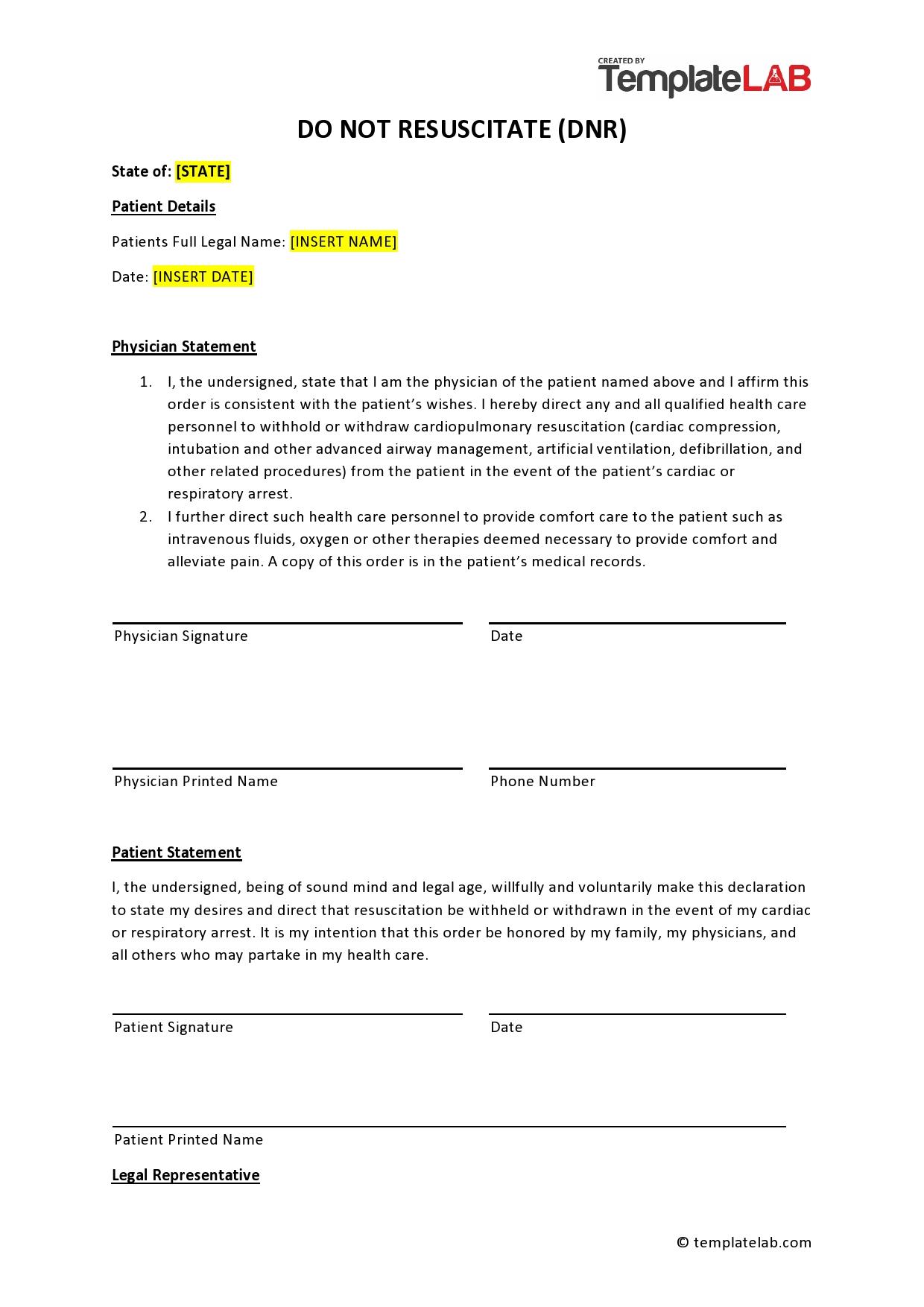
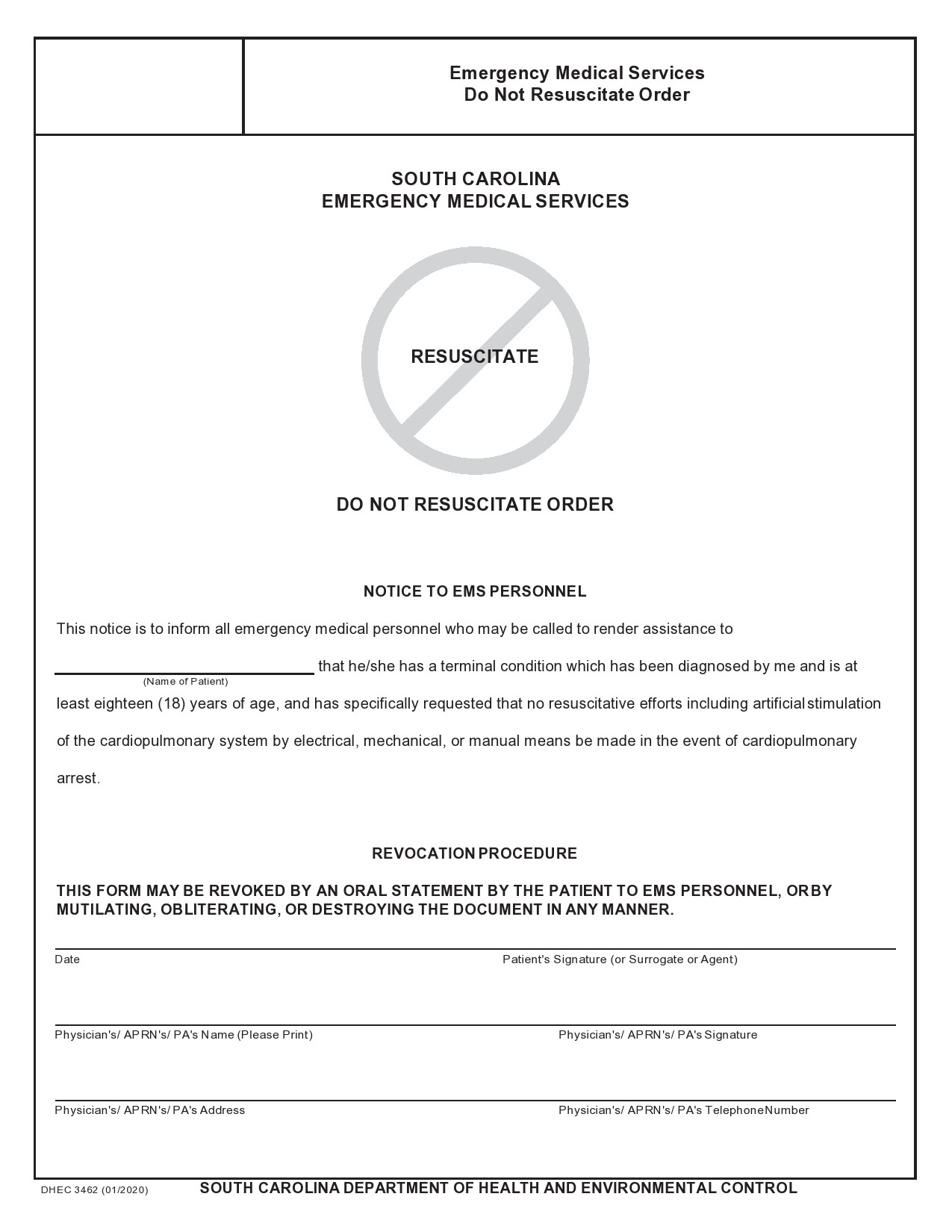
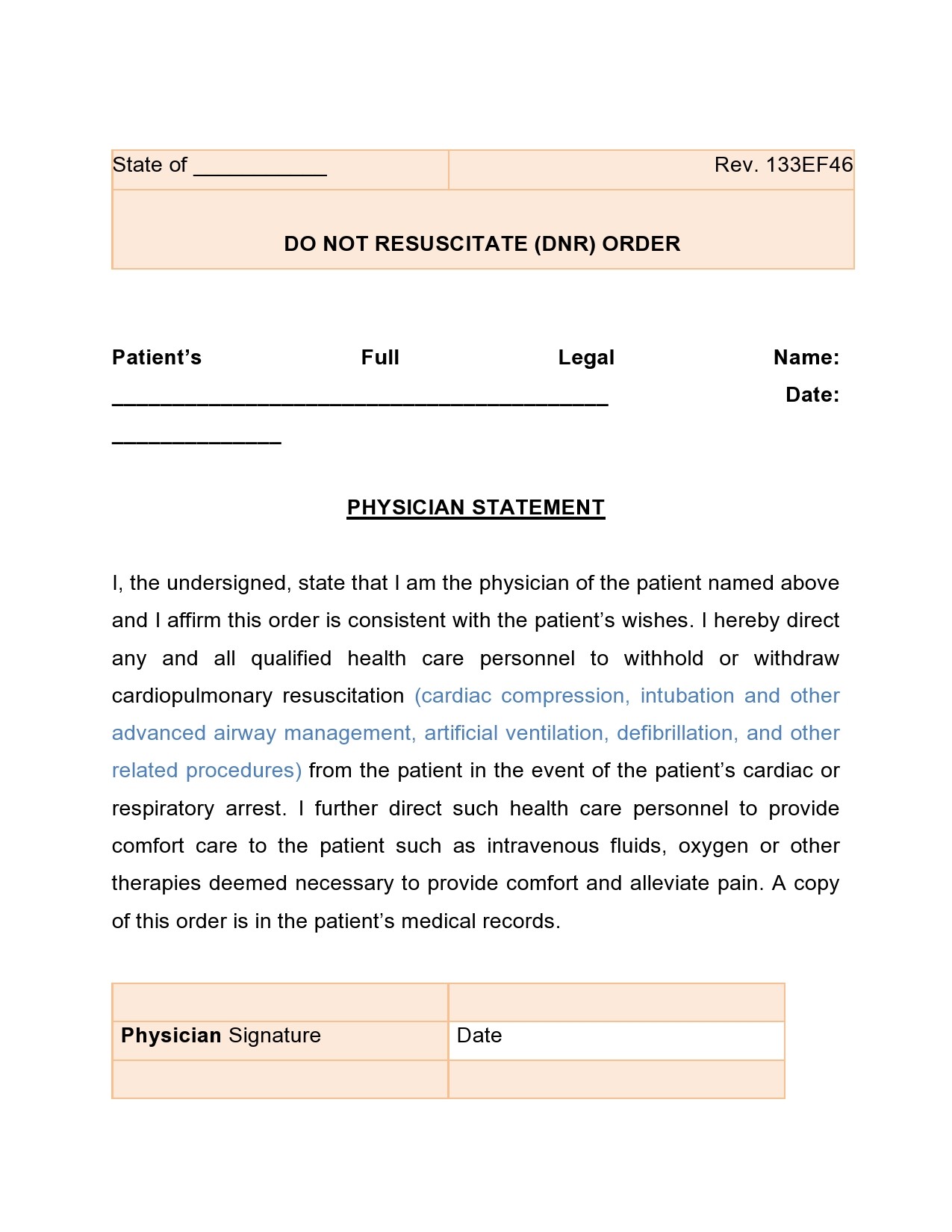
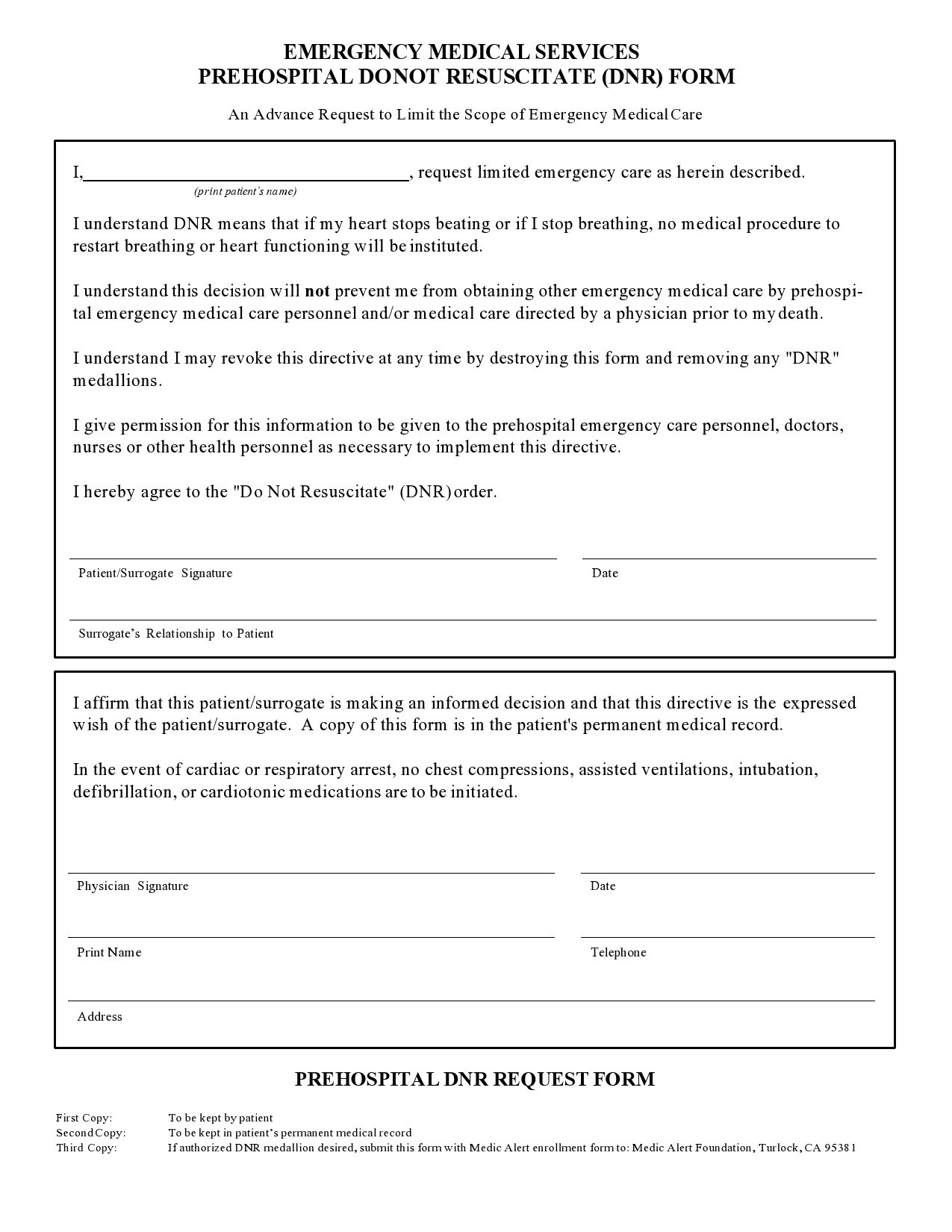
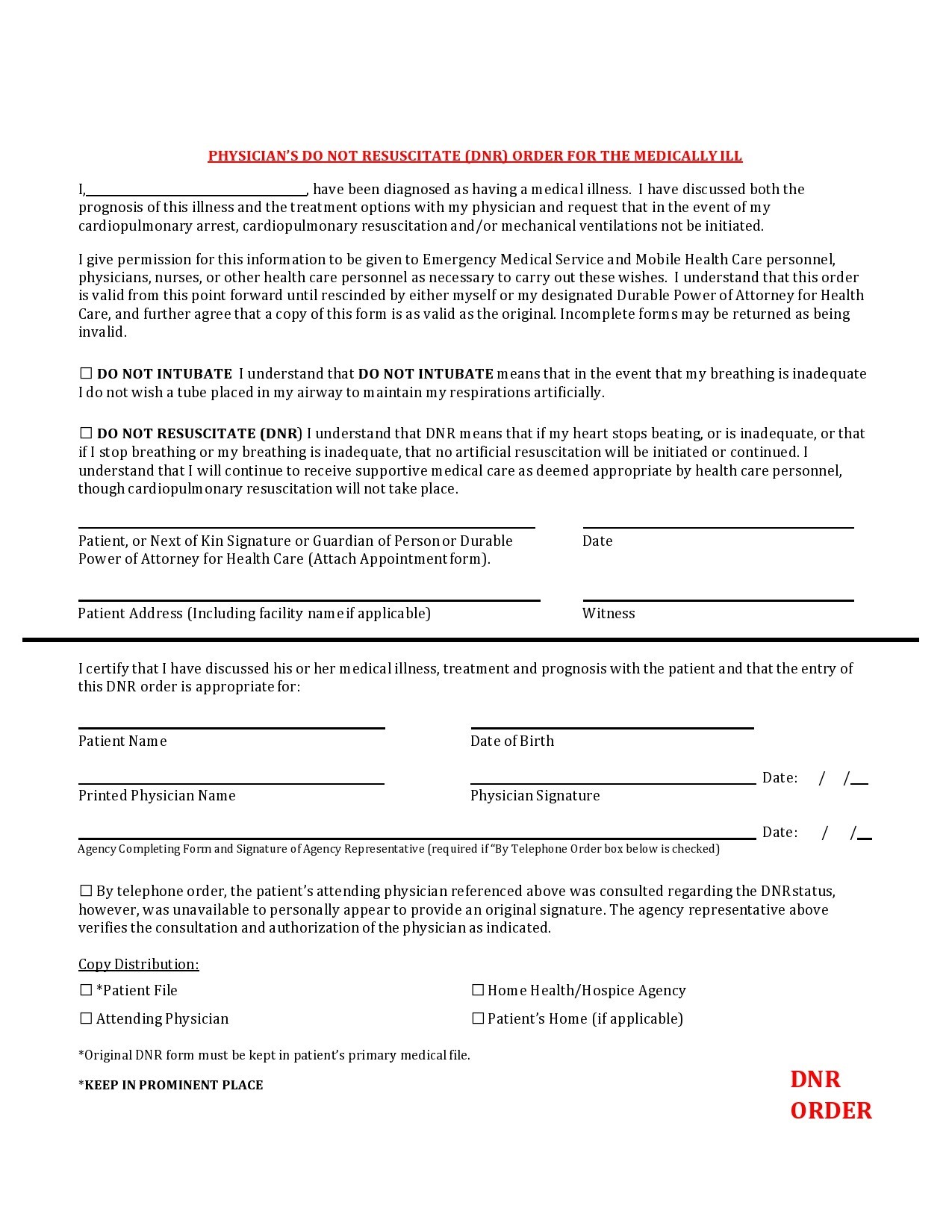
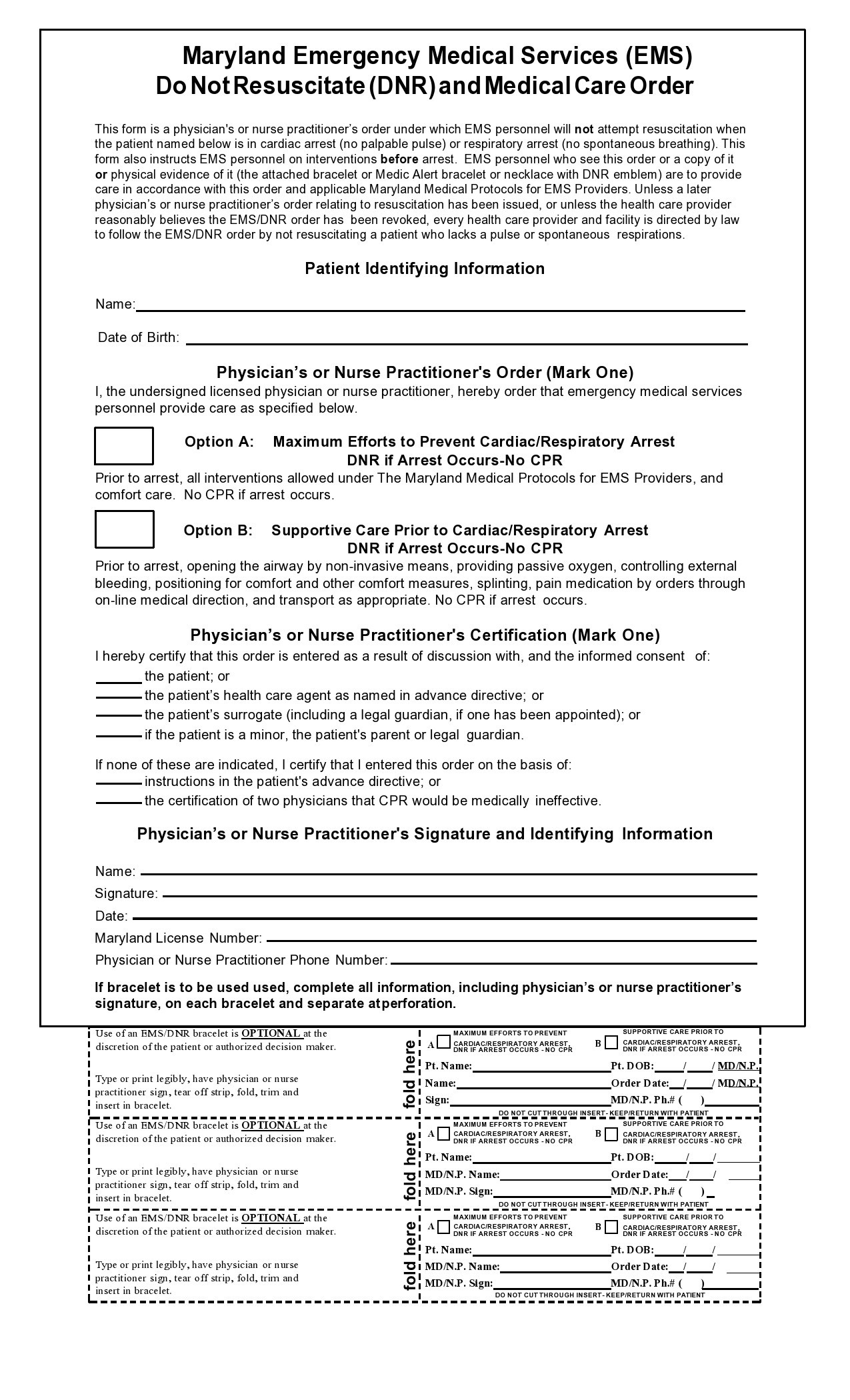
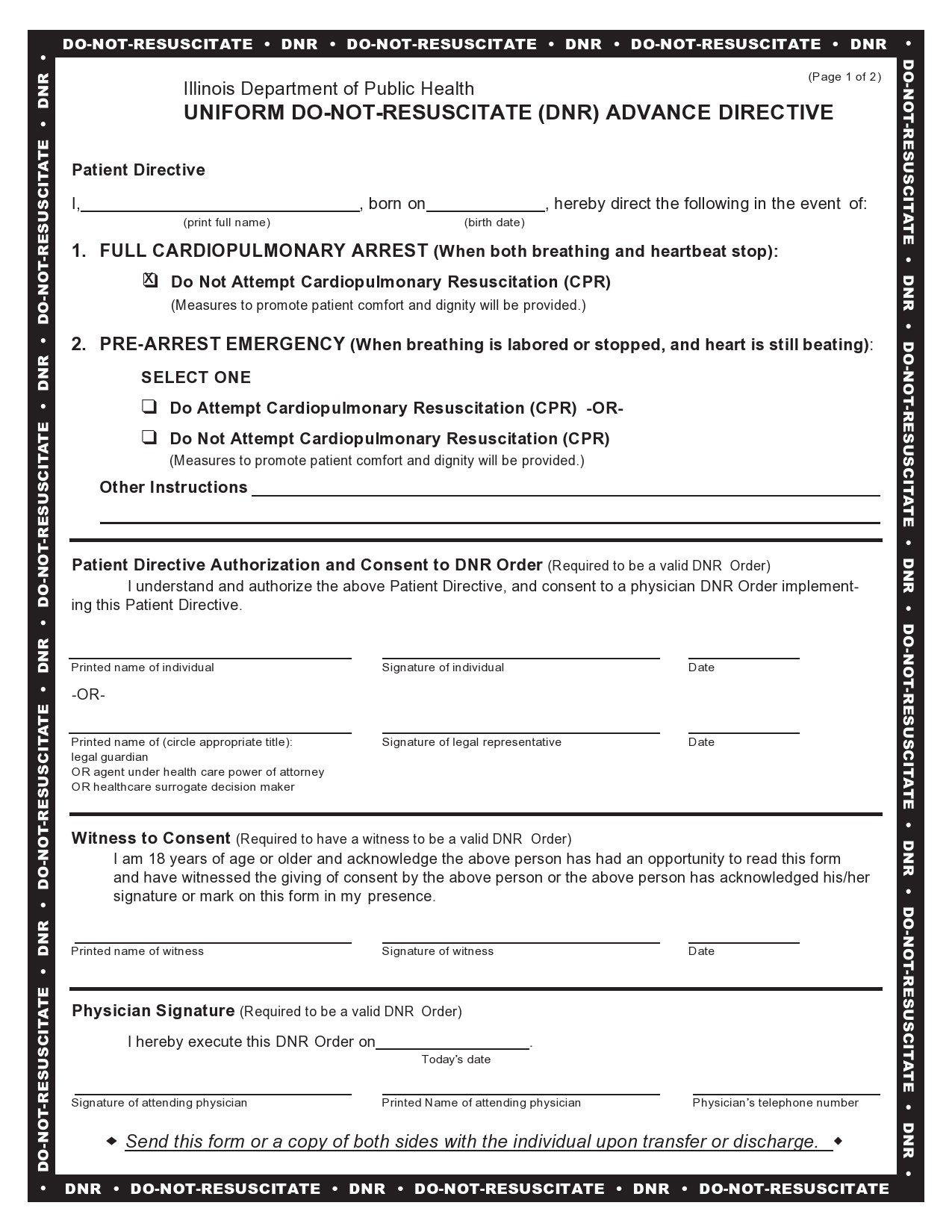
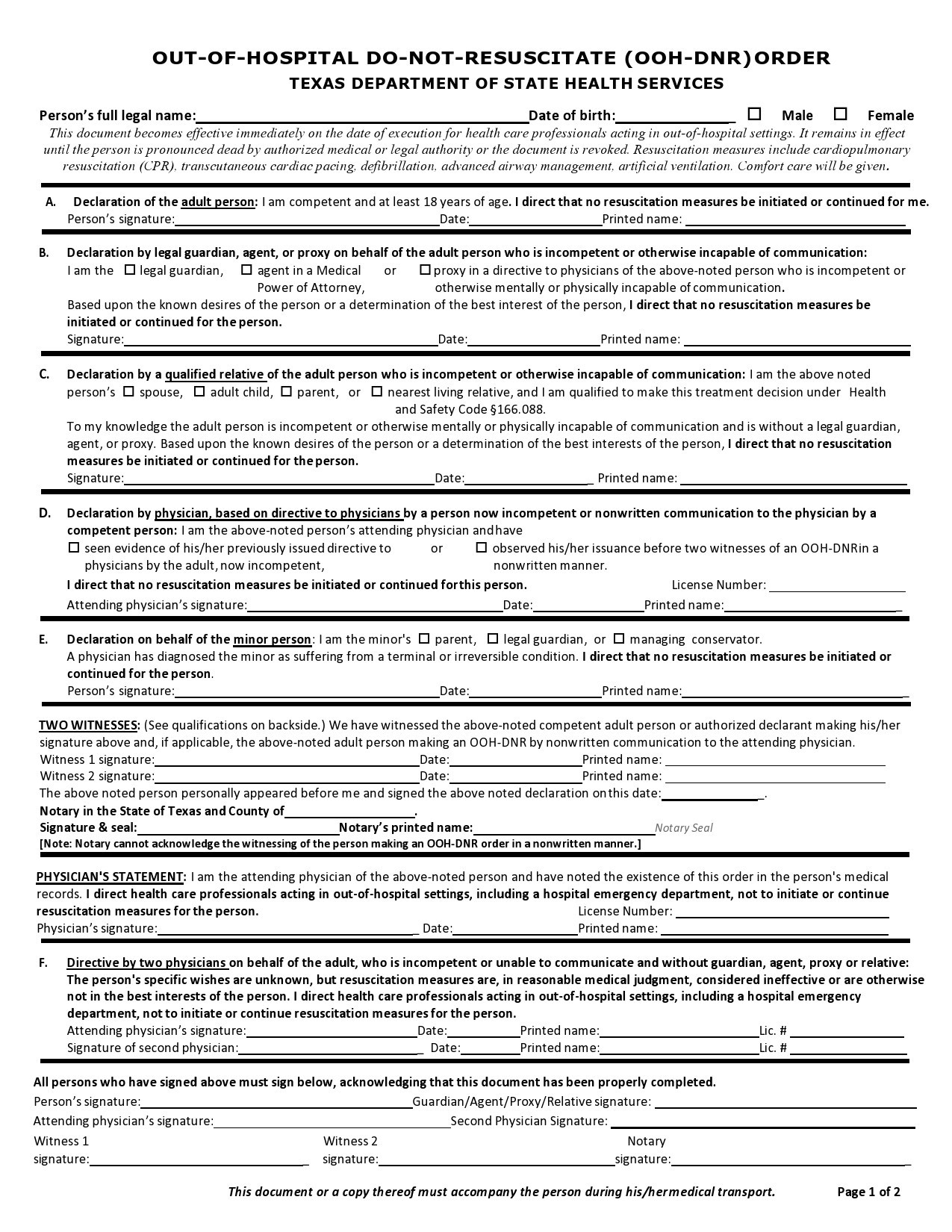
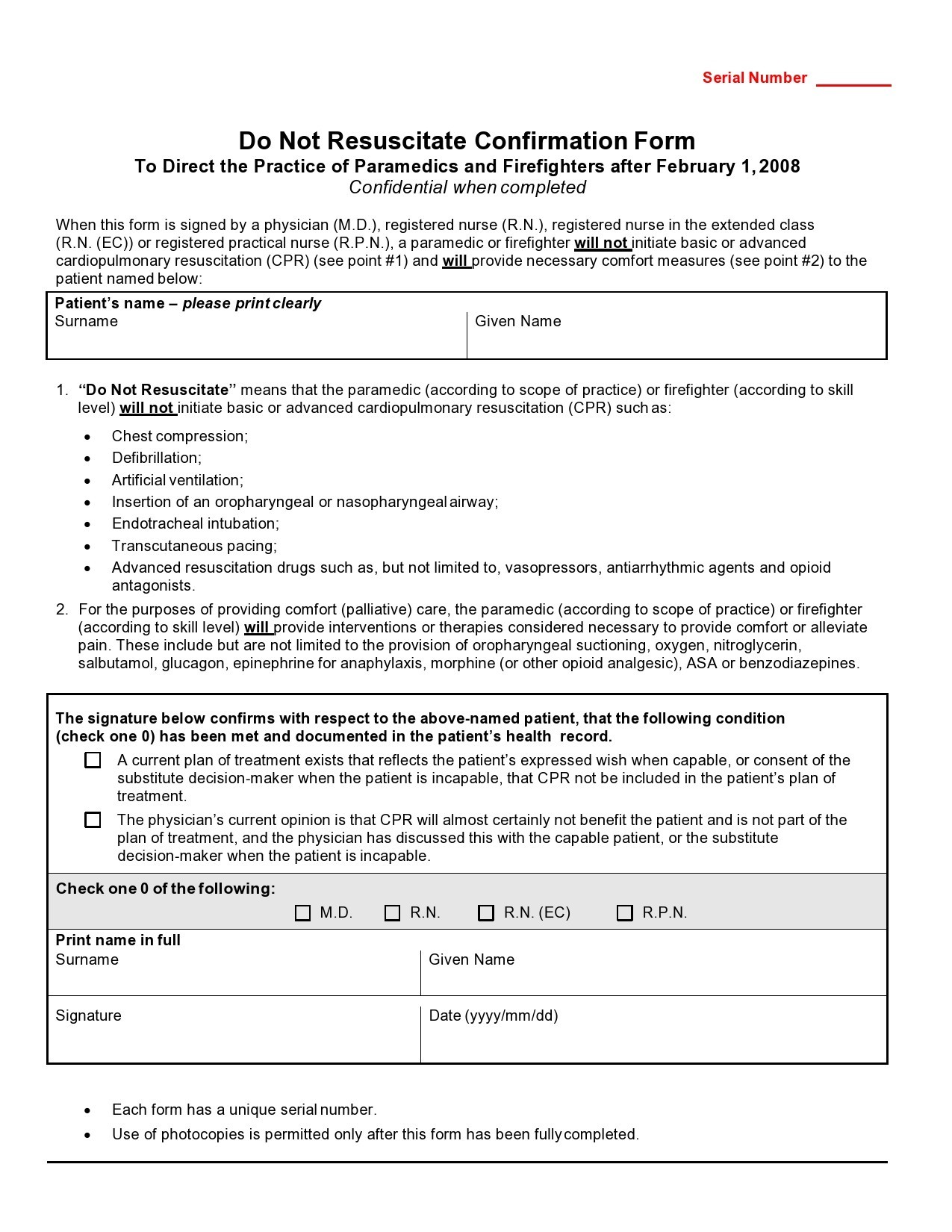
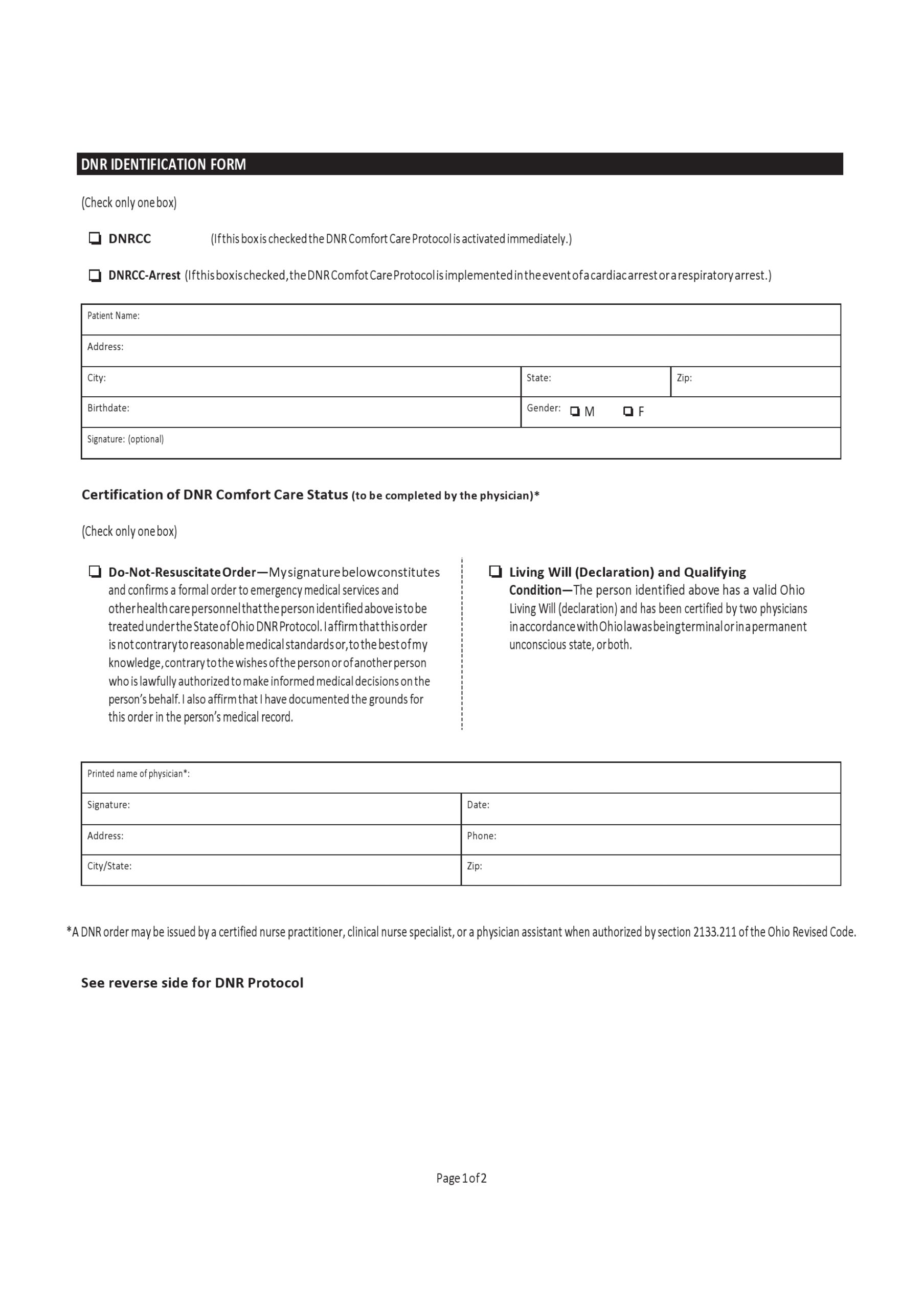
