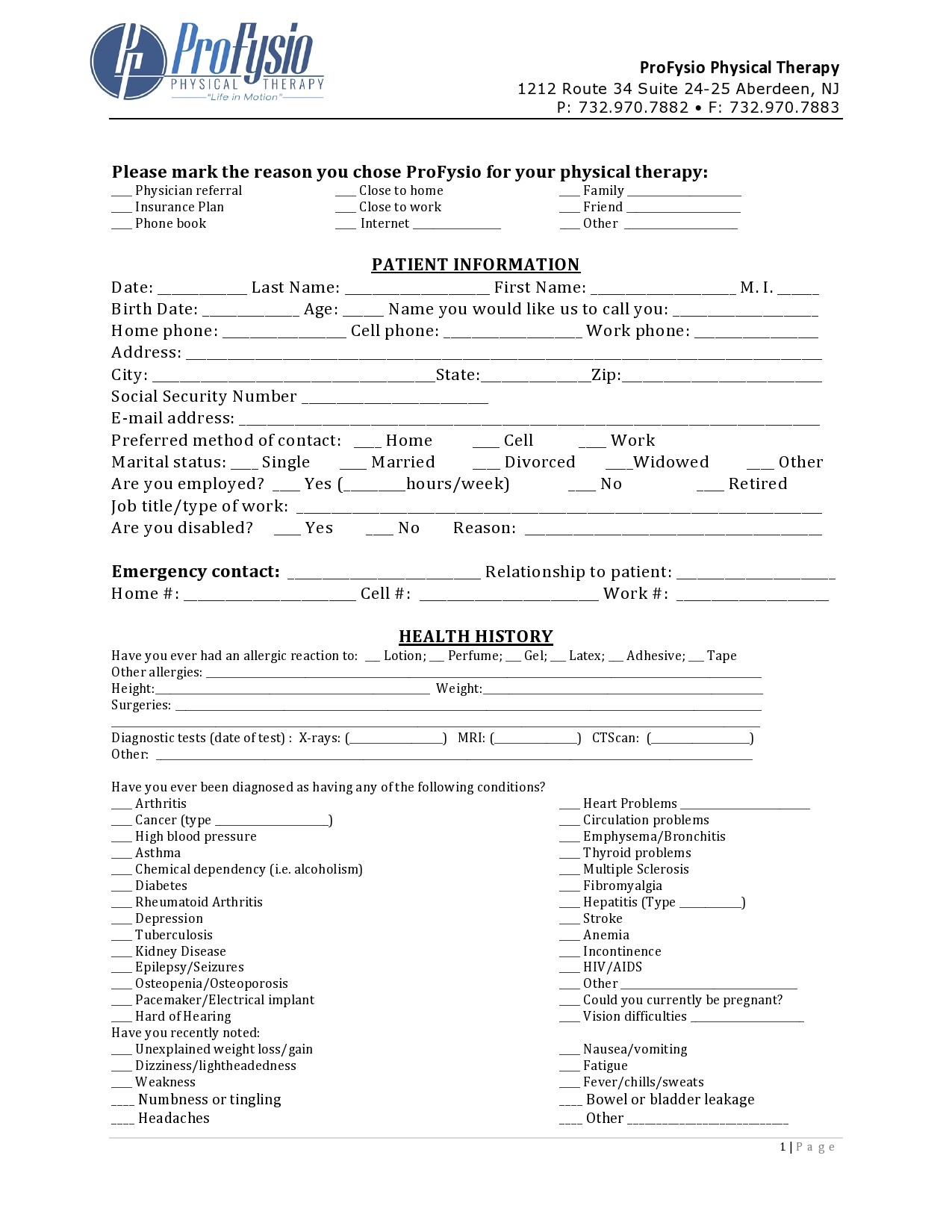
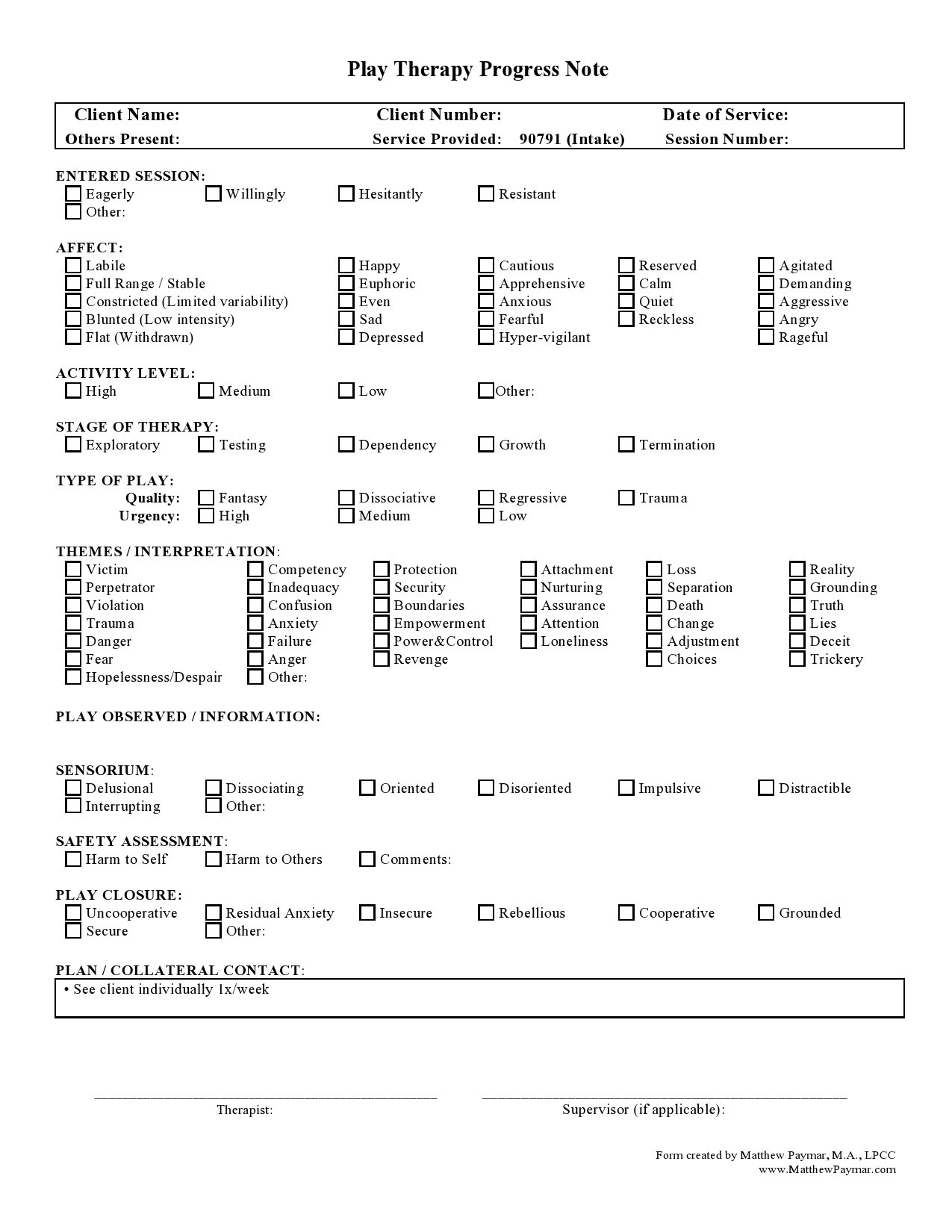
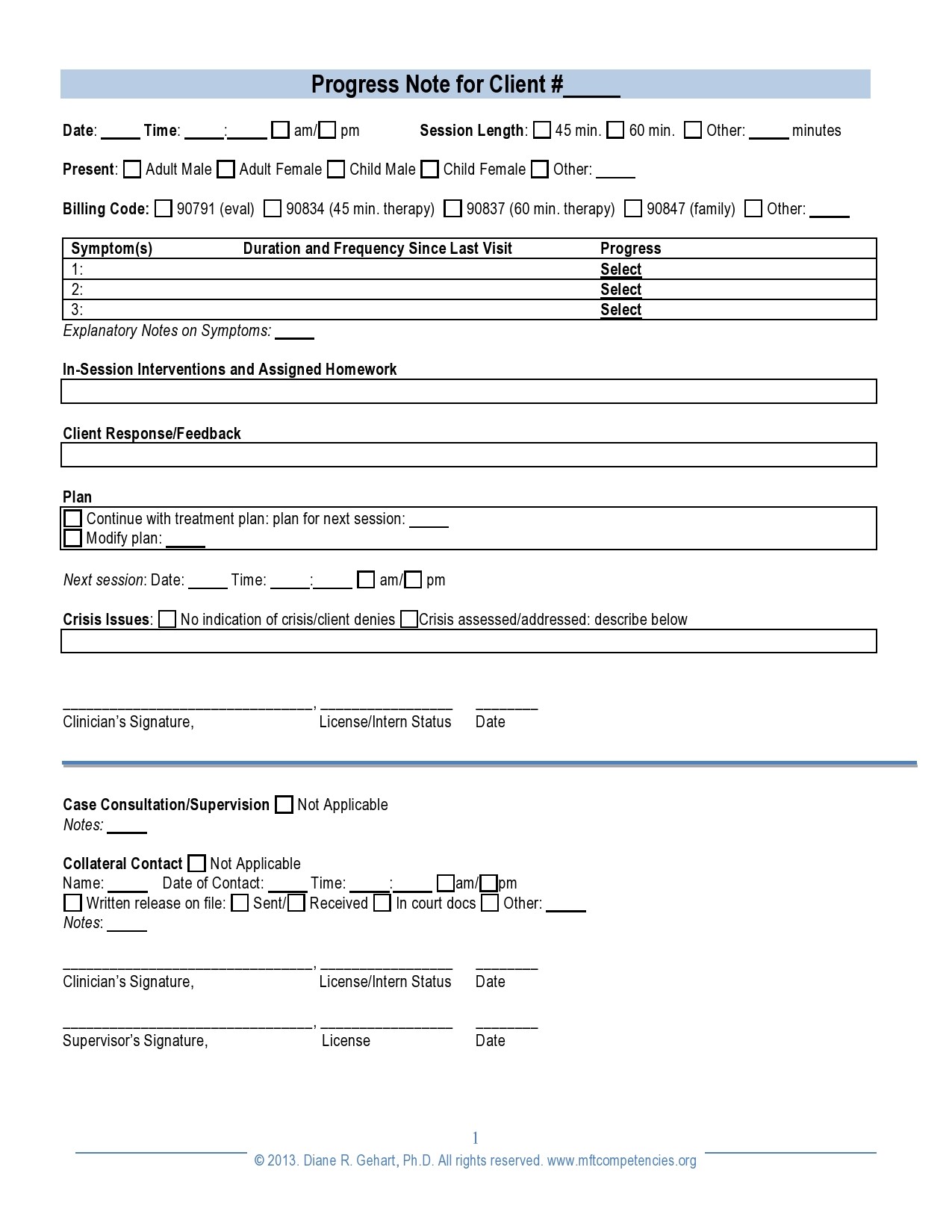
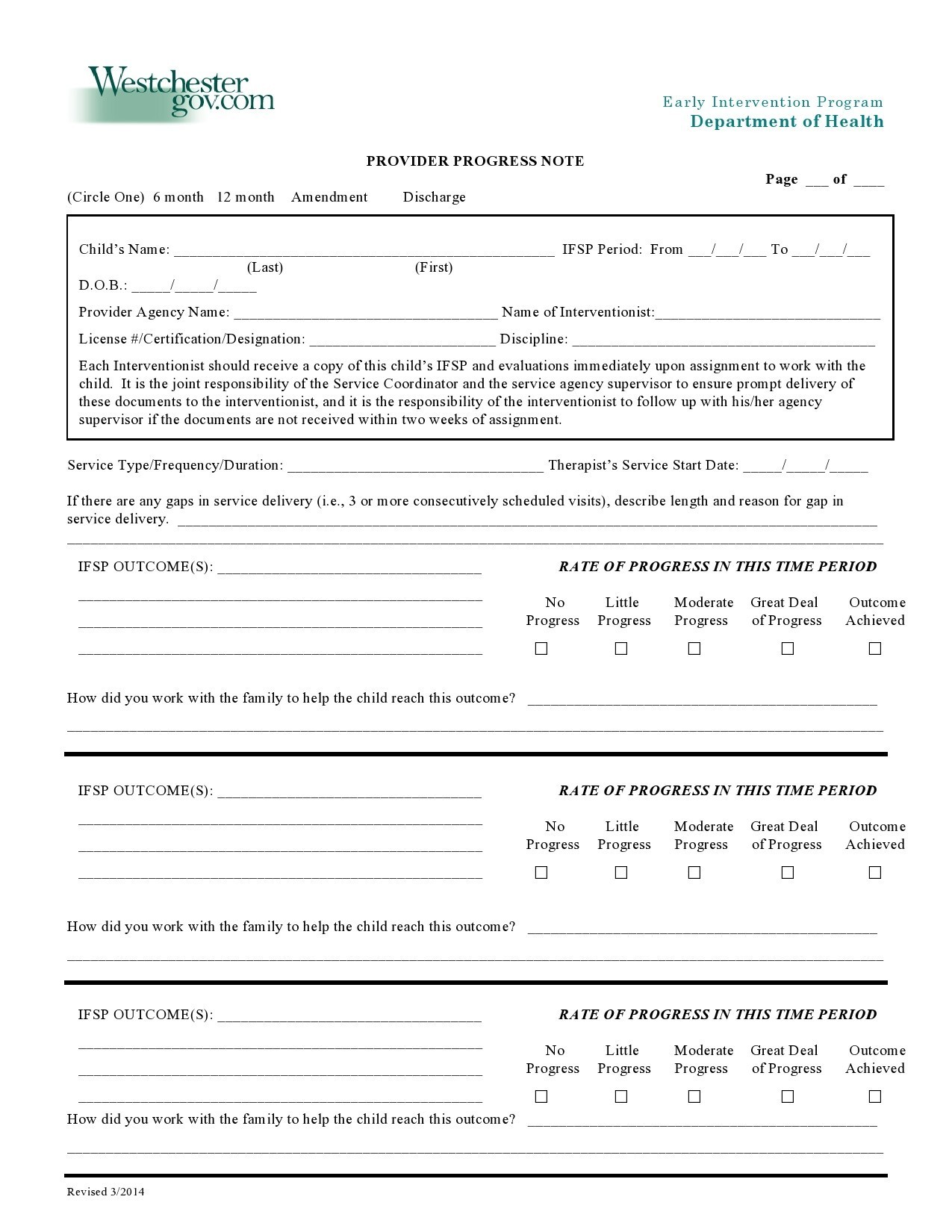
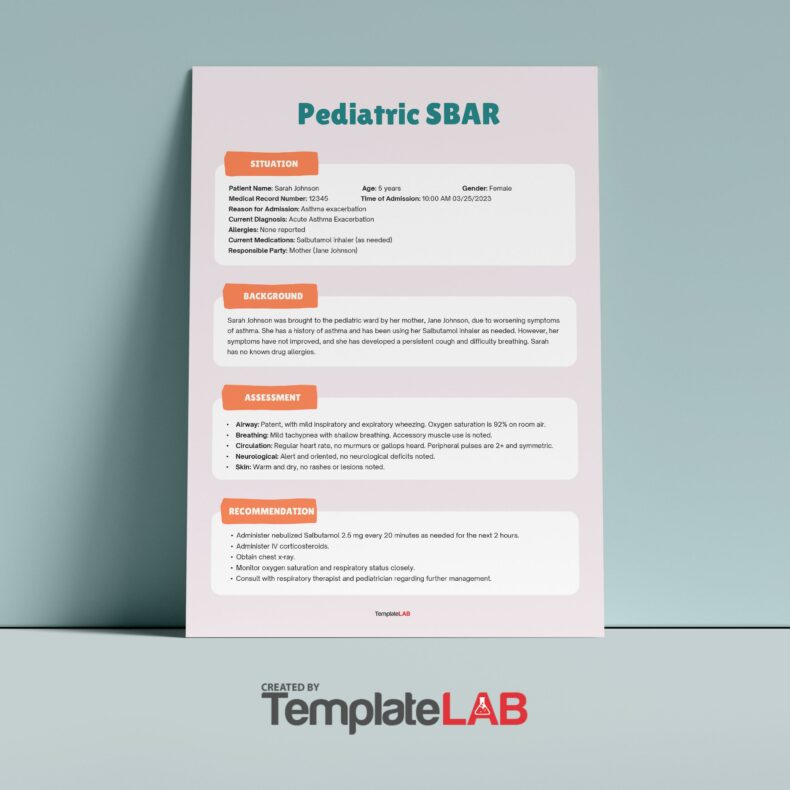
Therapy Notes Examples
Can the therapist’s notes be recorded in medical records?
Therapist notes are for your therapist. They contain detailed information about your history. Some of the information may be inappropriate to record in your medical file. That’s why therapists use a separate counseling notes template when recording your case.
They are solely used by the therapists who counsel you. Due to this, they are treated as confidential information that cannot be recorded in medical records. Your therapist will decide later what information to write in the medical record. This is information that can be shared or nonconfidential information.
Why do therapists require a counseling notes template?
The counseling notes template helps the therapist to record important notes fast. It provides several advantages.
It reduces distractions
As the therapist takes notes, it’s easy to get distracted. They want the information their client is sharing to keep flowing uninterrupted. The counseling notes template is designed in a way that the therapist will only need to insert the main ideas. It means the client will be less distracted.
It’s easier to use
The counseling notes template is already predesigned, which makes it easier to use. A therapist will not require to start drawing lines or notes structures to help them record information. The template is an easy-to-use document.
It safeguards client information
Mostly, the therapist will not need to print the counseling notes template. They can insert information on the soft copy and save it in their gadget. When recording information on papers or hard copy books, someone else can easily access the confidential information. When it’s recorded in softcopy, only the person with the password to the gadget will access the information.