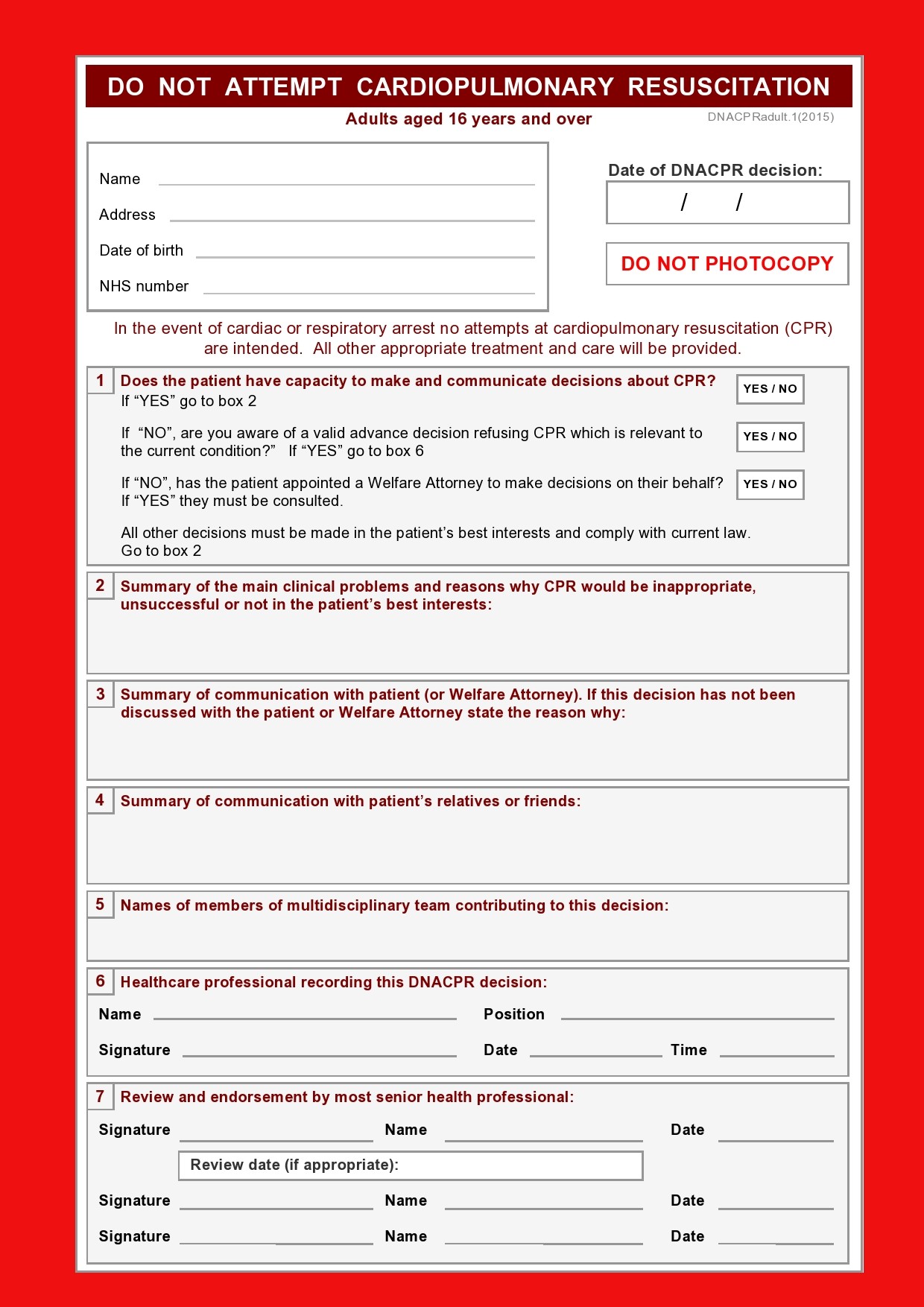
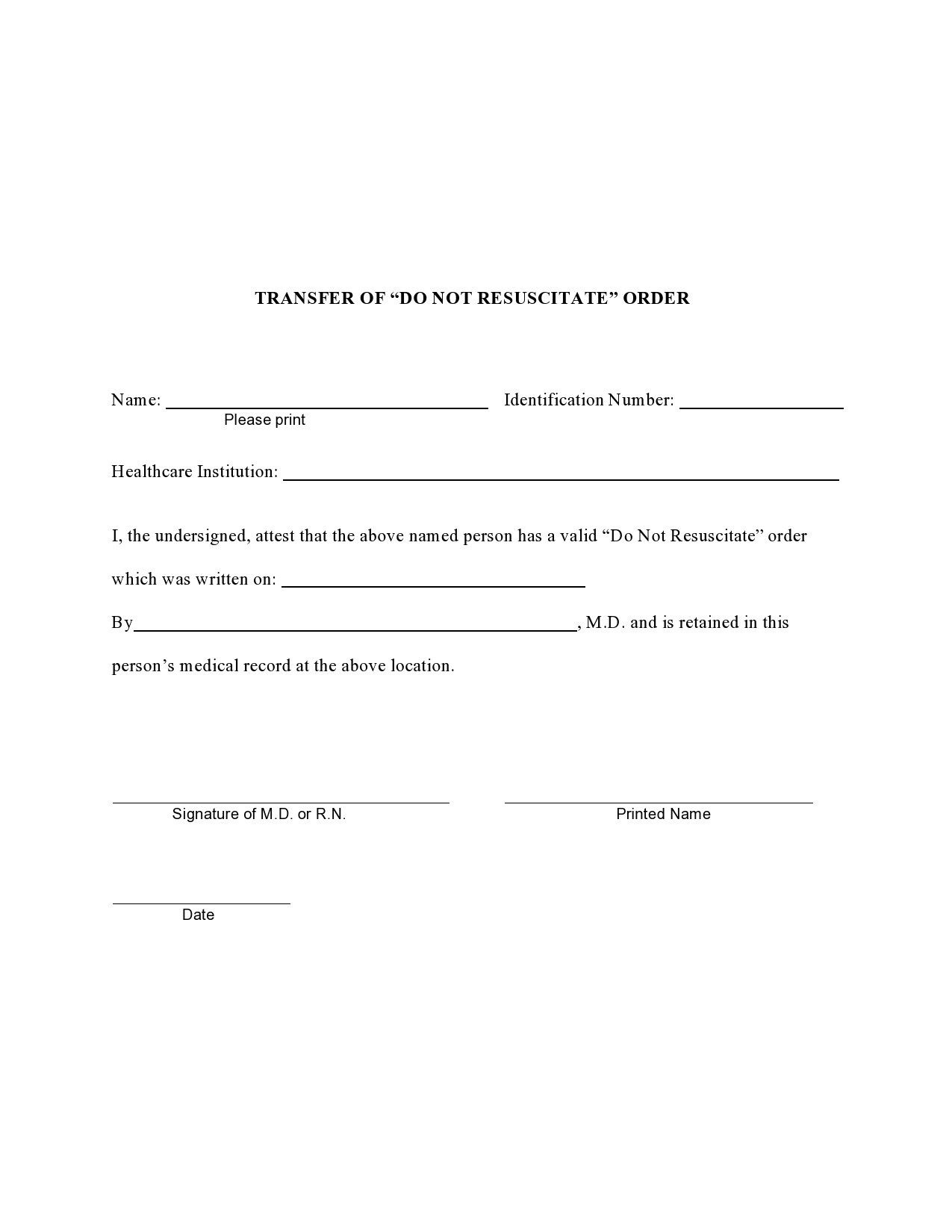
Doctors create a do not resuscitate form and it serves as an instruction for health care providers not to perform Cardiopulmonary Resuscitation (CPR) should a patient stop breathing or their heart stops beating. In an ideal situation, a DNR order should already exist even before an emergency happens.
Table of Contents
Do Not Resuscitate Forms
What does not for resuscitation mean?
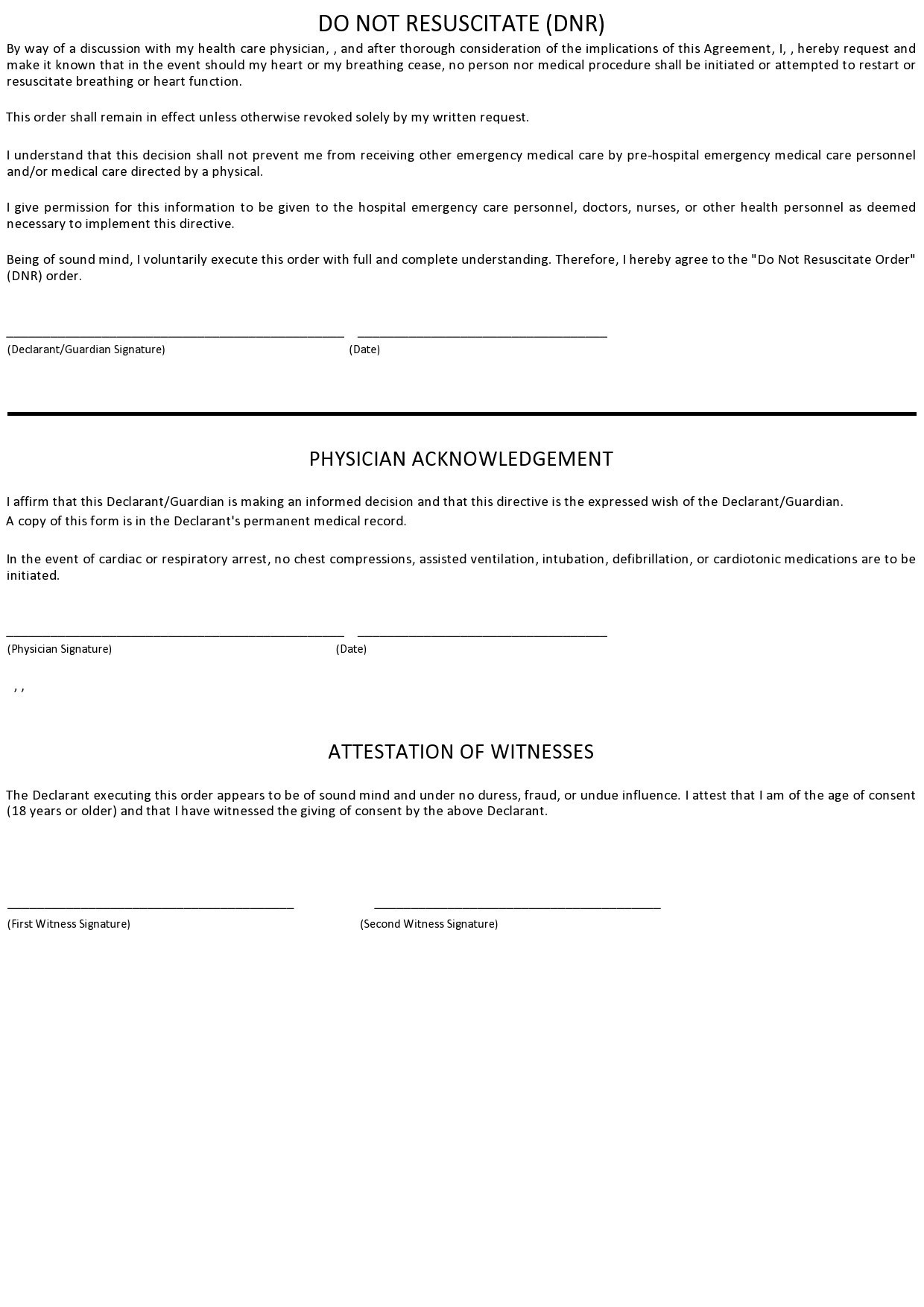
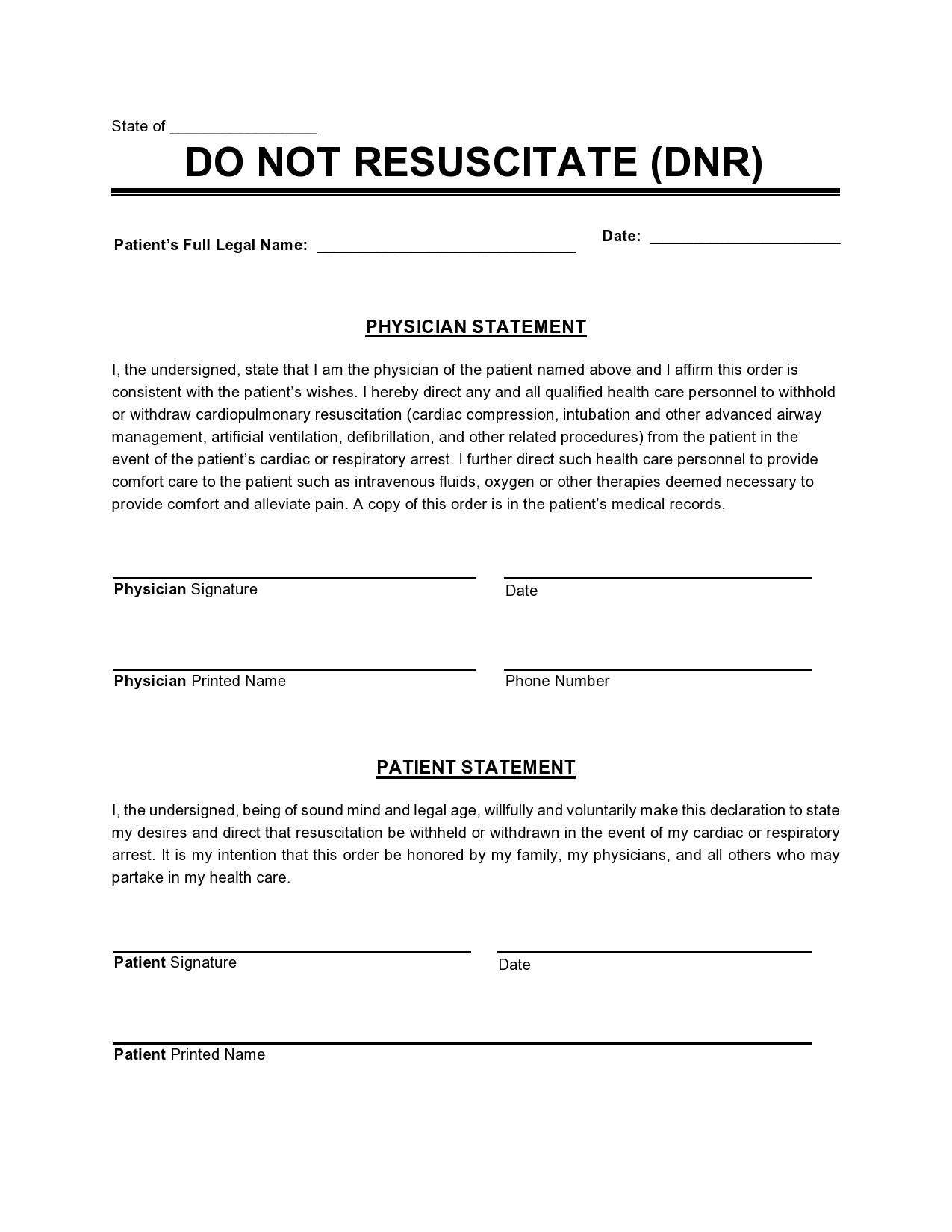
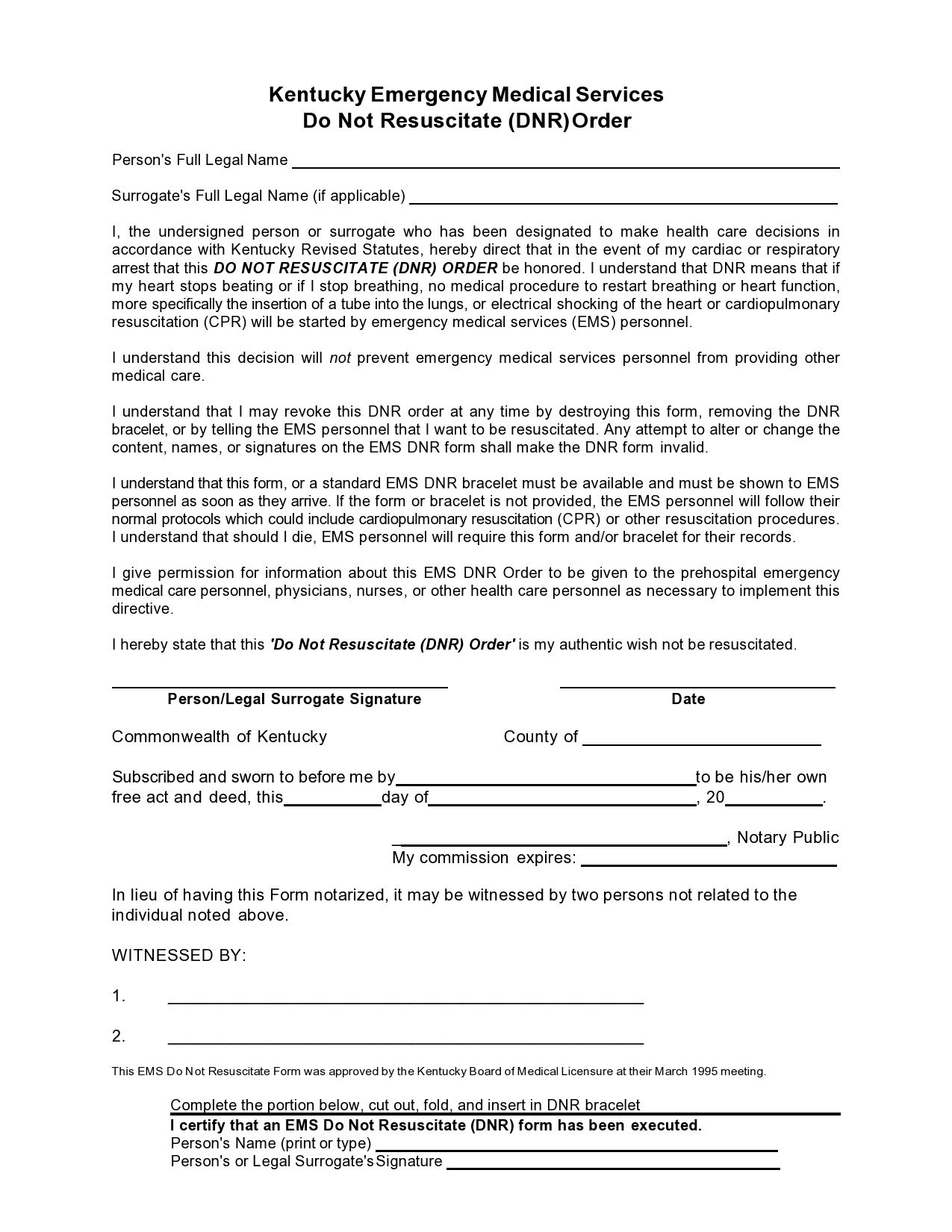
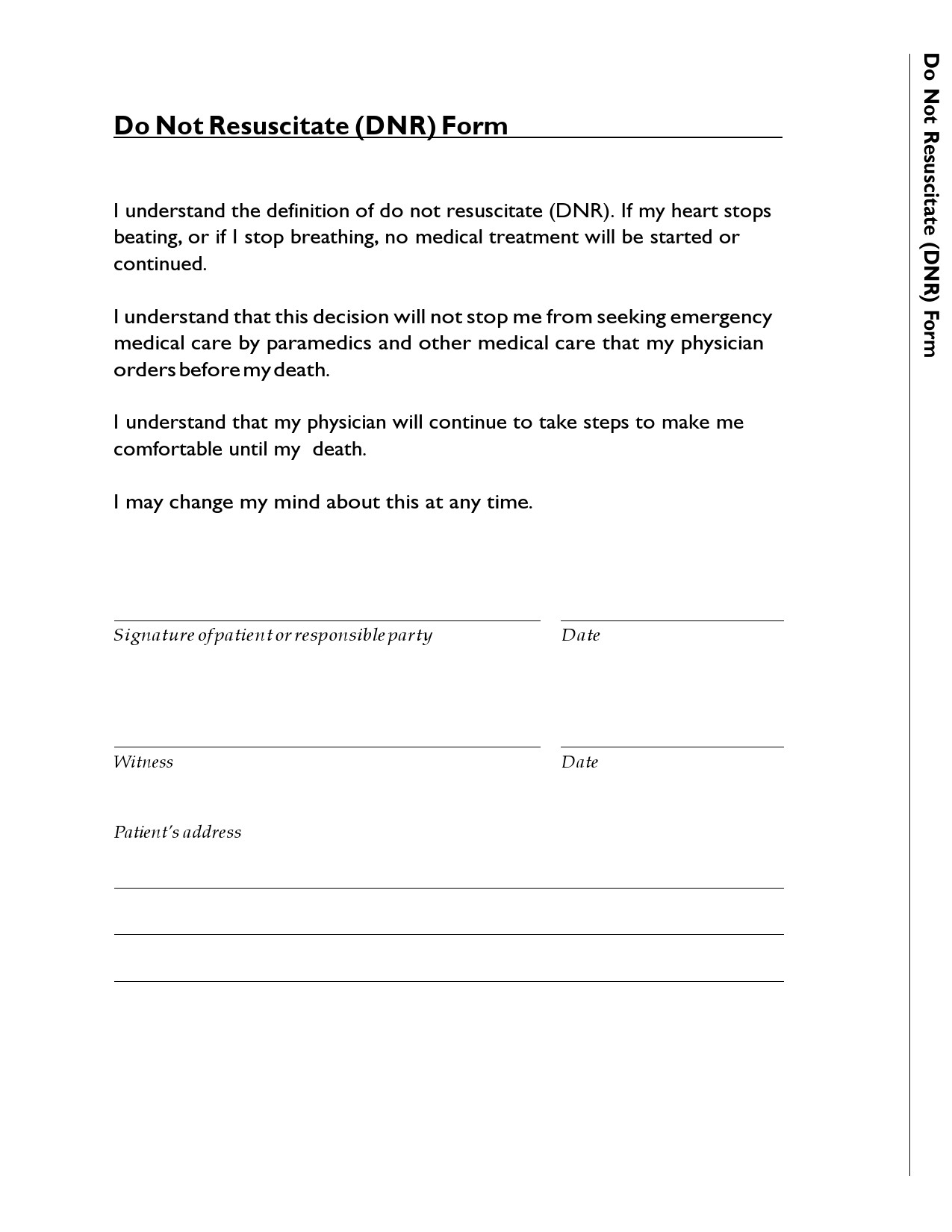
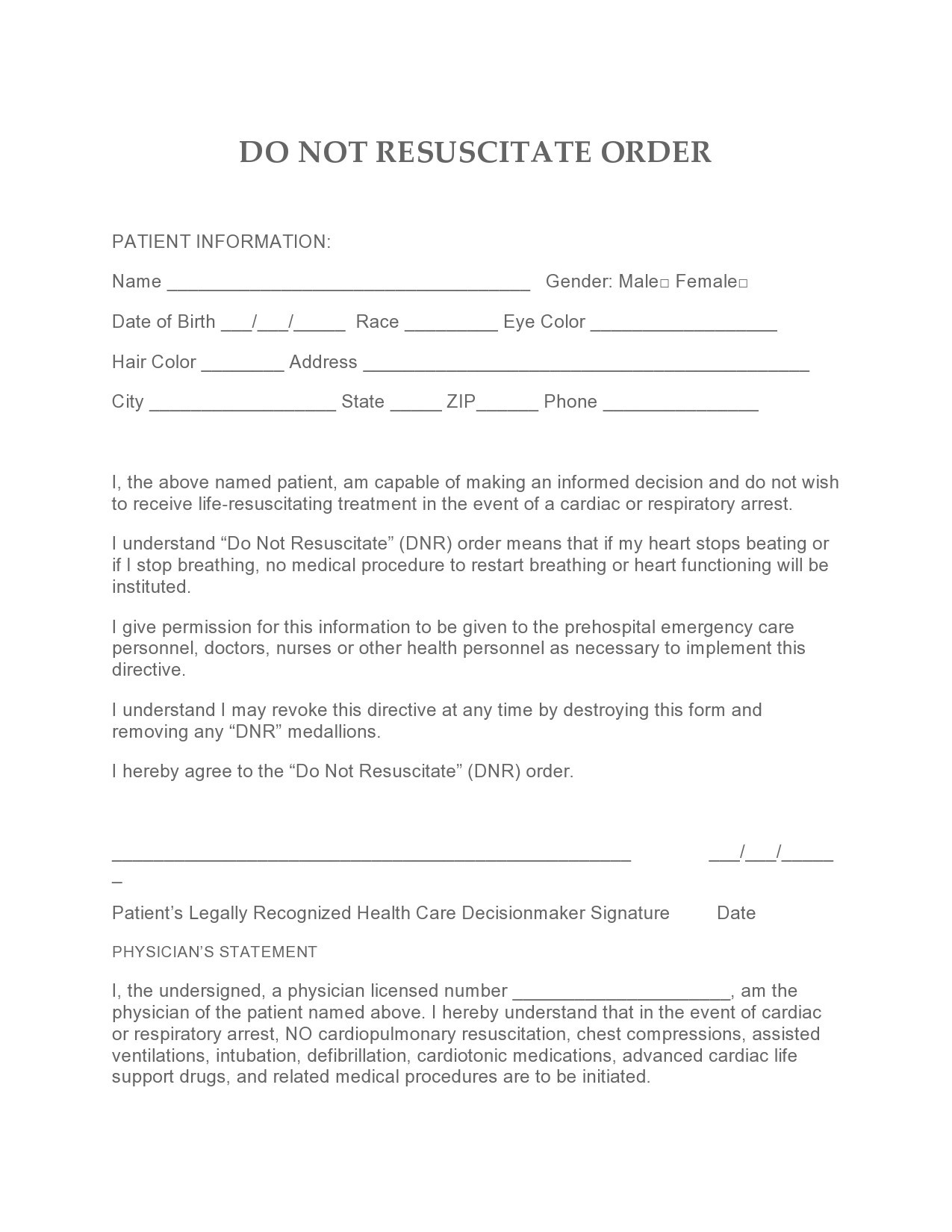
A do not resuscitate form is an official order. It is either oral or written, depending on your country and it specifies that an individual doesn’t want to receive cardiopulmonary resuscitation should their heart stop beating.