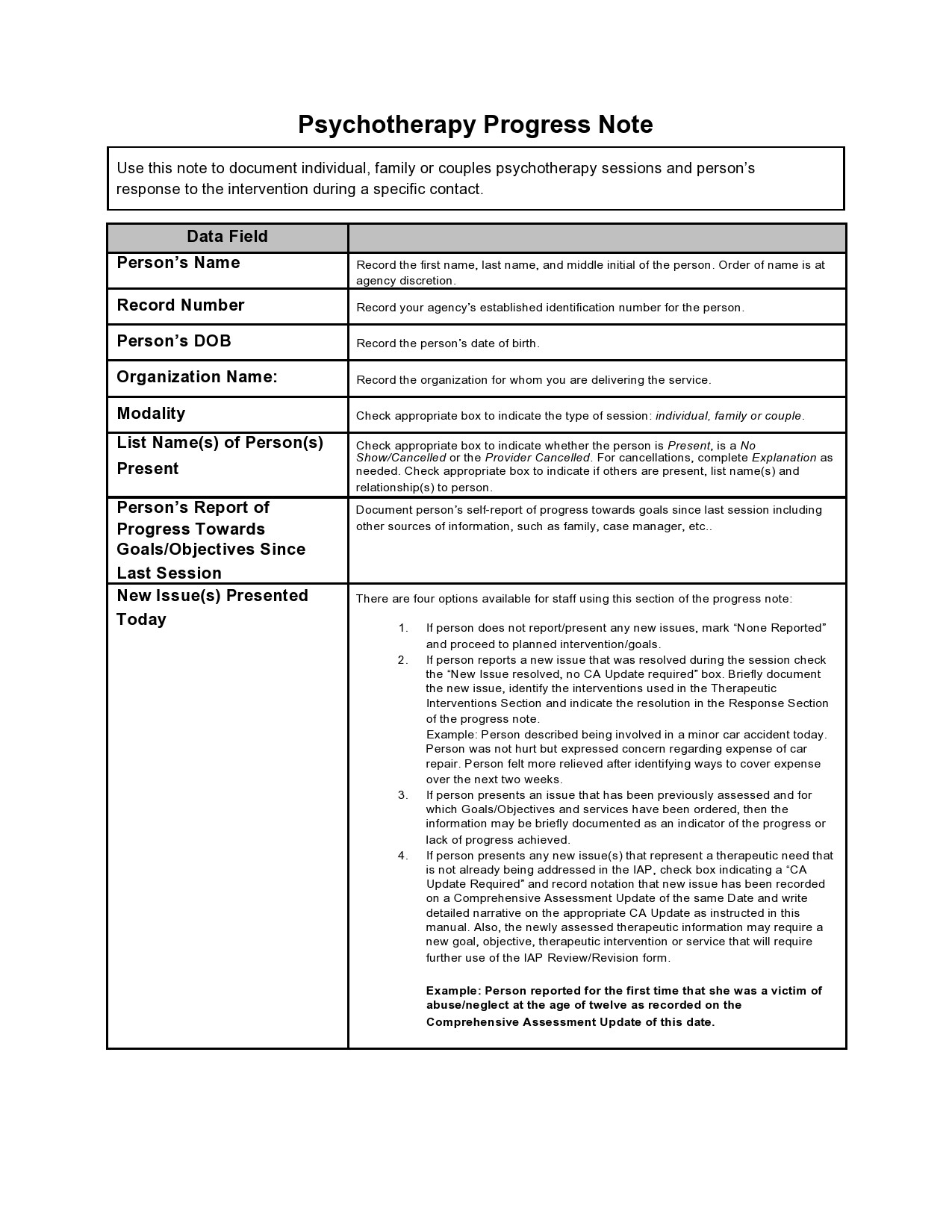
What needs to be in a therapy note?
A therapist must have documented information that will help them to accurately recall their sessions with their client. The document helps with treatment follow-up and effective cooperation with your client.
It is an important document to the insurer for purposes of reimbursement. You may want to refer to therapy notes examples to understand what should be included. For any therapy notes document to be effective, it must include the following details.
Client demographics
The details of your client demographics are necessary. You might be attending to several clients each day. You don’t want to confuse therapy for one client with another. Make sure you capture the following information in this section.
Client name: Do not use an alias name or codes to note a client. Some of the information in the progressive notes will be captured in the client files. Again, you will create a better relationship if you address your client by their name. Record their full name in the counseling notes template. Here are the other important things:
- Client age
- Gender
- Ethnicity
- Employment
- Marital status
- Physical address
When you have recorded a client’s current living situation and occupation, it will help get some ideas about their current situation. The information could be valuable when creating a treatment program.
Client diagnosis
Client diagnosis will help you develop a treatment plan. For billing, make sure you have included the ICD code (International Classification of Diseases) in the diagnosis. Health insurers will always demand proof that the treatment occurred. It will help you with billing and reimbursement claims processes.
Your client case/problem
You must record your client’s case as they present it before you. It helps you get more accurate information when you record it in your own words. As you review the notes later, you may notice important information that will help you develop a better mental health treatment plan.
Any safety precautions
Some of the clients who visit you might be planning suicide. Others might be planning to harm the people they think are contributors to their problems. Still, some might have deeper mental issues that could be a danger to you. In the progressive notes, record any safety issues that you might feel needs to be addressed immediately. You may record them in three categories.
- Your client’s safety concerns
- Their immediate family safety concern
- Your safety concerns
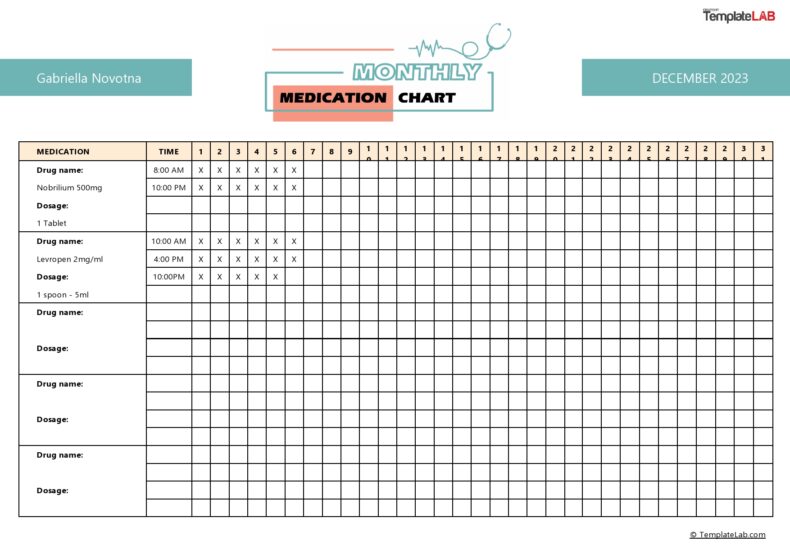
Medications prescribed
The client might be taking medications prescribed by a health specialist. Record the details of the medication.
- Type of medicine
- Prescribed dosage
- When they started to use
- When they will stop
- What is being treated
- Any experienced side effects
The type of medication your client is taking could have certain side effects. They might have a certain level of effect on their mental health.
Symptom’s history
It is necessary to record the history of the client’s symptoms. Record how the symptoms have impacted their health, relationships, and work. Find out what they have been involved in over the years. Record any successes they have had and what went wrong. Request the client for any treatment documents they might have.
Your client’s current mental status
Record the mental status of the client. You may observe their mood, behavior, or appearance. If you notice anything unusual, record it. You might require to use a mental exam cheat to help you through this part.
Interventions applied
Record the interventions you apply to assist the client. Record the main issues you discussed in the session. If it’s not the first session, record if the client followed the instructions you gave. Find out their willingness to follow or refuse the instructions.
Plans for treatment and goals
Record the plans you create for treatment. You may decide to prescribe
- Behavior therapy
- Humanistic therapy
- Integrative therapy
- Cognitive therapy
- Psychoanalysis therapy
In the record, include how the intervention you recommend will help your client progress well. Record also the actions you will require the cline to do. There might be assignments to do at home and others to do at your facility.
Progress notes
For each session, record any progress that you can directly observe. It will help you decide if their symptoms are deteriorating or improving. If they fail to show any improvements, record why they are not improving. It could be they are not following your instructions. It could also be they might require a different approach or change of therapy. You may want to refer to progress notes examples for ideas.
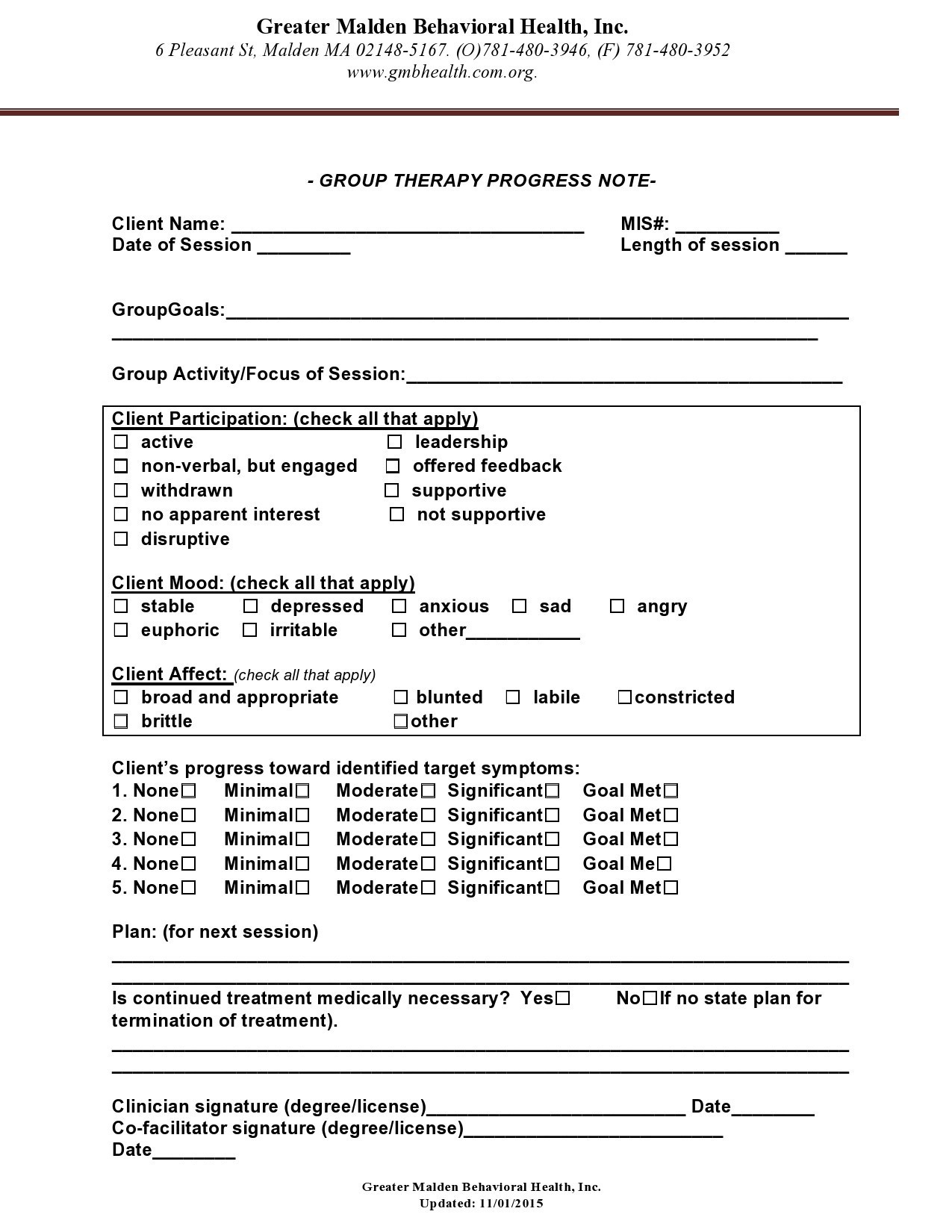
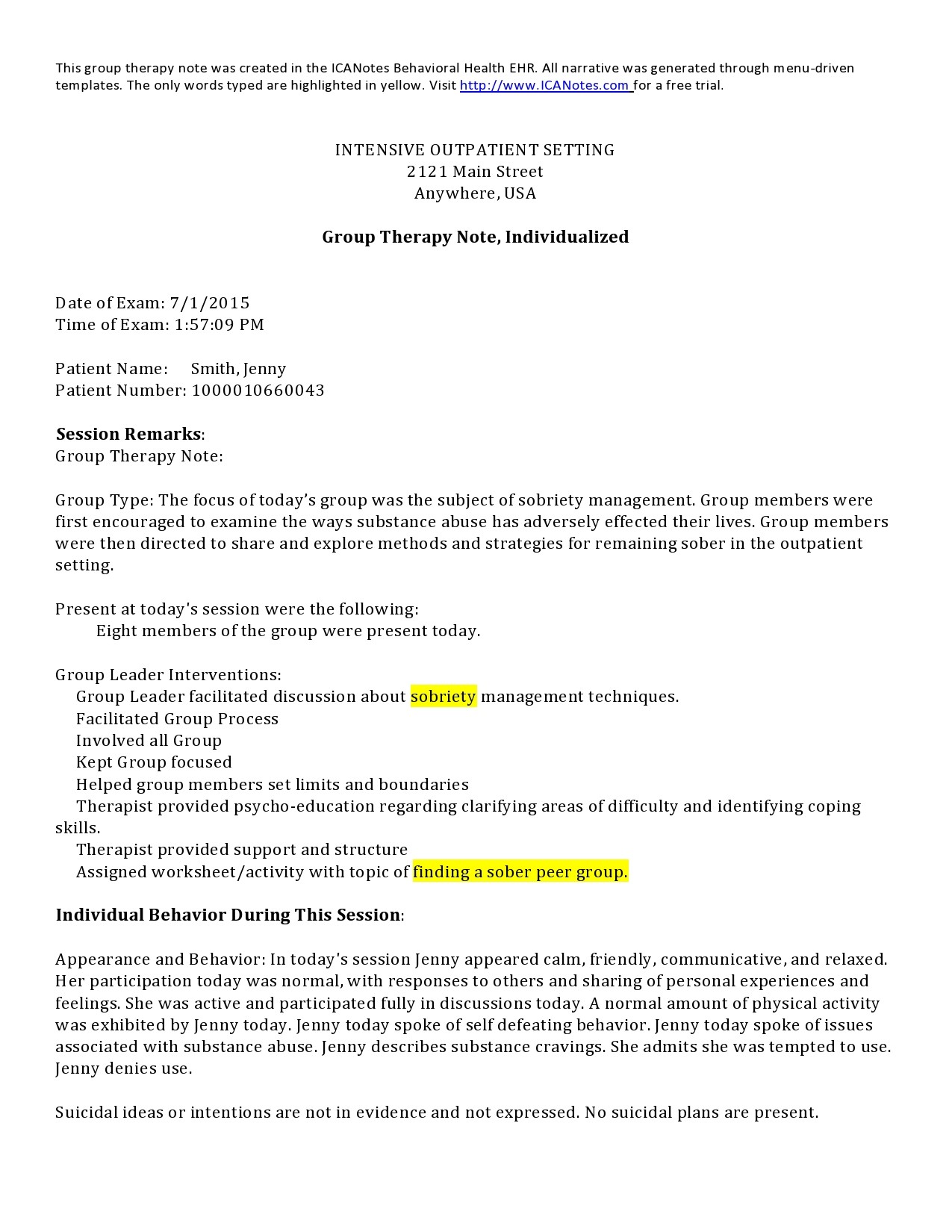
Progress Notes Examples
How do you write a therapy note?
There might not be a specific formula for writing a therapy note. You may develop your formula or get inspiration from progress notes examples. Choose a therapy note template that will meet your needs. This is how you will write a therapy note.