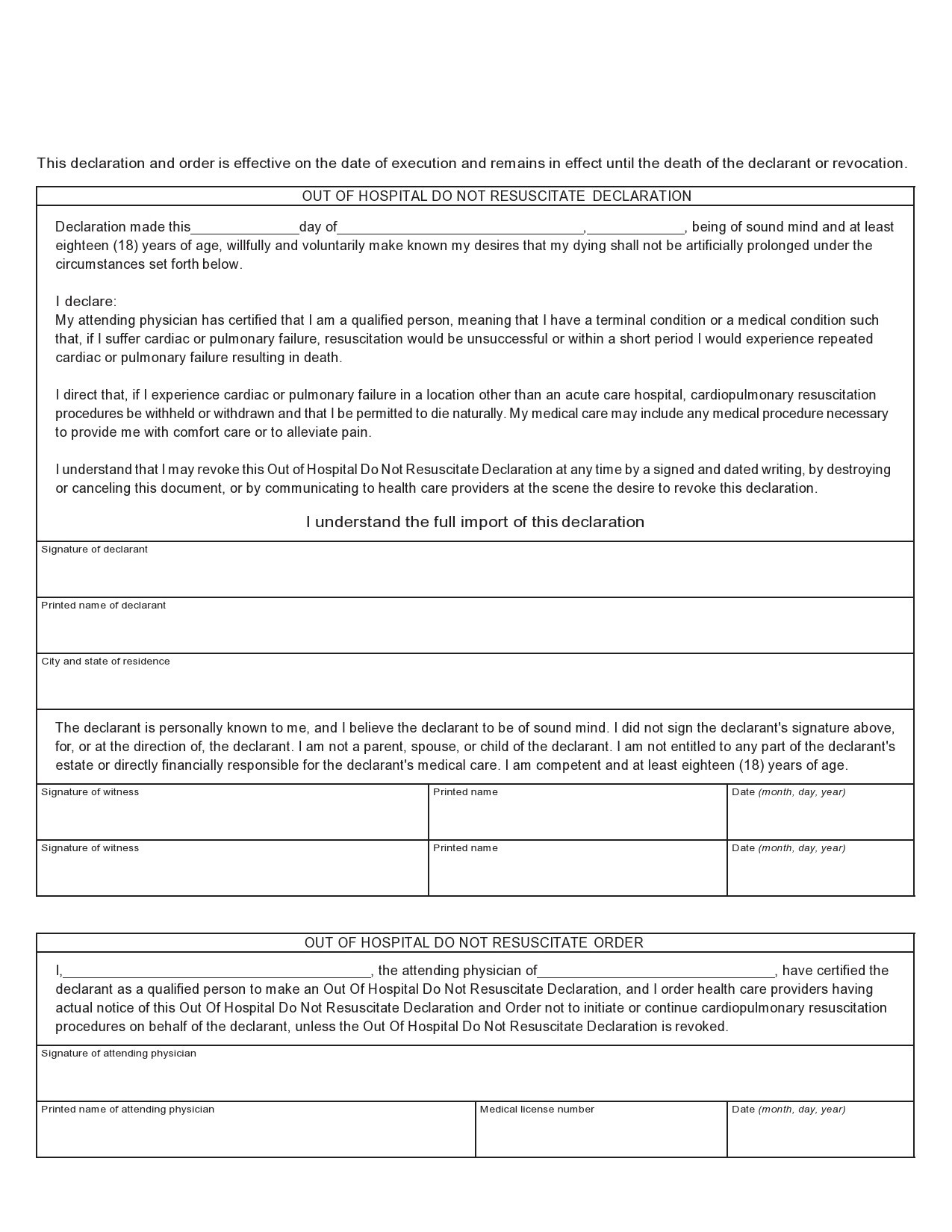
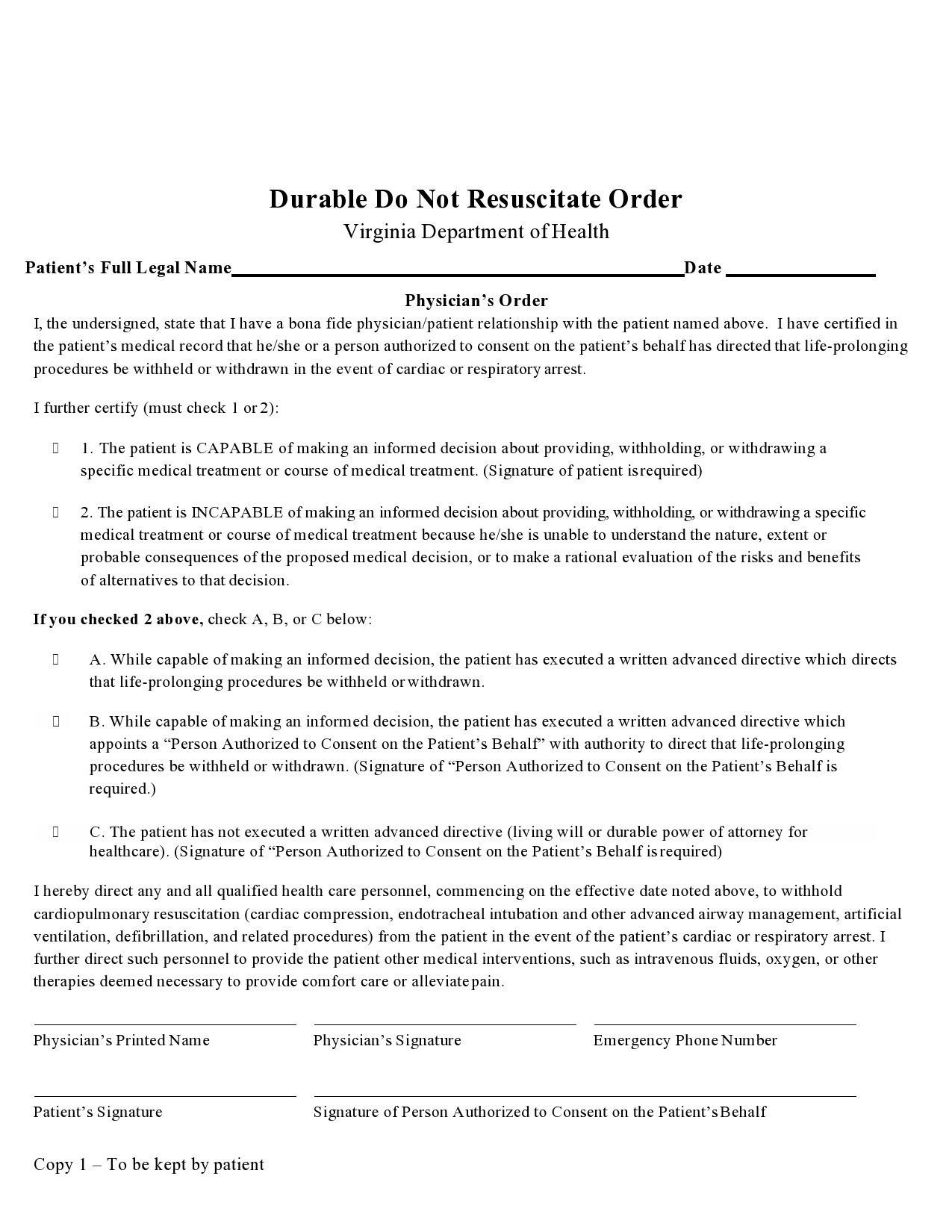
Sometimes, the DNR medical form can also prevent other medical interventions. The legal processes and statuses that surround these orders may vary. Usually, though, the order comes from a doctor based on a combination of their medical judgment and the values and wishes of the patient.
When explaining a DNR document, medical institutions describe it in the context of survival from CPR so that they can address the outcomes and concerns of their patient. Based on the information in this document, they compare the survival of patients who have multiple chronic illnesses
Such illnesses may include patients with liver disease, lung, kidney or heart disease, widespread infection, cancer, and nursing home residents. Studies show that:
- For patients suffering from diabetes, heart disease, kidney diseases, or multiple chronic illnesses, the survival rate after CPR is close to or the same as the average CPR survival rate
- For patients with liver disease, kidney disease, widespread infection, or cancer, the survival rate after CPR is half as good as the average rate.
- For residents in nursing homes, the survival rate after CPR is about half to three-quarters of the average rate. But these nursing homes and similar health facilities that have AEDs usually have a survival rate that is twice as high as the average survival rate compared to other nursing homes overall. Unfortunately, very few nursing homes have AEDs.
Most patients who consider DNR orders know the risks involved in cardiopulmonary resuscitation or CPR. If you’re considering signing such an order, you should know that these risks include:
- Physical injuries like broken bones affect 13% of all CPR patients. An unknown number of individuals have experienced broken cartilages, which sound a lot like breaking bones.
- Some patients sustain mental problems both after and before CPR. These include:
1 or more people in every 100 survivors go into comatose after CPR but most of them come out of it.
5 to 10 people in every 100 survivors need more assistance with their daily lives compared to when they didn’t receive CPR.
5 to 21 people in every 100 survivors experience mental decline but still remain independent.
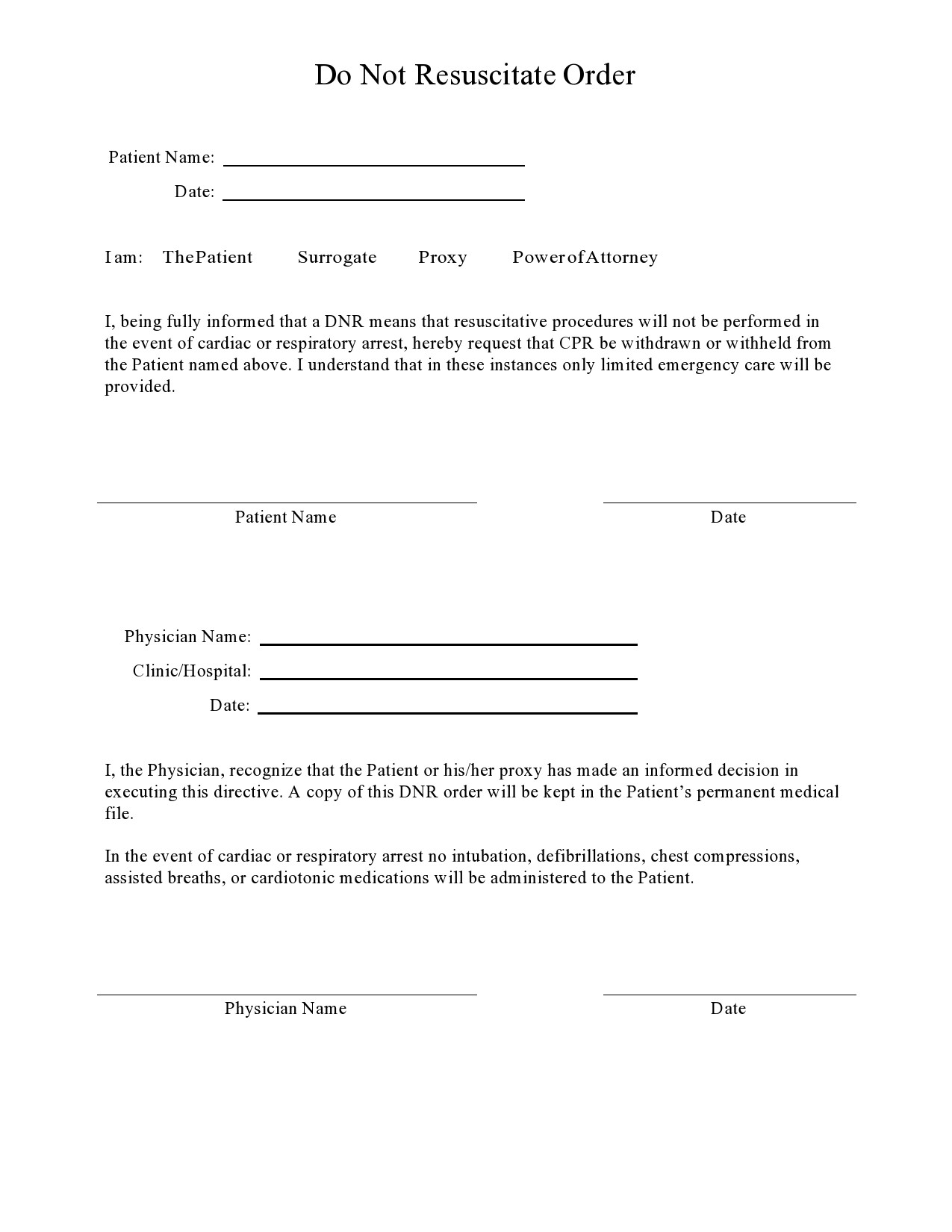
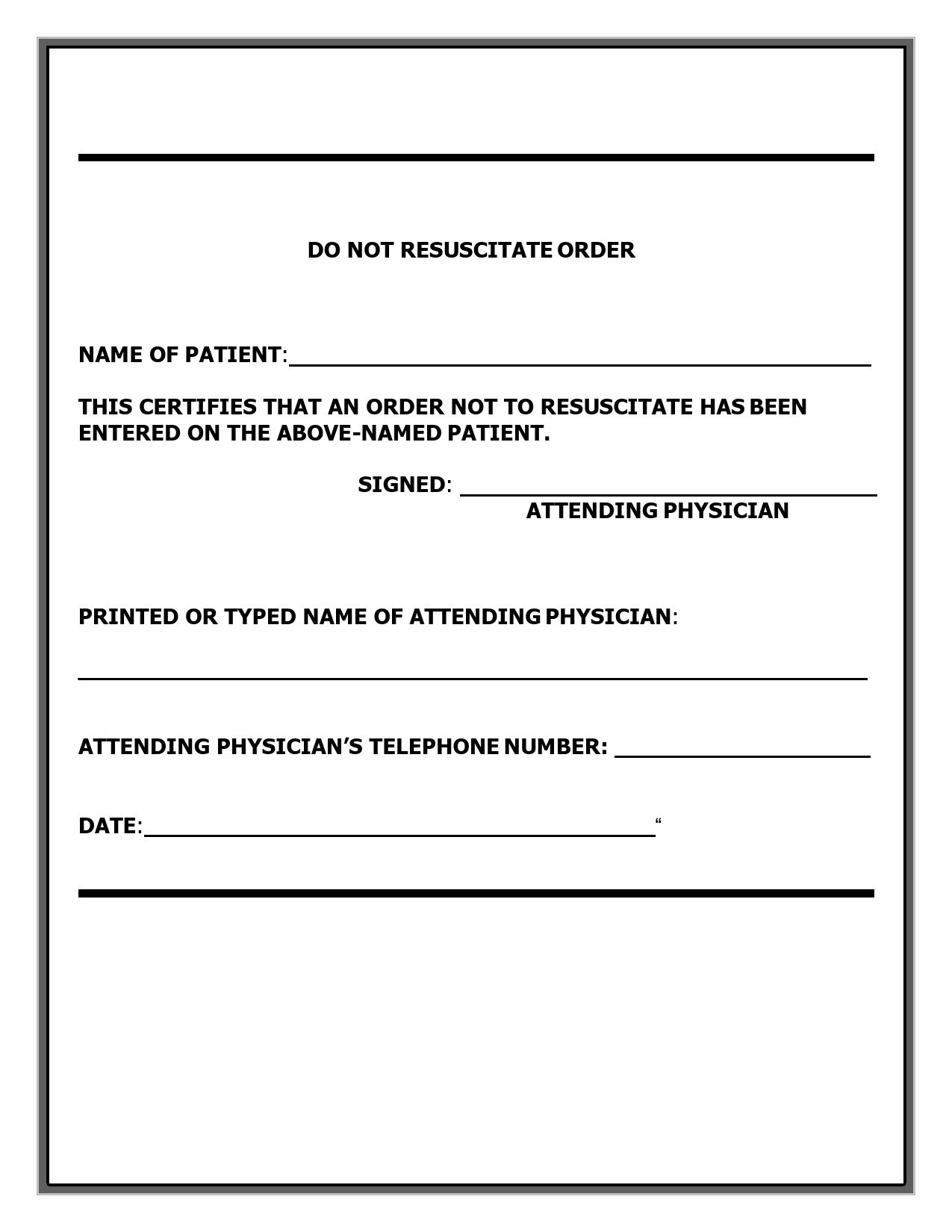
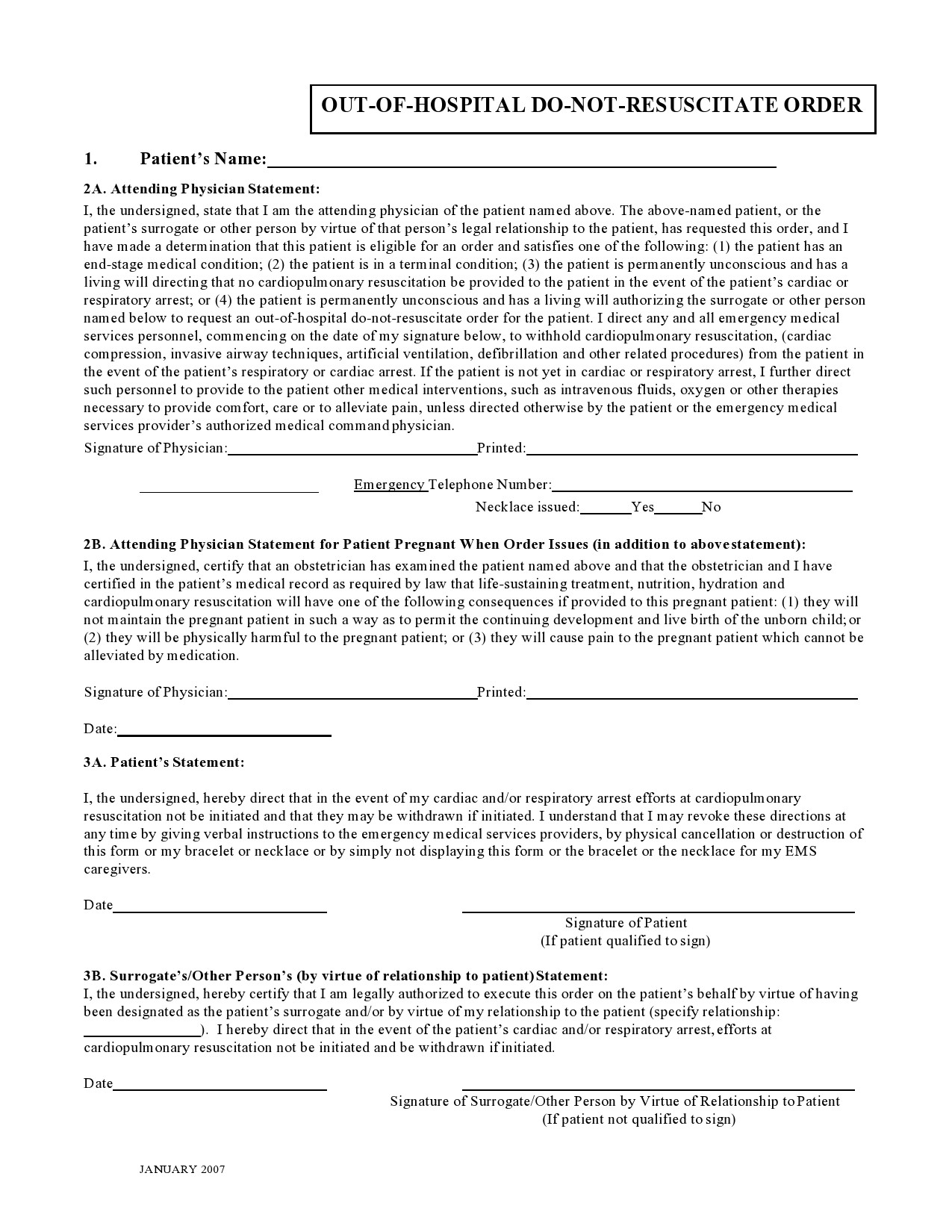
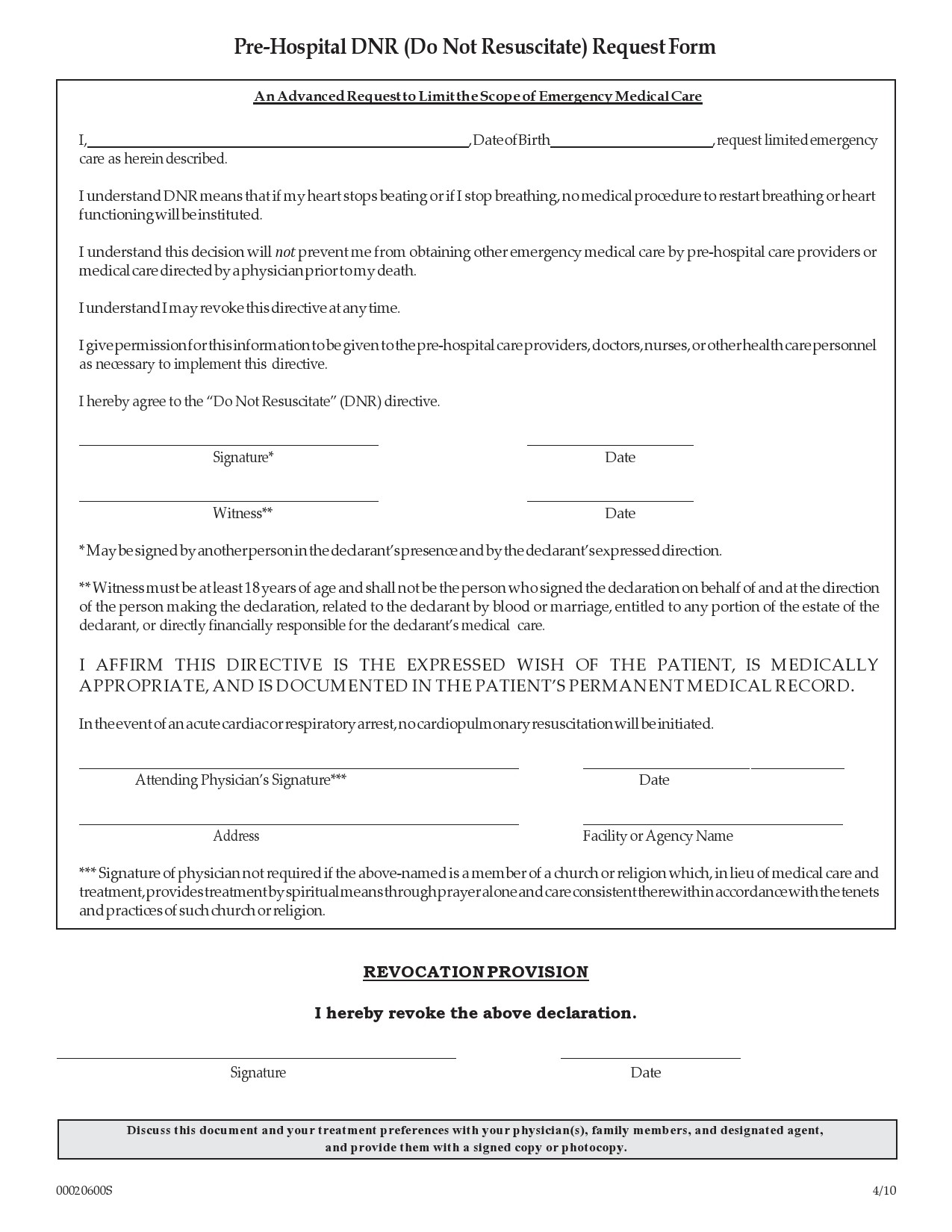
DNR Forms
Different types of advanced directives
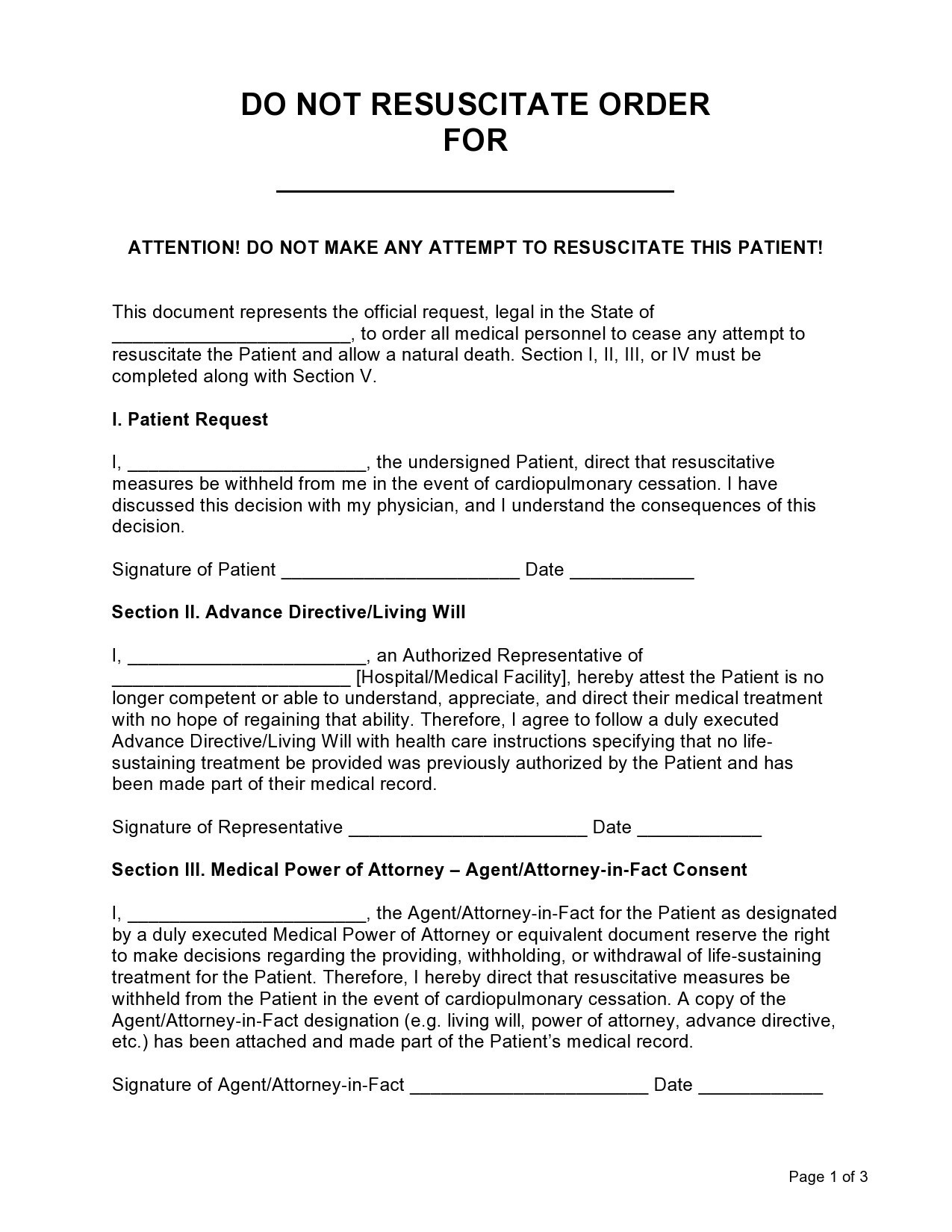