Record the names
If you are dealing with one client, record their name. If it is a group session, record the names of every participant. You may include their contact details such as telephone and email for future follow-ups.
Session type
You will be handling different types of therapy sessions. Record if it’s a –
- Group session
- Family session
- Students’ session
- Individual
- Couples etc.
Date
Record the date each time a client visits. It will help you build a timeline that will help monitor your client’s progress.
Start/finish time
It is professional to record the time when a session starts and the time it completes. If you are charging for the sessions per hour, it will help prepare the bill.
Current progress
You can record progress in two ways:
- Progress since the last visit
- Overall process since therapy started
When you understand your patient’s current status, you will have an idea of where to begin the current session. It also helps you to know if you need to change your approach or advice for a doctor’s help.
Observations/actions
Record any mental issues you notice the client is displaying. They might be looking tired, stressed, unstable, restless, ungroomed, etc. Record if they acted on the assignment/s you have given them in the last session.
Preparation of the session
You can fill out this section in advance. It will help you to be ready by the time your client arrives. You may highlight any significant observations you made in the last session that require follow-up.
Session description
You may want to introduce a new session but you must highlight it before the client. Give reasons, if necessary, on what you expect and why the session is important.
Any dangers, assignments, and next appointment
Record anything you notice could signal danger to the client. Even when they don’t expressly say it, you may notice they have suicidal thoughts. If there are more actions you want the client to do, record the assignments you have given them. Take note of further insights you get from the client. Record the date and time for the next appointment.
Signature
Sign the progressive notes template as confirmation that the client visited you for a therapy session.