Advance directives are the various types of treatment you might want depending on your condition. Aside from the do not resuscitate form, these advance directives can:
- Describe the type of care you choose if you’re suffering from an illness you might not recover from.
- Describe the type of care you will receive should you become permanently unconscious.
- Inform the physician that you don’t want any type of treatment or conversely, you want a specific type of treatment no matter how dire your illness is
Before you opt for a printable do not resuscitate form, you should consider other advanced directives including:
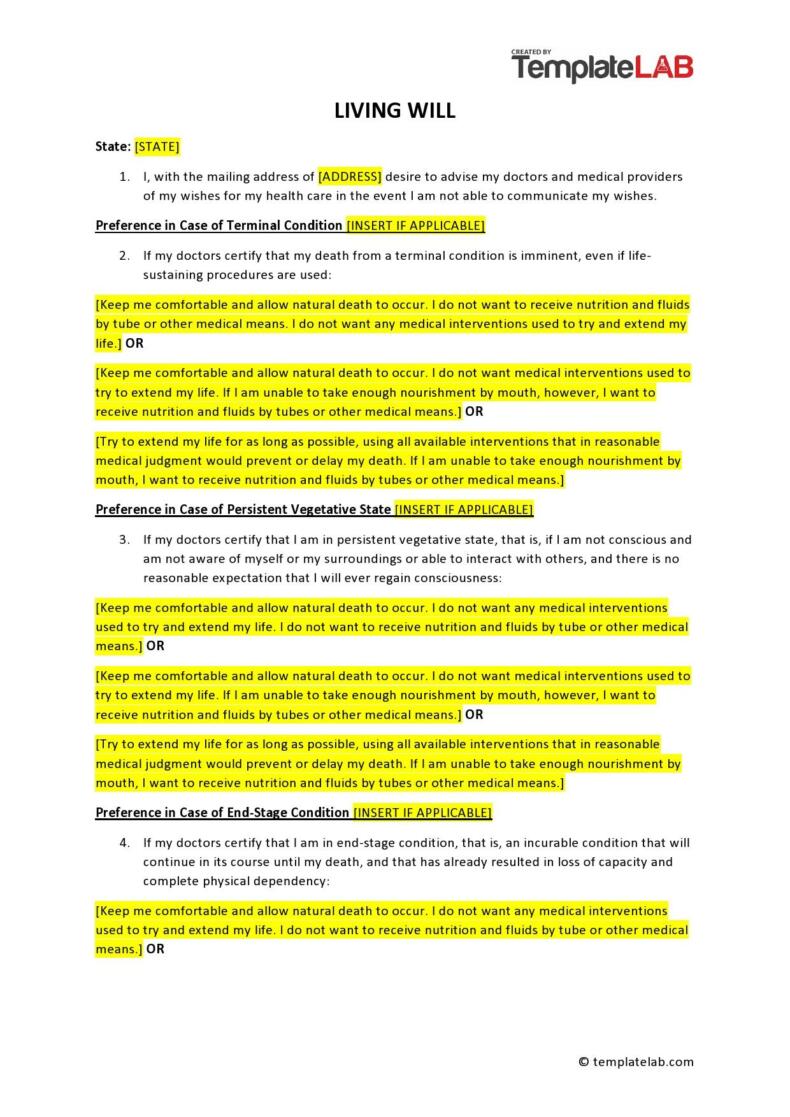
- Living Will
This is a written document that describes what treatments you want if you’re either permanently unconscious or terminally ill. These treatments can come in the form of medical treatments to help you live longer. A living will doesn’t let you choose someone else to decide on your behalf. - Durable Power of Attorney (for health care)
Also called the Medical Power of Attorney this advanced directive specifies whom you have chosen to make decisions on your behalf. It becomes applicable anytime you become unconscious or you aren’t able to make medical decisions.
In general, the DPA is more useful compared to a living will. However, it may not be the best choice if you don’t have a person you can entirely trust to make decisions for you.
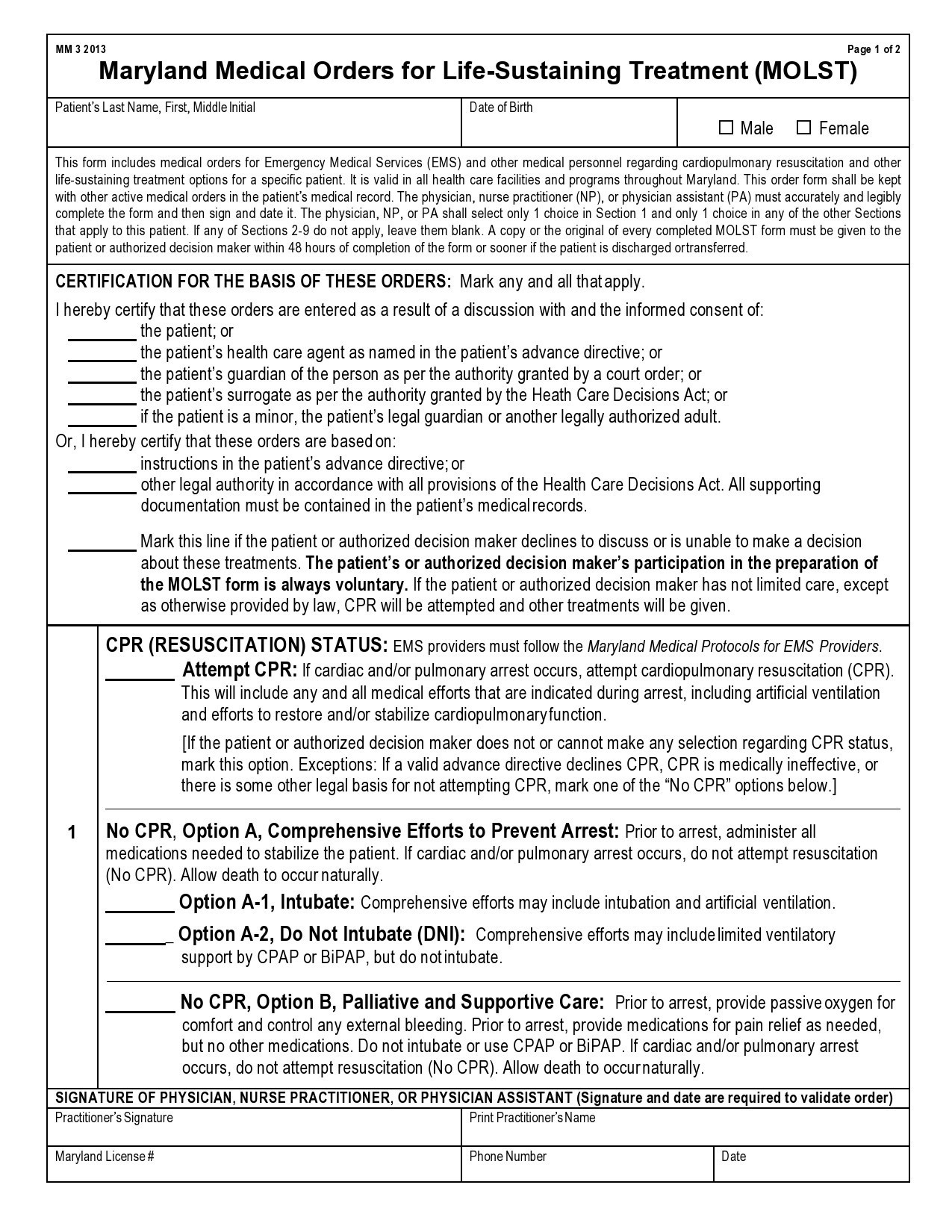
The laws governing advanced directives vary in each state. DPAs and living wills are legally recognized in most states. Therefore, it is essential to check with your state laws regarding this matter. But you can still use this as a guide for your loved ones and your physician if you become incapable of making decisions with regards to your medical care. - Physician Orders for Life-Sustaining Treatment (POLST)
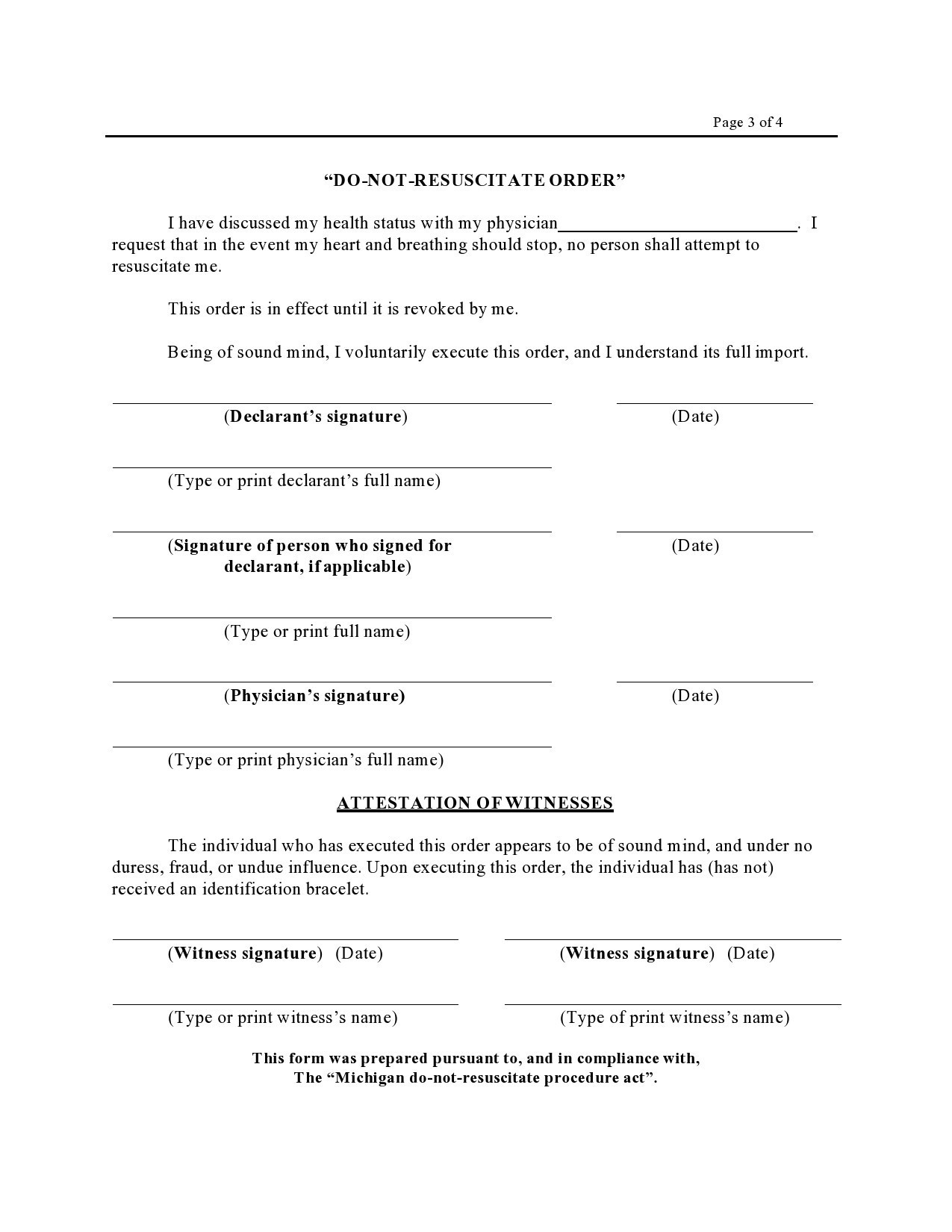
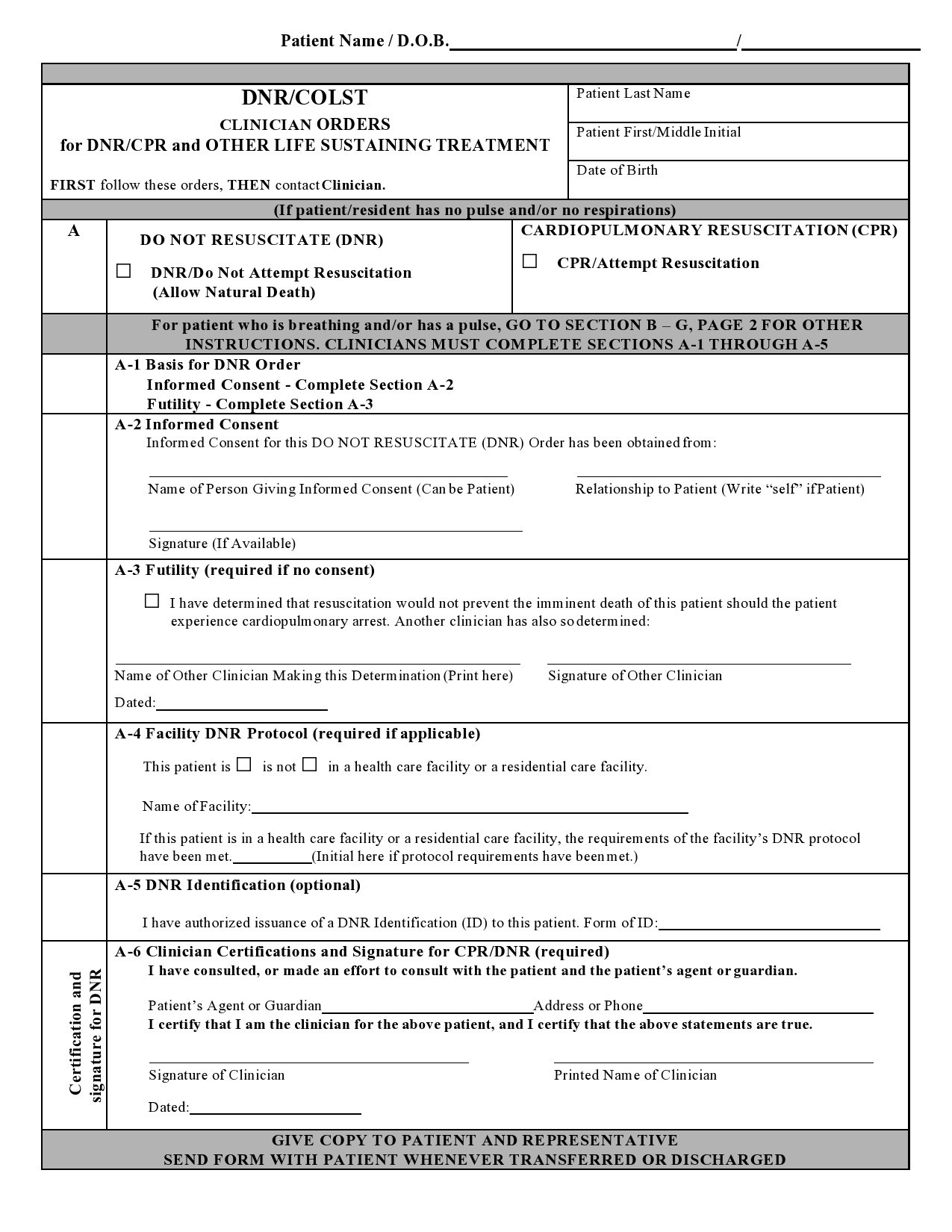
This can apply to you if you receive a diagnosis for a serious illness. This holds the responsibility for filling out this document. Remember that this isn’t a replacement for other types of advance directives. Rather, it will stay with you to make sure that you get the type of medical treatment you want. - Do Not Resuscitate Order
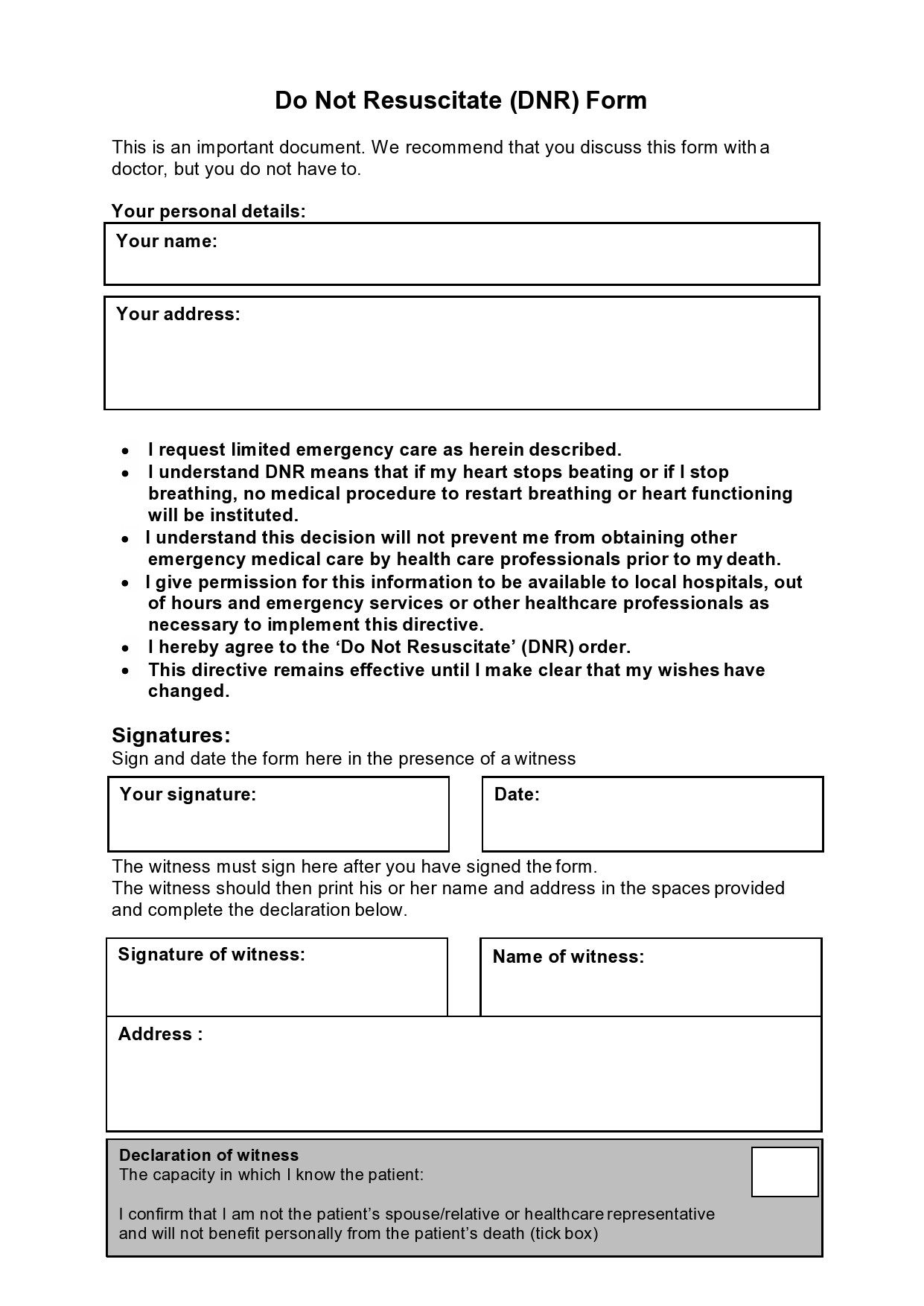
This is a request not to administer CPR if you stop breathing or if your heart stops. You may use an advanced direction form or just tell your physician that you do not want CPR. The physician will then note your request on your medical chart.
DNR orders are generally accepted by hospitals and doctors in all states. They don’t need to be part of other types of advanced directives like a living will. Other probable end-of-life issues that you can address using this document include:
In the case of ventilation, mention if you agree to this and for how long you want a machine to take over your breathing.
In the case of tube feeding, mention if you agree to this and for how long you want to receive your food through an IV or through a tube in your stomach.
In the case of palliative care, mention if you want the doctors to keep you comfortable or manage your pain. This may include dying at home or receiving pain medication.
In the case of organ donation, specify if you want to donate your tissues, organs, or your whole body for research or other patients.
DNR Medical Forms
Can you choose not to be resuscitated?
The answer to this question is, YES. If you’re nearing the end of your life or you discovered that you suffer from an illness that won’t improve, you can decide whether you want the doctors to administer CPR to you or not. In case of the latter, you need a printable do not resuscitate form:
- If you want to receive CPR, you don’t need this form.
- If you don’t want to receive CPR, talk with your doctor about a DNR document.
This can be a difficult choice to make for yourself and the people you love. Unfortunately, there isn’t any fast rule about what you should choose. But it is important to think about your situation while you can still decide for yourself. For instance, you should:
- Learn more about your condition and what you can expect in the future.
- Speak with your doctor regarding the advantages and disadvantages of CPR.
A do not resuscitate form may be part of a hospice care plan. Remember that the focus of this plan isn’t to prolong your life but to ease your symptoms and keep you comfortable. Even if you have this order, you still maintain the right to change your mind and ask for CPR. In some cases, though, you might not get to state your wishes anymore. In such a case:
- Your loved ones cannot override it.
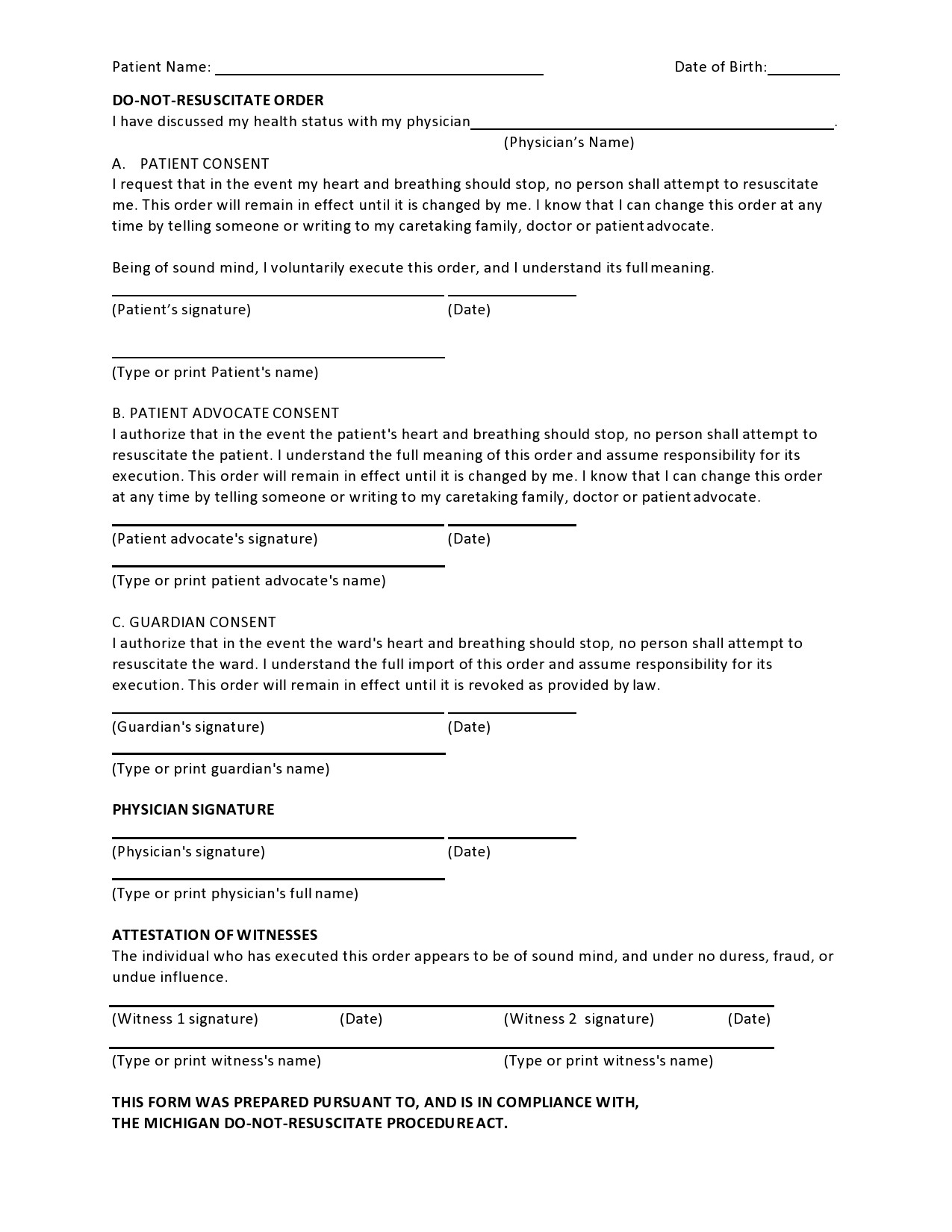
- If you have named a person to make decisions on your behalf, this person can agree to a DNR order for you.
DNR Documents
How to get a DNR form?
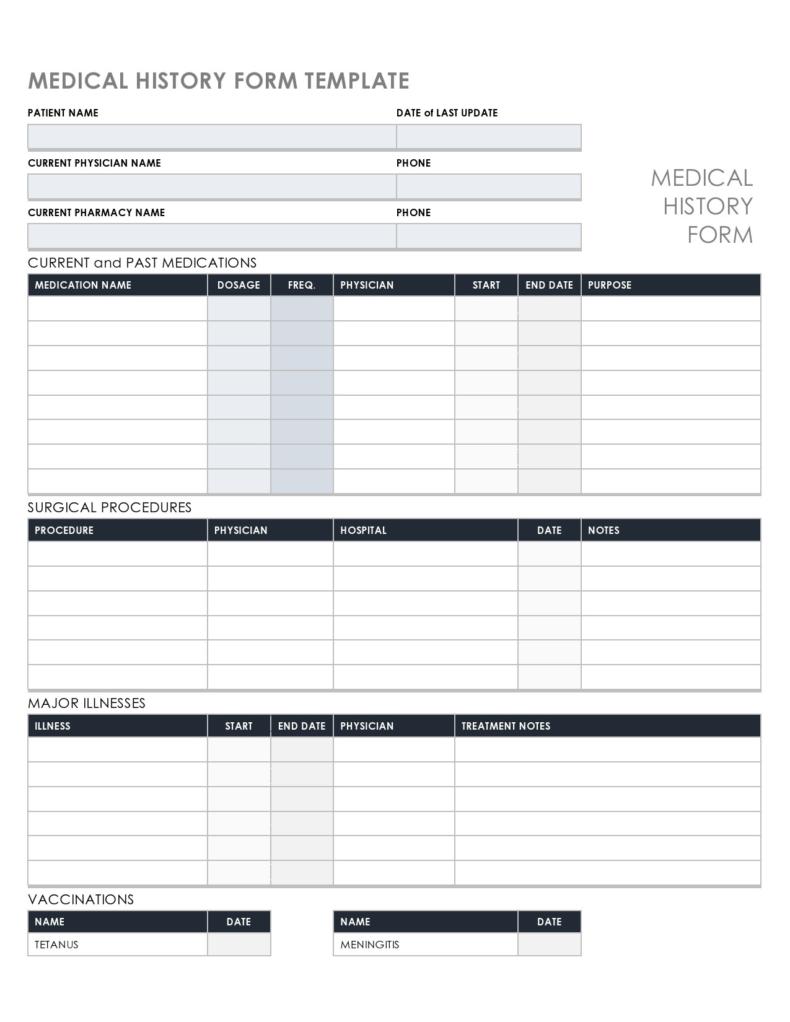
You may include a DNR form with either an advanced directive or a living will. Both of these documents allow you to express your preferences when it comes to end-of-life care in case you cannot communicate what you want when the time comes.
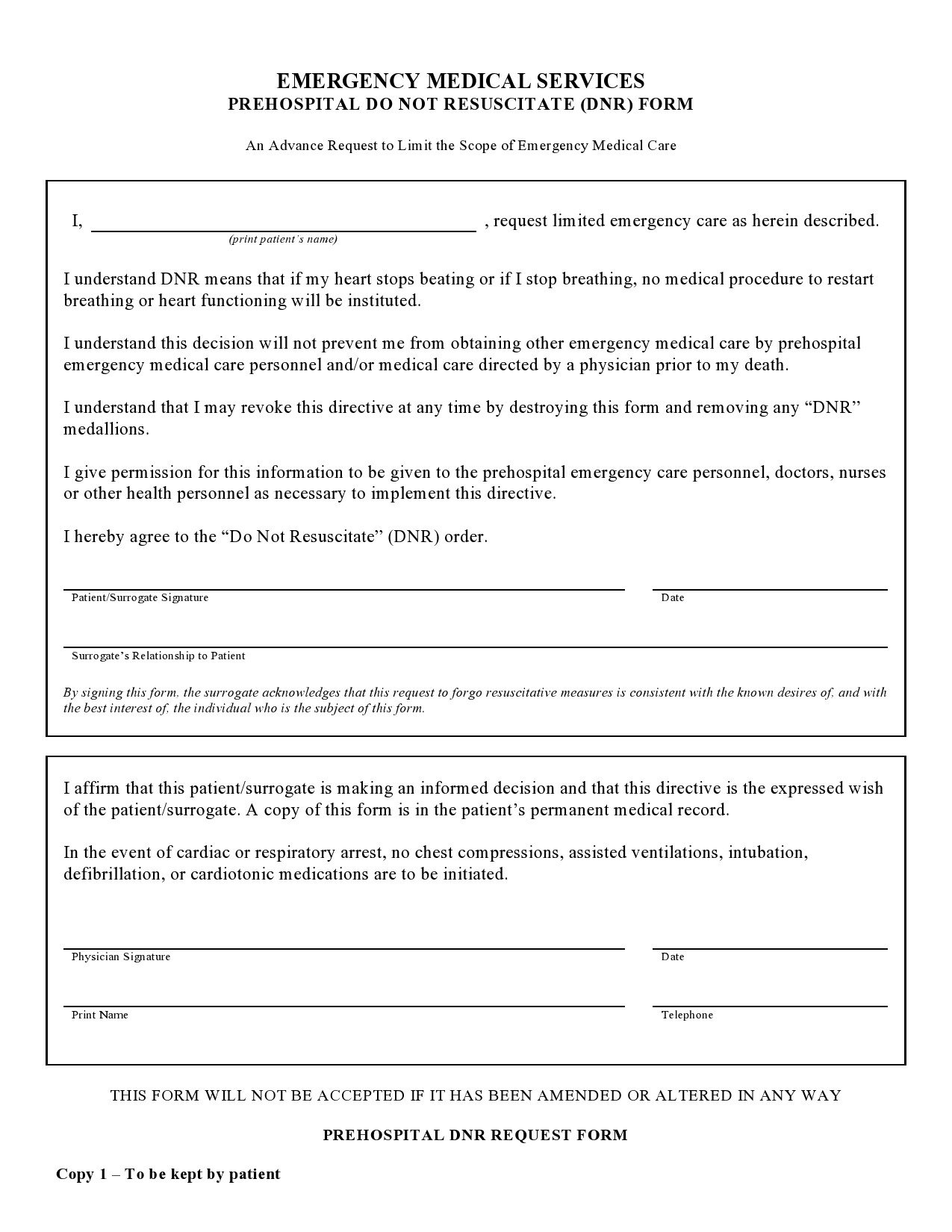
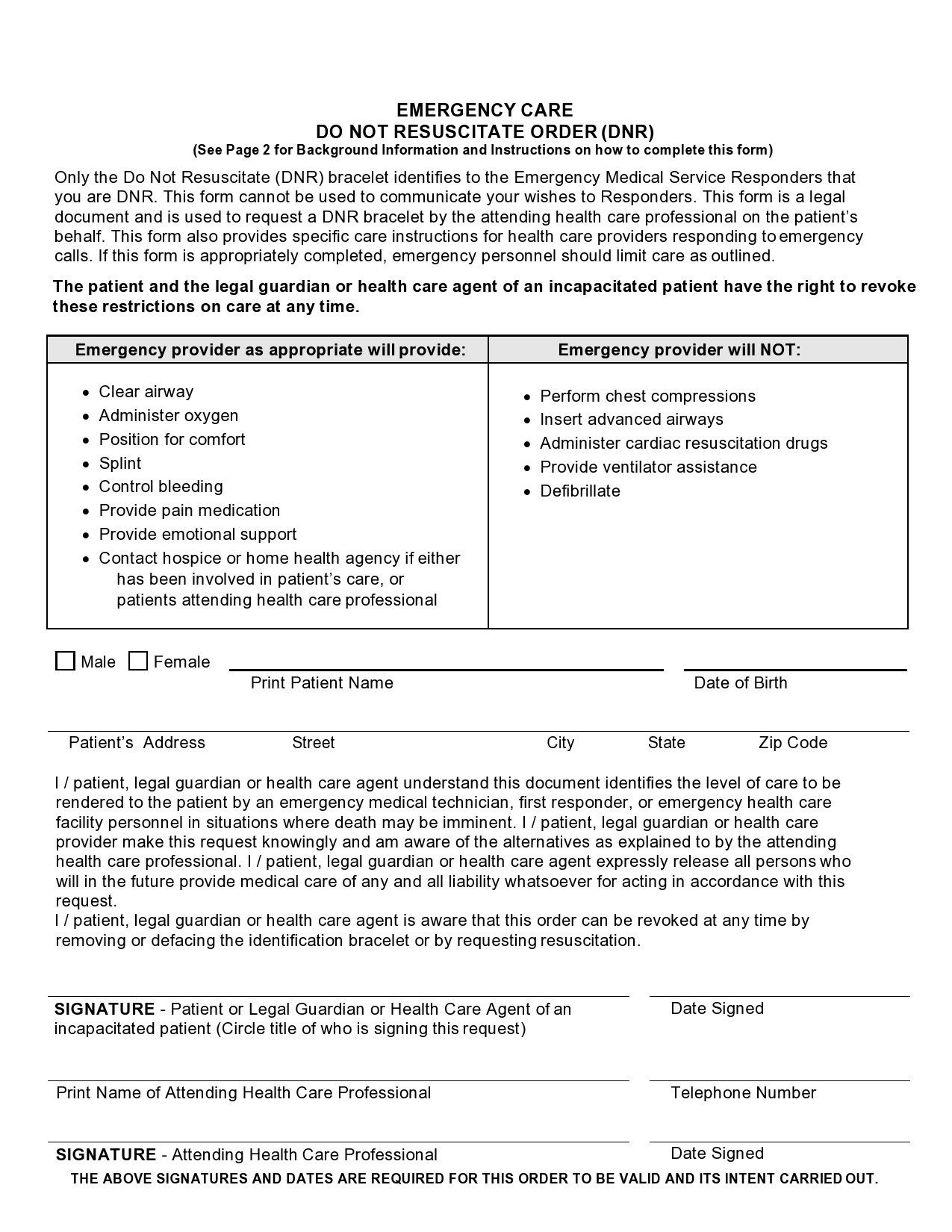
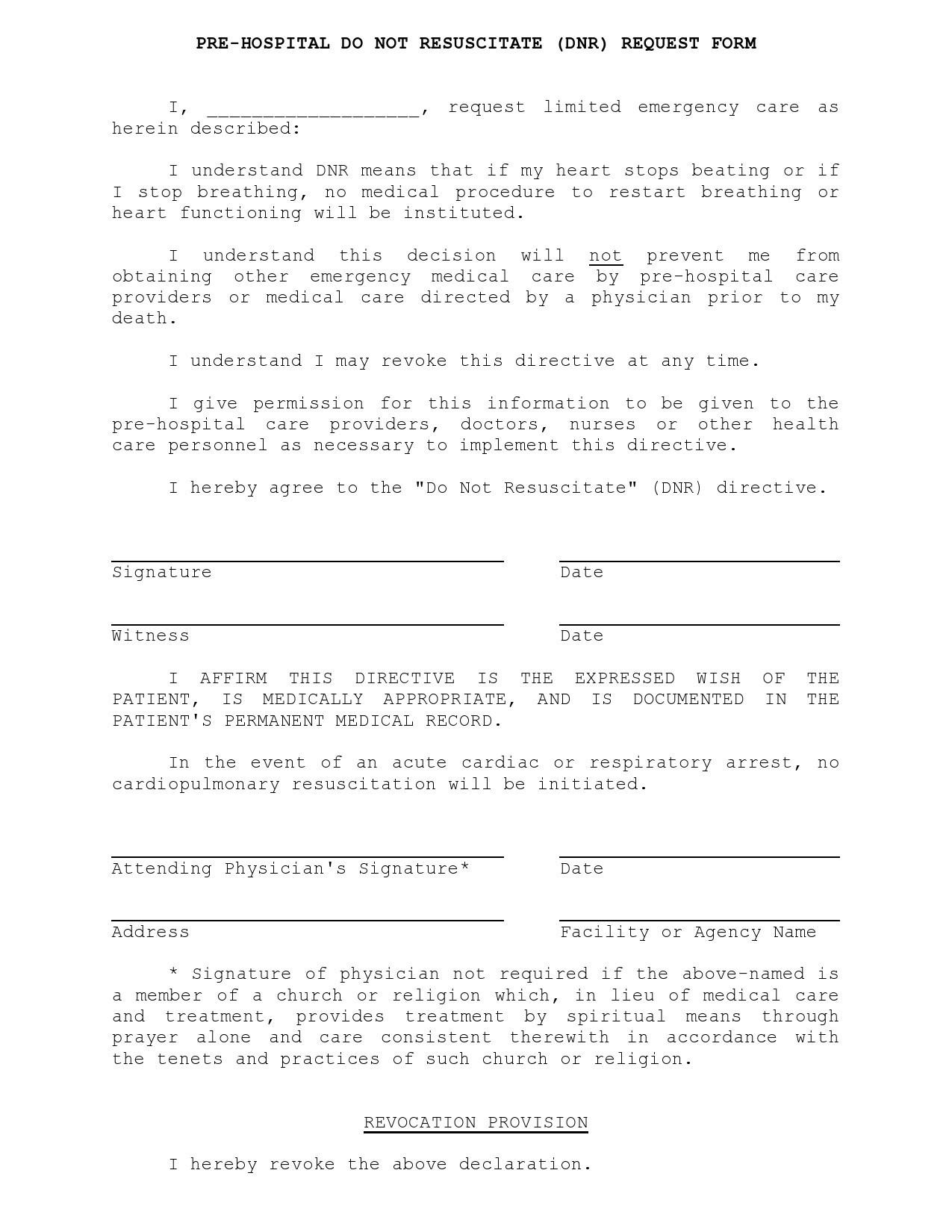
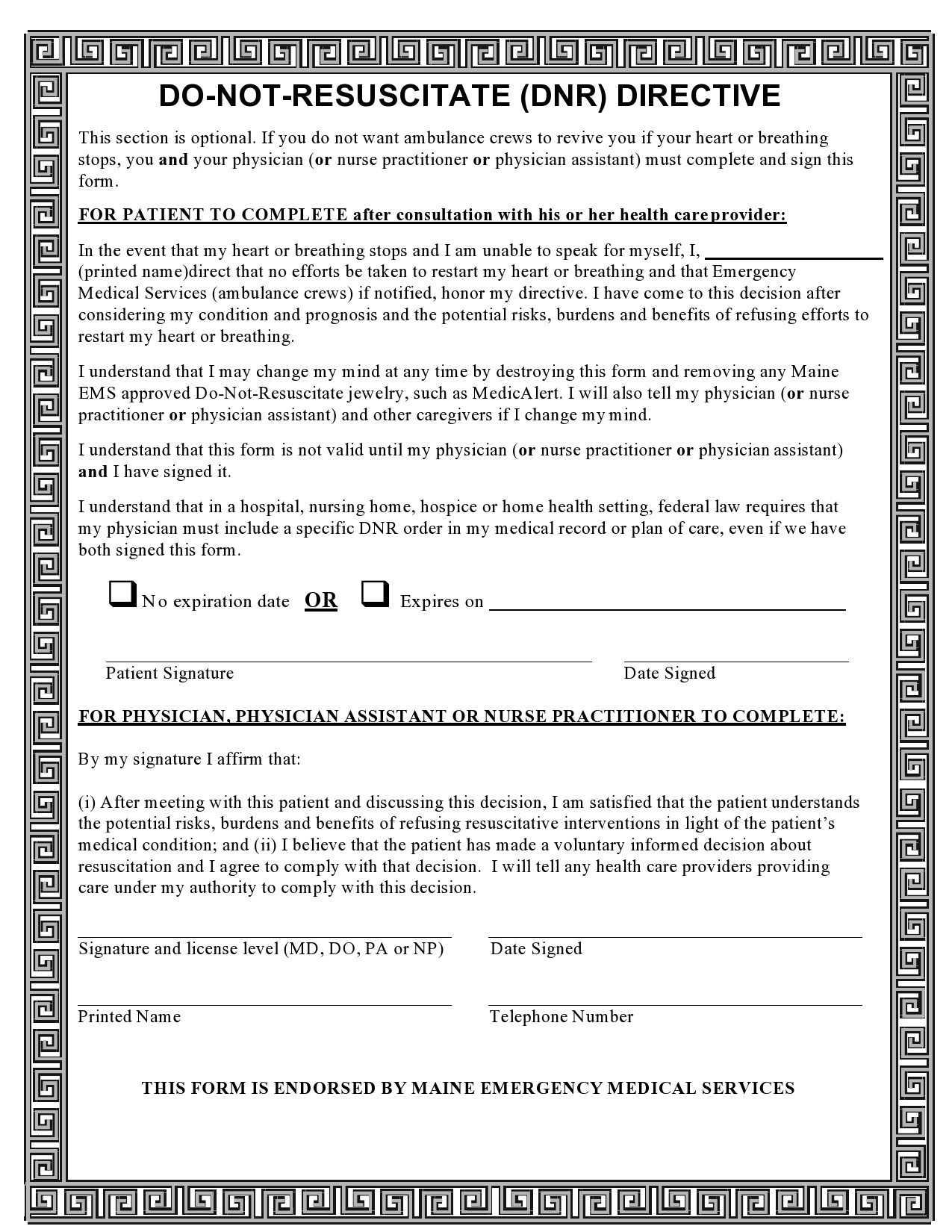
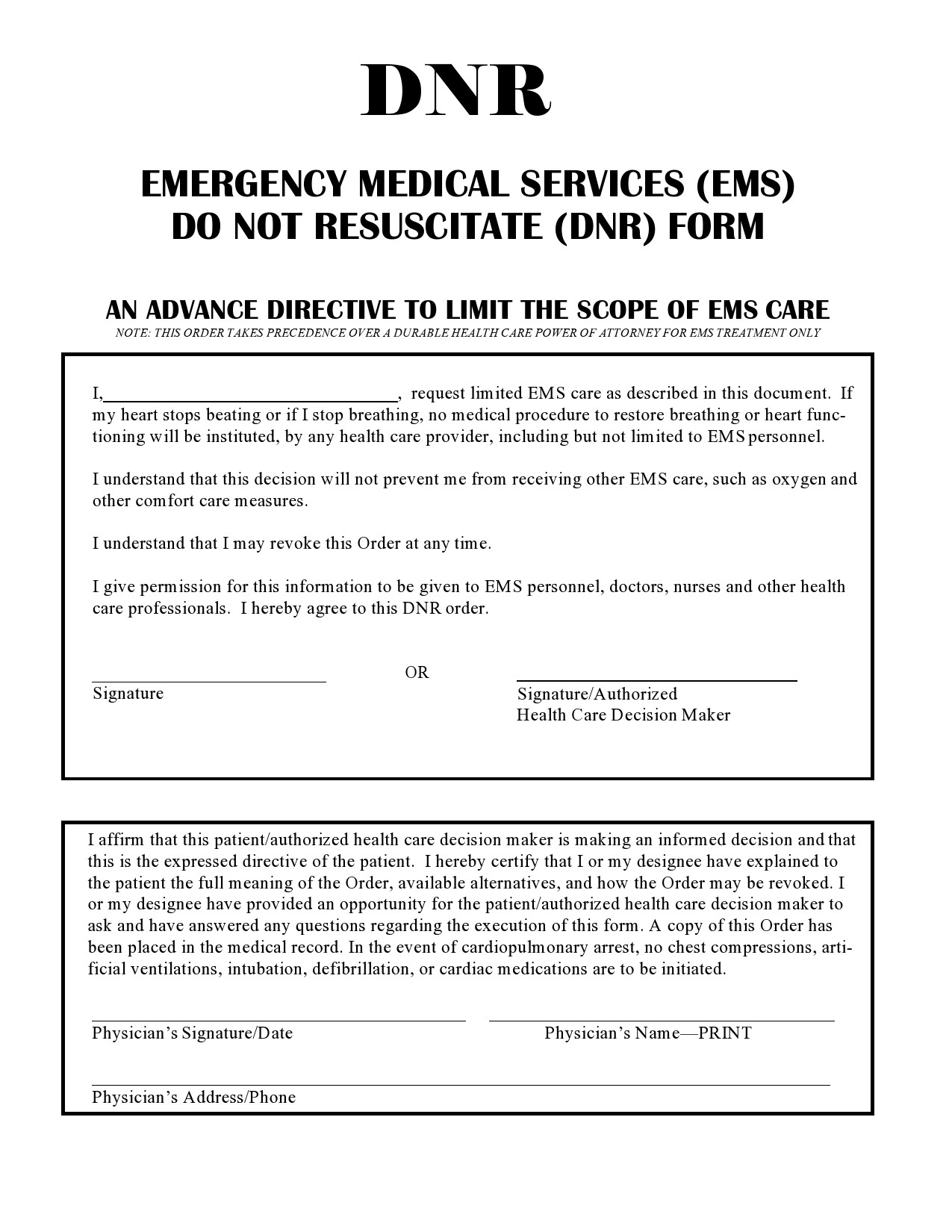
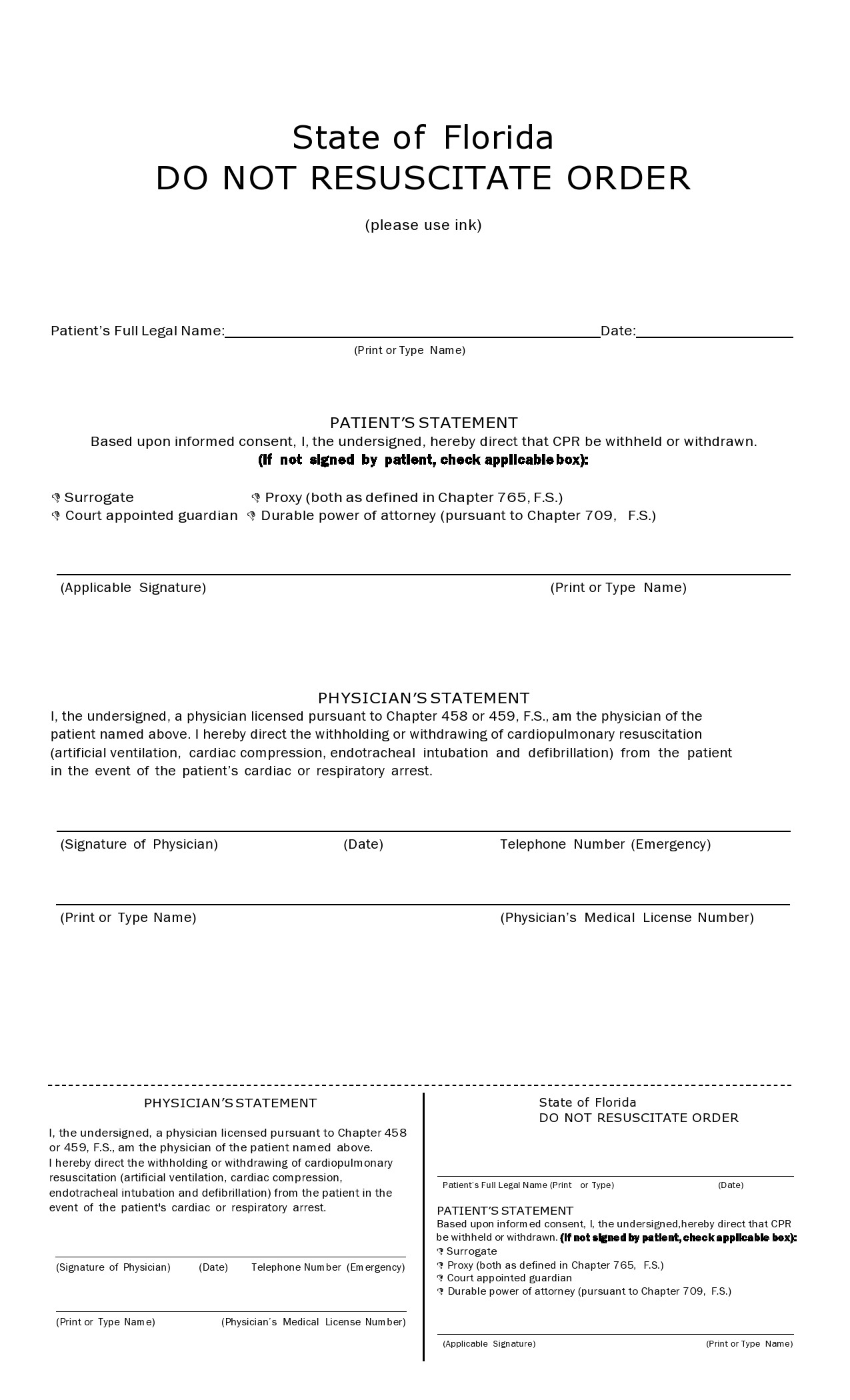
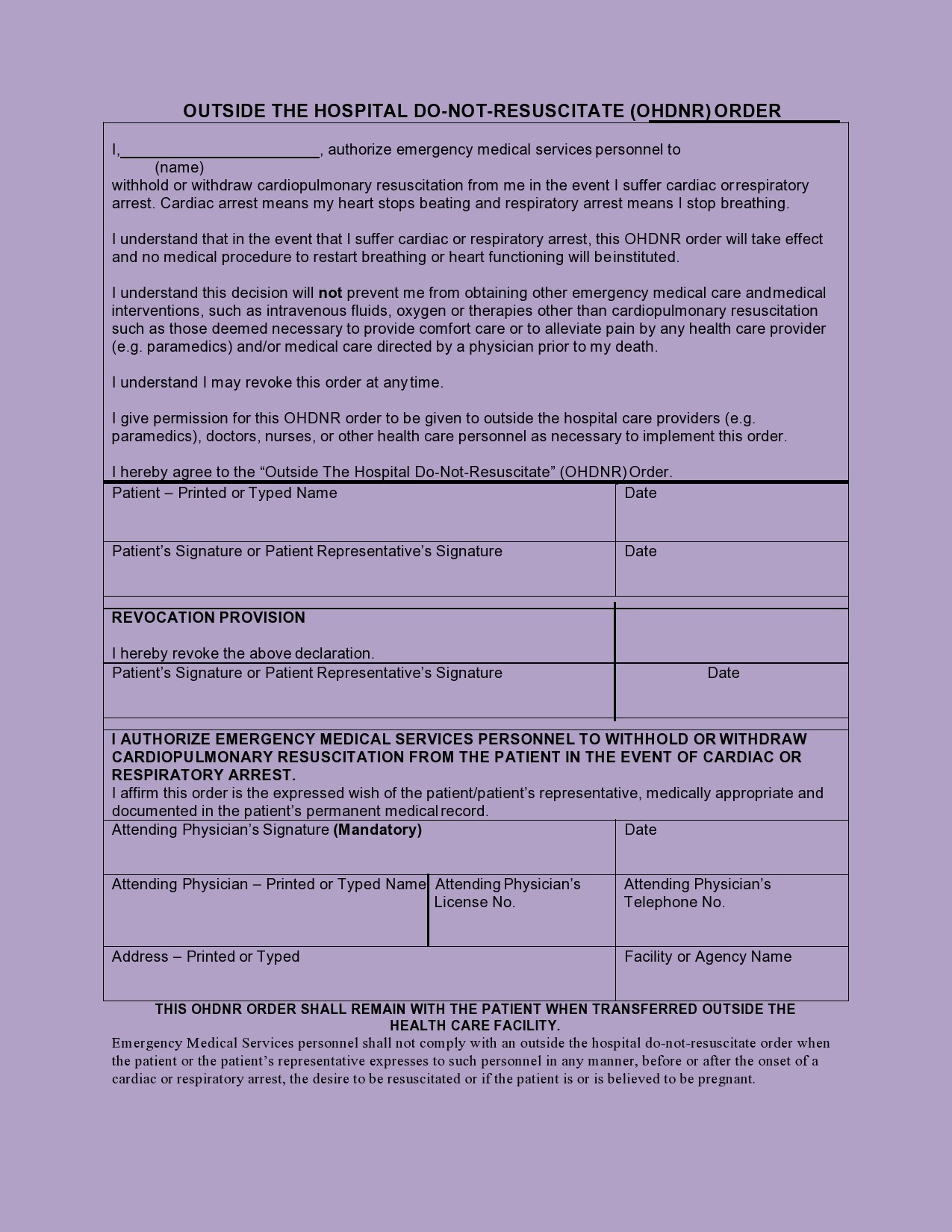
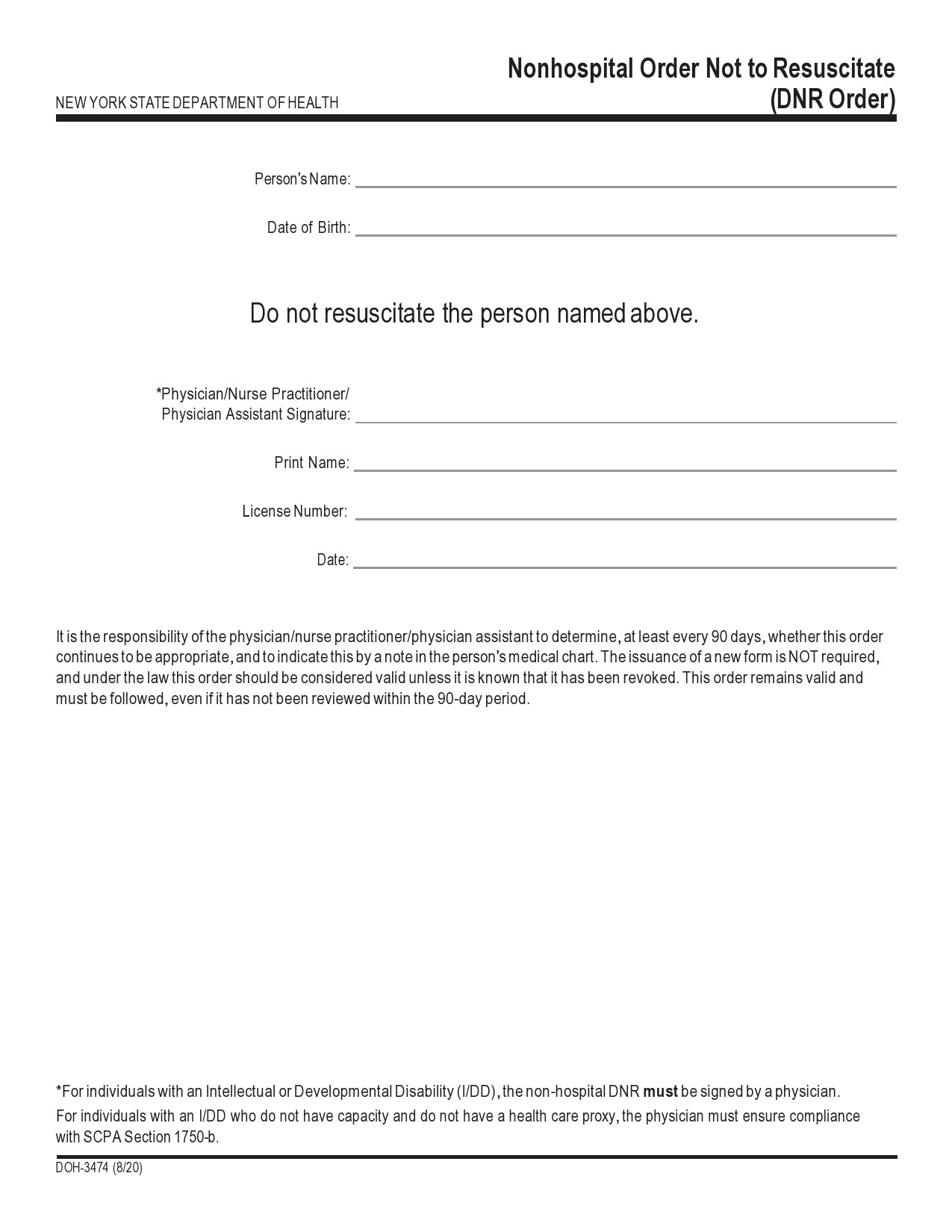