The common types of session notes
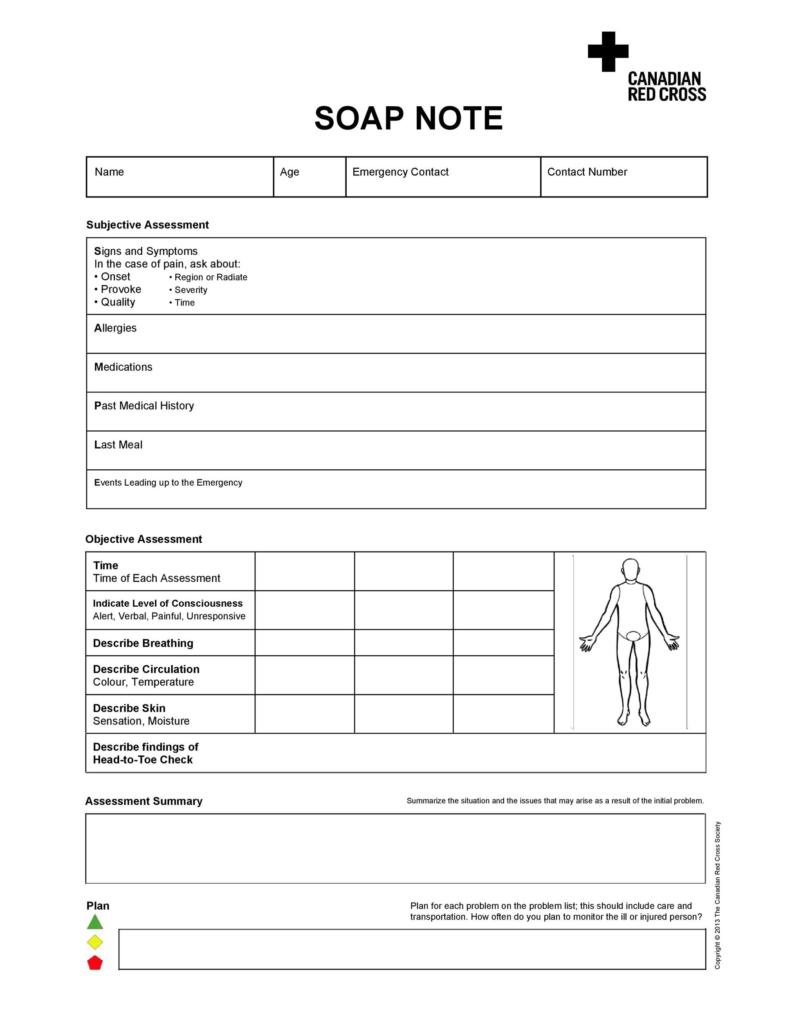
When you read therapy notes examples, you will notice three main types of therapy notes templates.
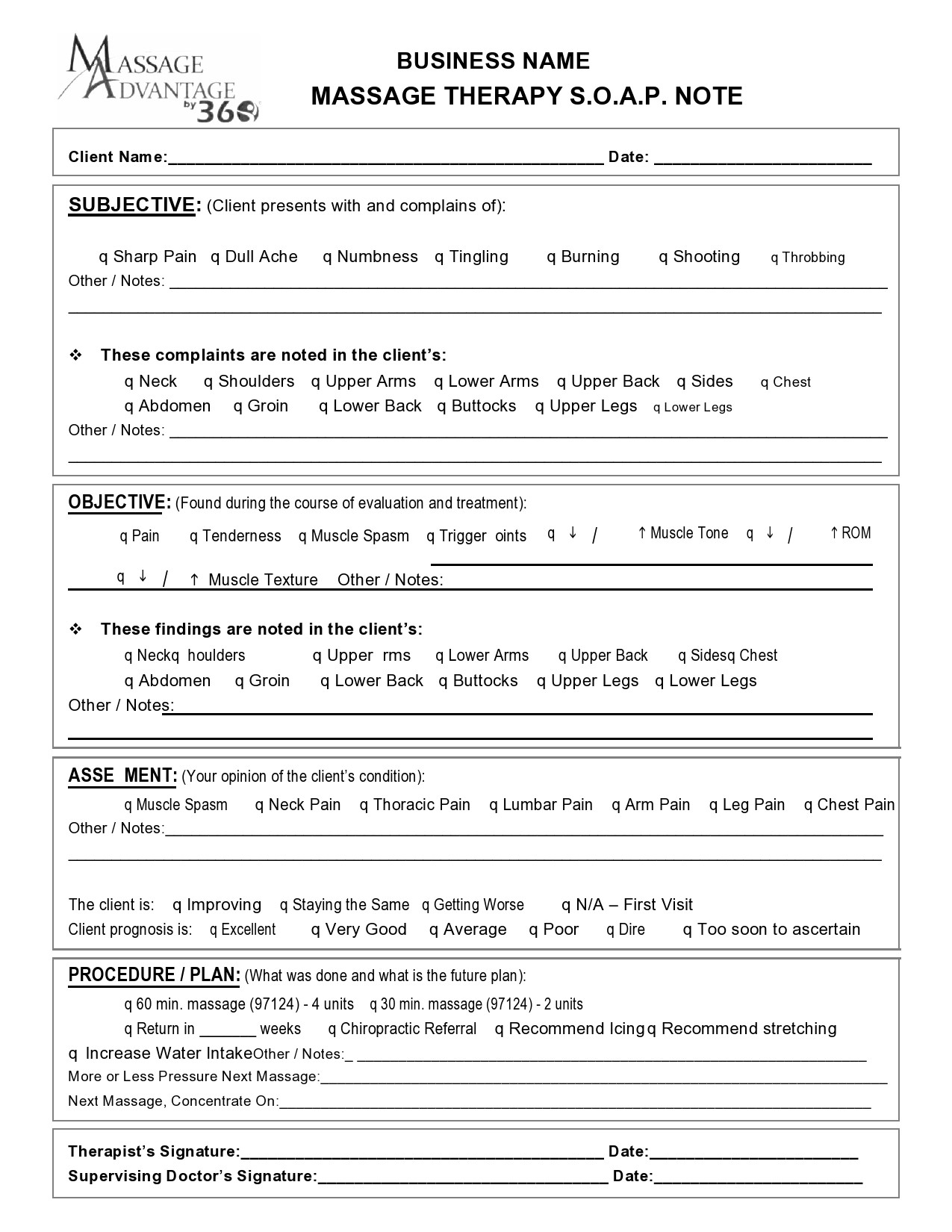
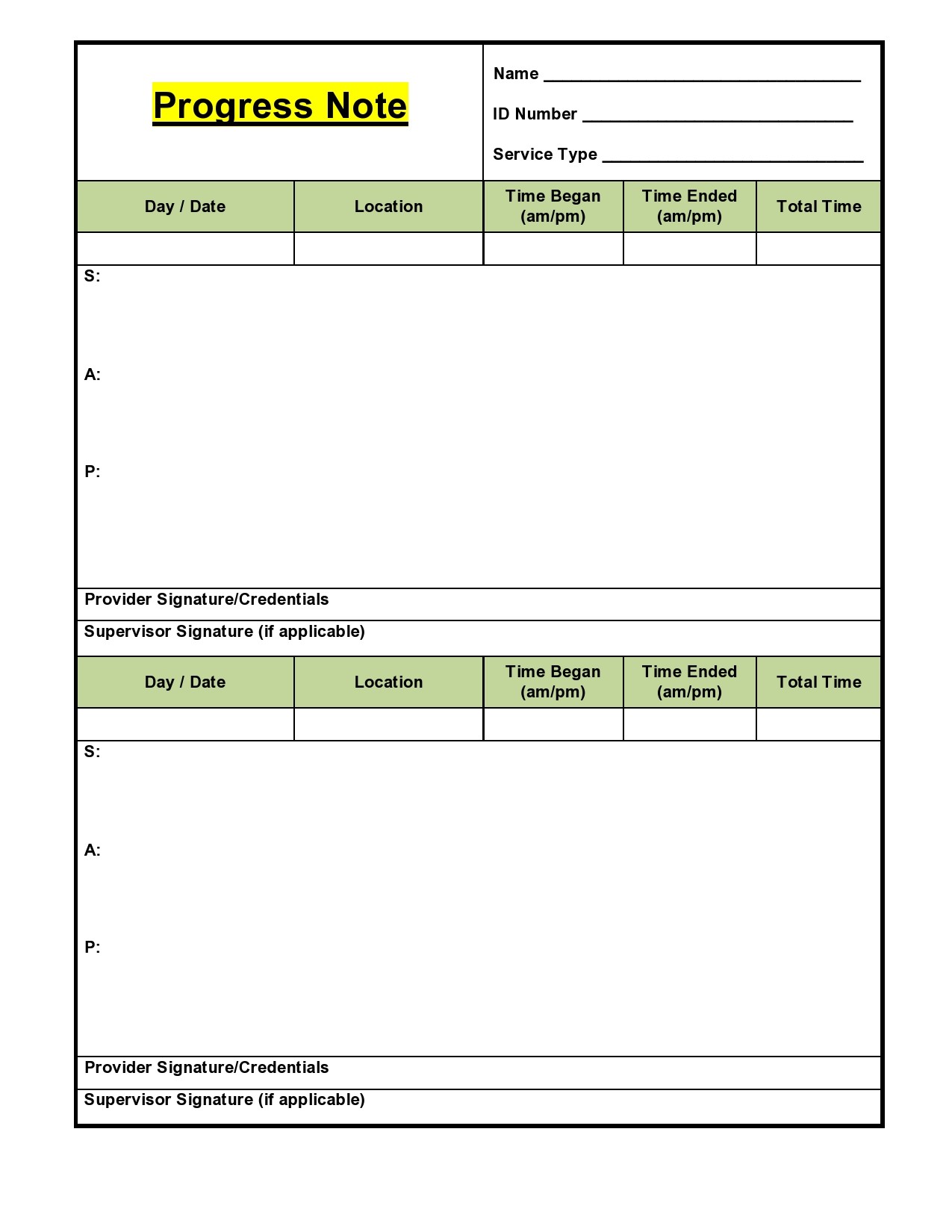
SOAP notes
SOAP progress notes examples contain four main types of details.
- Subjective
- Objective
- Assessment
- Plan
BIRP Notes
BIRP progress notes examples record the following:
- Behavior
- Intervention
- Response
- Plan
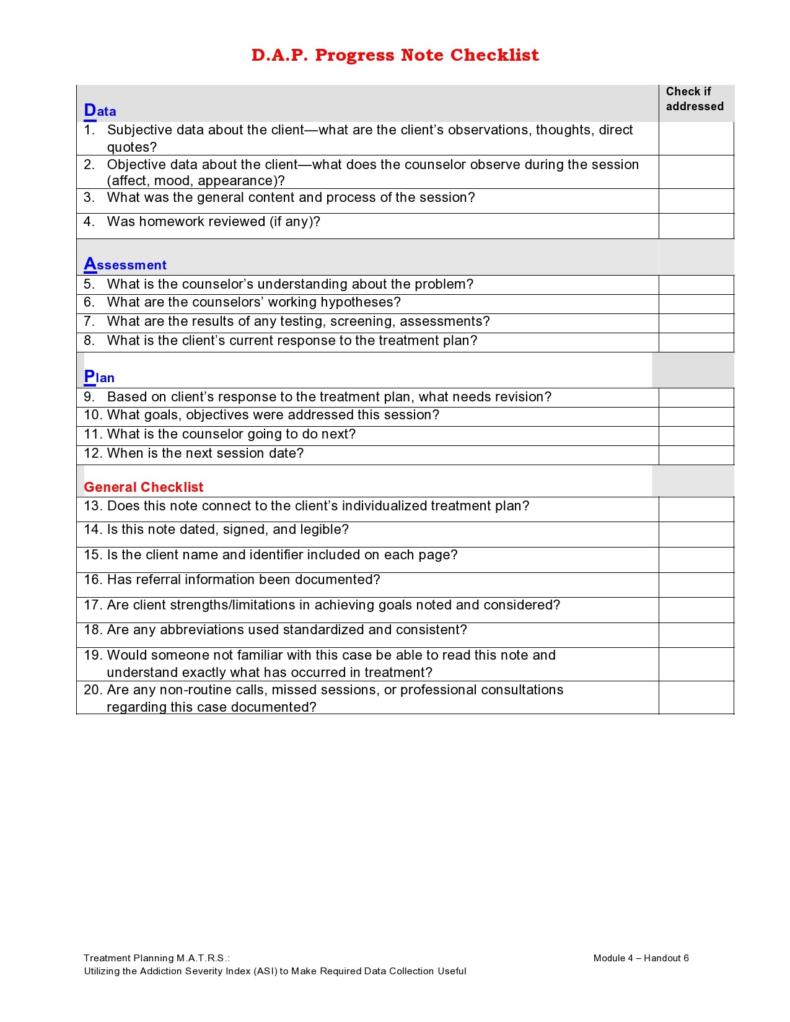
DAP Notes
DAP notes record the following:
- Data
- Assessment
- Plan
Counseling Notes
Other categories of therapy session notes
Session note: They are used during a therapy session
Event note: They are used to record significant life events of a patient, such as medication history, behavior changes, and progress.
Contact note: They are used to record communications with a client, such as follow-ups, schedules, and logistics.
Supervision notes: It records any interactions with anyone responsible for the supervision of the patient. It could be a family member or another authorized caretaker.
Treatment note: It records any treatments given to the client.