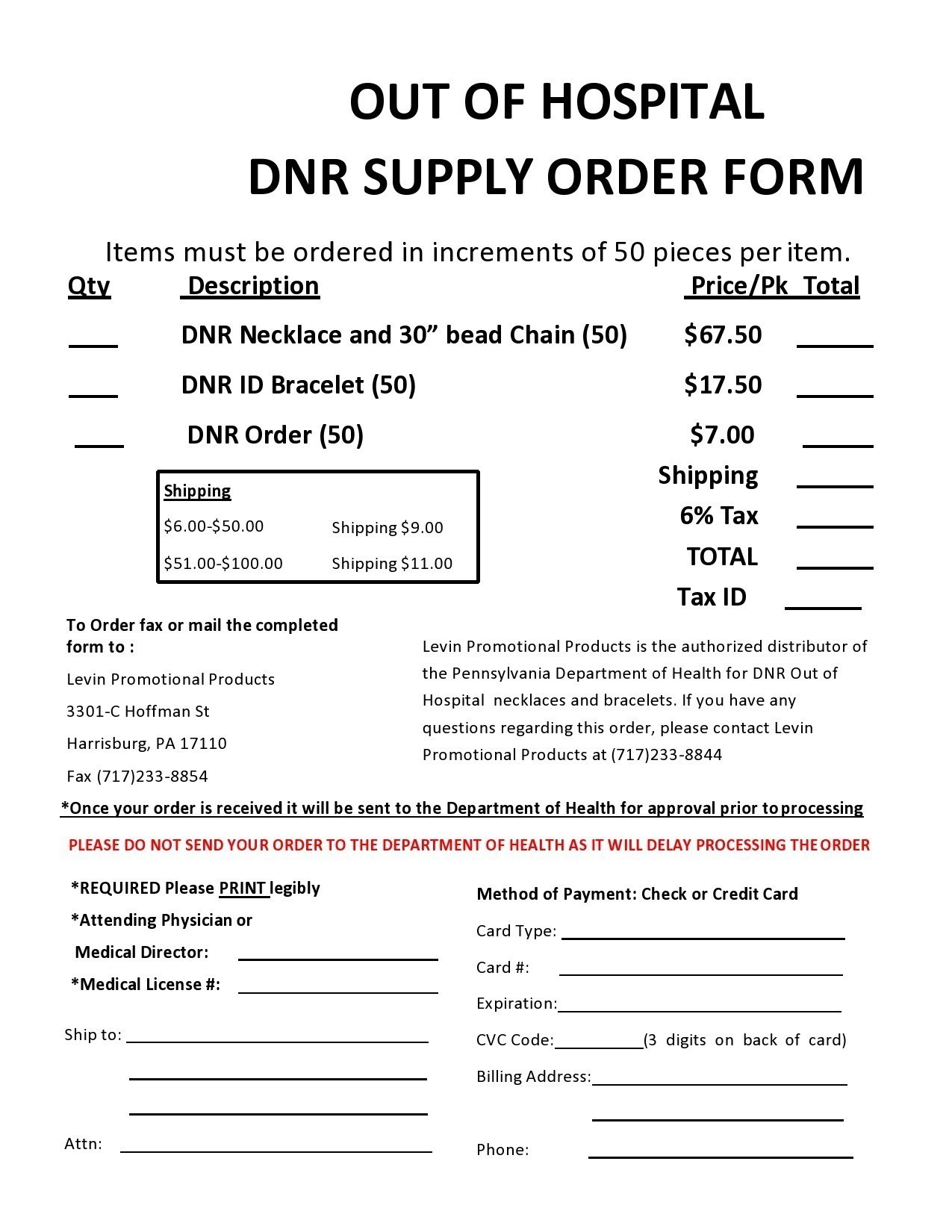
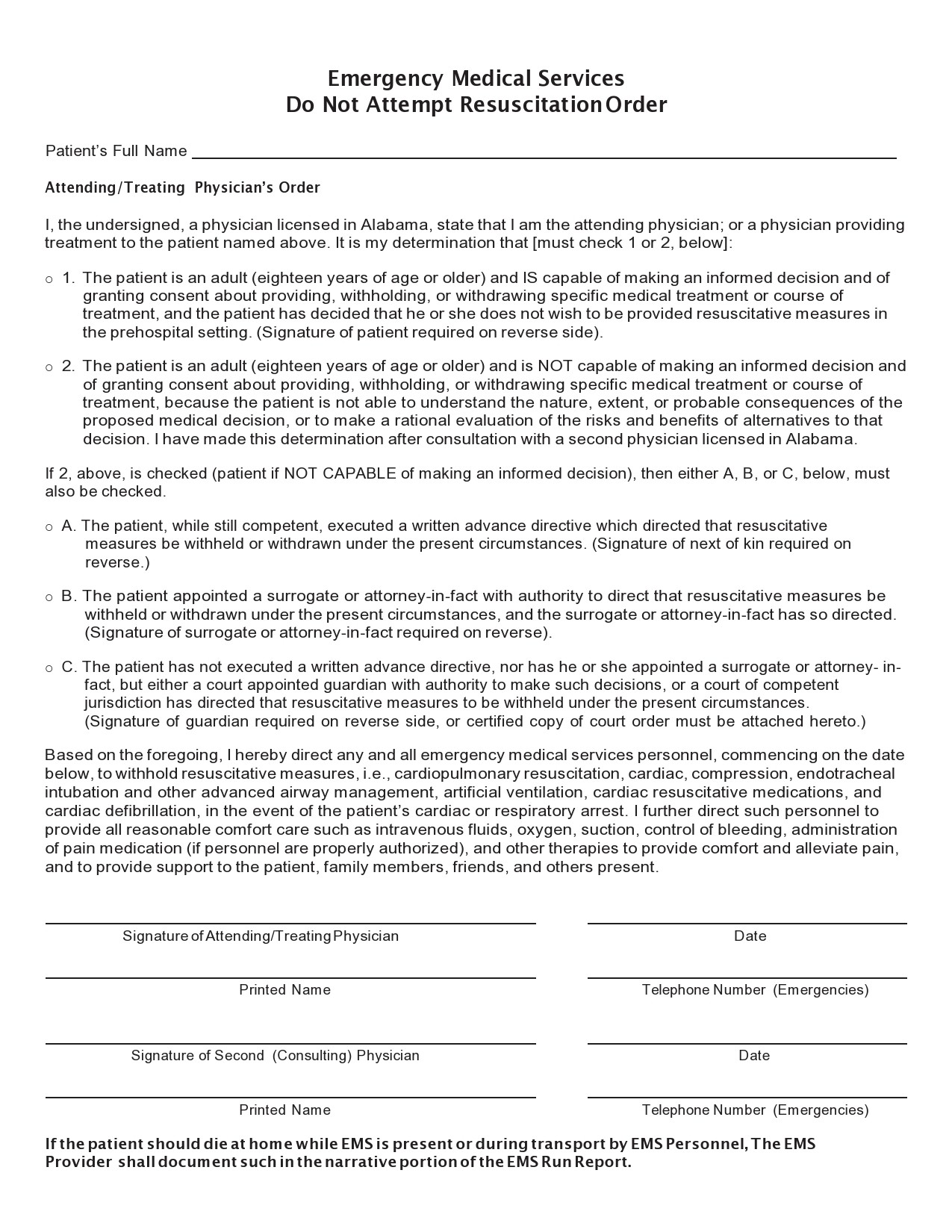
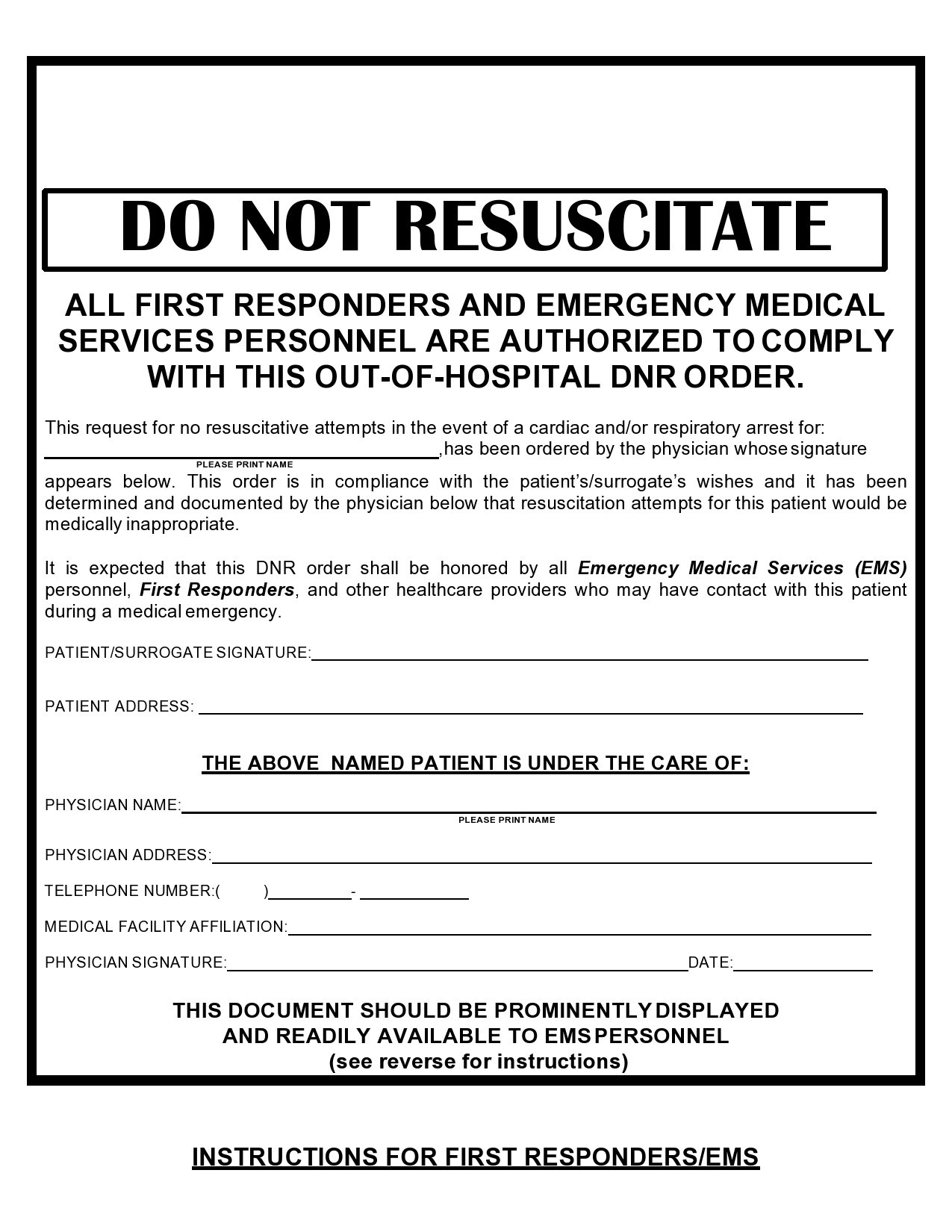
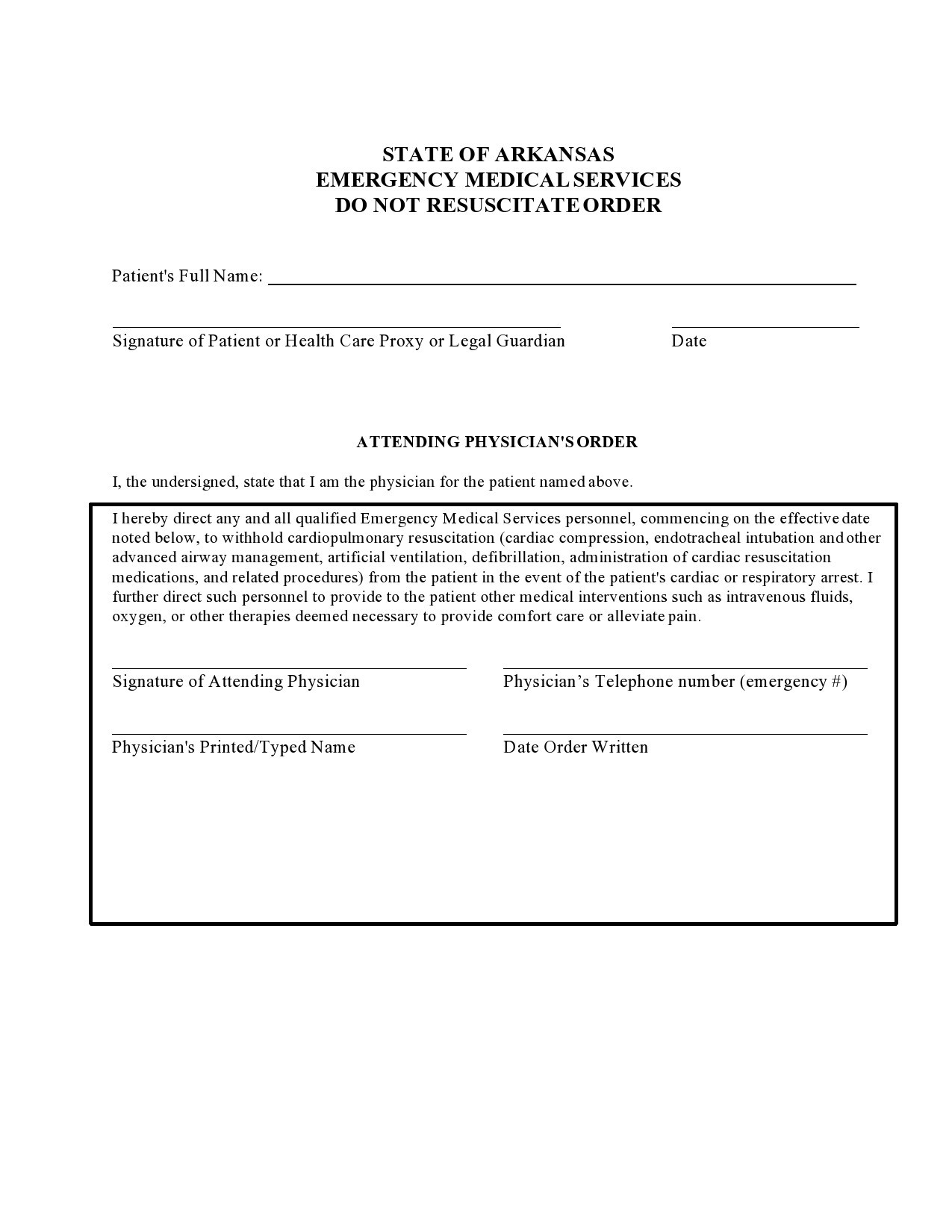
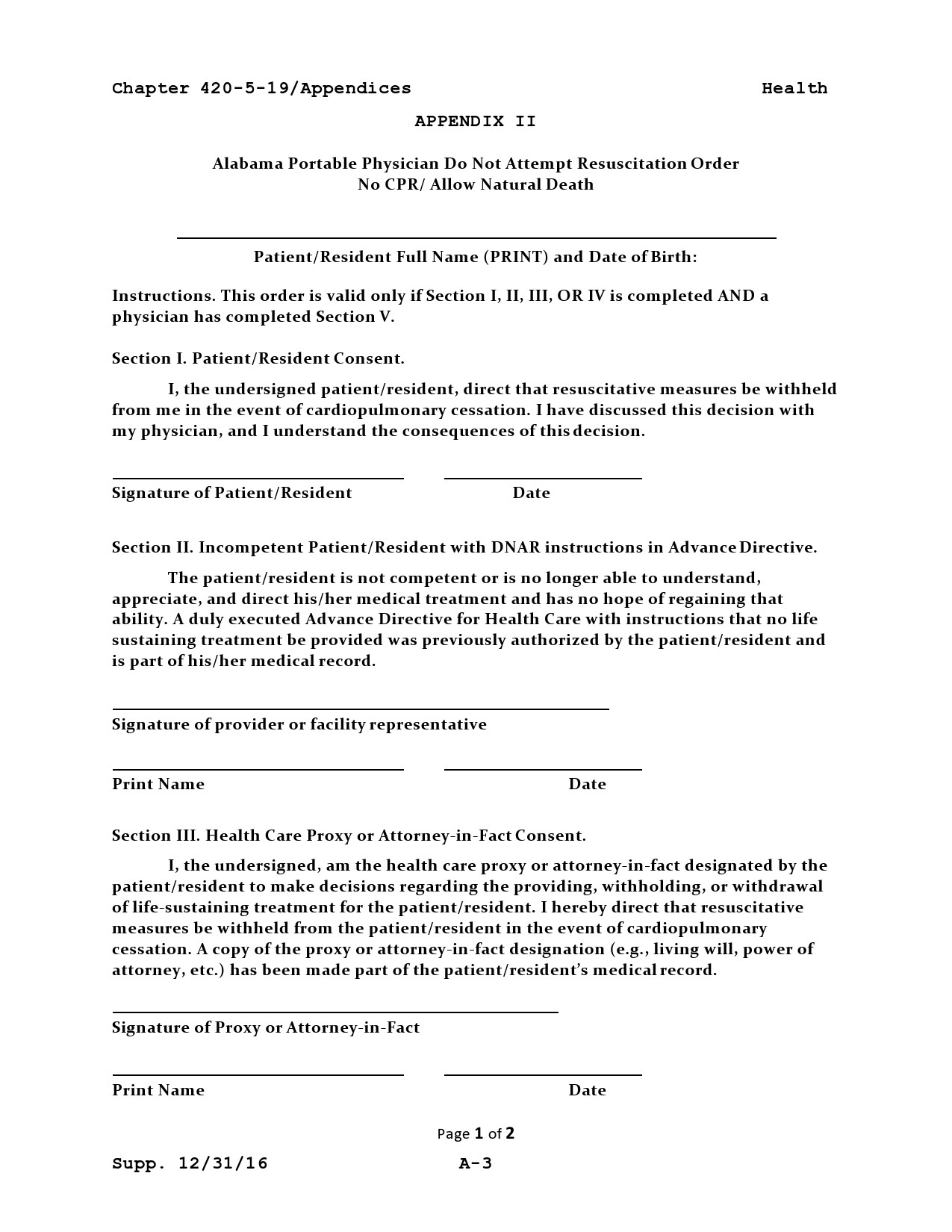
If you’re a patient admitted to a hospital, the doctors will attach your DNR to your chart. In emergency situations, you can opt for either a “pre-hospital” or “out of hospital” do not resuscitate form. This gives instructions to the emergency medical personnel to make no attempt for intubation or resuscitation.
You must be absolutely sure during this situation to keep your DNR visible so that the first responders will see it. Otherwise, they won’t know that you don’t want to get revived. The legal requirements regarding these forms vary in each state although generally, these forms are relatively simple to create and execute.
Still, you want to be absolutely certain that you are in compliance with the rules of your state. In most cases, these orders are one-page documents that you can include as part of advanced directives. You can also attach the form to your living will.
You can have great peace of mind if you have your DNR in place because you know you have expressed what you want for end-of-life treatment if the situation arises. It can also give you the chance to talk to your loved ones about these choices and where you keep your form. This will make them aware of your preferences and won’t try to go against your wishes.